The Association of Type 2 Diabetes Mellitus and Hyperglycemia With Subclinical Atherosclerosis in South Asian Adults
Quick Takes
- The risk of atherosclerotic cardiovascular disease is approximately twofold higher in South Asian (SA) adults than in other racial and ethnic groups, and type 2 diabetes mellitus (T2DM) is a strong contributor to this disparity.
- T2DM is associated with a higher likelihood of having a high coronary artery calcium (CAC) score in SA adults compared with the likelihood in adults from other racial and ethnic groups.
- CAC testing may be used to identify individuals with prediabetes and T2DM who are at higher risk.
Commentary based on Premyodhin N, Fan W, Arora M, et al. Association of diabetes with coronary artery calcium in South Asian adults and other race/ethnic groups: the multi-ethnic study of atherosclerosis and the mediators of atherosclerosis in South Asians living in America study. Diab Vasc Dis Res 2023;20:[ePub ahead of print].1
Background
The risk of atherosclerotic cardiovascular disease (ASCVD) is approximately twofold higher for South Asian (SA) adults than for adults from other racial and ethnic groups. Type 2 diabetes mellitus (T2DM) is a highly prevalent risk factor that likely contributes to this disparity.1,2 Measurement of coronary artery calcium (CAC) provides a direct, accurate, cost-effective, and personalized assessment of subclinical atherosclerotic burden. To date, the relative influence of T2DM on the development of CAC in SA adults compared with adults from other racial and ethnic groups has not been evaluated in well-characterized epidemiologic studies.
In this context, Premyodhin et al. explored the association of T2DM with CAC in SA adults, using data from the MASALA (Mediators of Atherosclerosis in South Asians Living in America) study compared with data from other racial and ethnic groups in the MESA (Multi-Ethnic Study of Atherosclerosis).1 Prediabetes was defined as fasting glucose level 100-125 mg/dL, and T2DM was defined as fasting plasma glucose level ≥126 mg/dL or use of insulin or oral diabetes mellitus (DM) medications. A T2DM diagnosis was associated with a higher likelihood of having CAC score >100 (a threshold at which statin initiation or intensification is recommended) among SA and Chinese adults compared with adults from other racial and ethnic groups. Furthermore, the slope of CAC score versus fasting glucose levels in a linear regression analysis was the steepest for SA adults, followed by Chinese adults and then by adults from other racial and ethnic groups. Above fasting glucose level 150 mg/dL, the mean CAC score was highest among SA adults. There was no association between prediabetes and CAC in any racial or ethnic group.1
Commentary
The findings of the present study build on evidence that SA adults with T2DM have a higher risk of subclinical atherosclerosis than do adults from other populations. These findings have important implications and contribute to clinical understanding of the relationship between T2DM and ASCVD in this population at higher risk. The mechanisms of heart disease linked to DM are complex, with hyperglycemia acting upon multiple pathways associated with oxidative stress, inflammation, and altered metabolic pathways, leading to atherosclerosis, myocardial fibrosis, and diabetic cardiomyopathy.3 Comorbid T2DM disproportionately increases levels of CAC in SA adults compared with levels in adults from other racial and ethnic groups.
There may be several explanations for the higher observed rates of subclinical atherosclerosis in SA adults with T2DM. A separate analysis of the MESA and MASALA data, which used clustering analysis, showed that the "severe hyperglycemia" subtype of T2DM was most common among SA adults, whereas adults from other racial and ethnic groups have T2DM characterized by older age and severe obesity.2 SA individuals had the highest hemoglobin A1c (HbA1c) and lowest beta cell function, consistent with other data demonstrating impaired beta cell function and worse insulin sensitivity in this population.4 Ectopic fat deposits in muscle, hepatic fat, and reduced beta cell function in SA adults has been hypothesized to underlie the unique pathophysiology of T2DM in this population.4 In addition to more severe T2DM, SA individuals may also have longer durations of T2DM, considering Asian Indian adults are diagnosed with T2DM approximately 5 years earlier (46 years of age; 95% confidence interval [CI], 43.9-48.5 years of age) than are non-Hispanic white adults (51 years of age; 95% CI, 50.4-51.9 years of age).5 Furthermore, there are rapid rates of progression from normal glucose tolerance to prediabetes and from prediabetes to T2DM, with a 32% rate of progression across glycemic categories in the MASALA cohort, supporting the need for frequent and repeat screening and for earlier lifestyle interventions for DM prevention.6
In light of stronger associations of T2DM and hyperglycemia with atherosclerosis in SA adults compared with those for adults from other racial and ethnic groups, an opportunity exists to capture risk beyond the binary variable of having DM or not. Current guidelines recommend testing using HbA1c or fasting blood glucose levels to screen for T2DM. Importantly, the American Diabetes Association (ADA) and US Preventive Services Task Force (USPSTF) recommend using body mass index (BMI) 23 kg/m2 as a threshold to screen for T2DM in Asian American individuals given the "metabolic obesity/normal BMI" phenotype prevalent in these populations.4
From a clinical standpoint, the role of CAC testing is reserved for those at borderline or intermediate ASCVD risk by the Pooled Cohort Equations (PCE) to help inform the use of preventive therapy (namely statins and aspirin).7 For SA adults at borderline and intermediate risk, the PCE overestimates ASCVD risk,8 potentially supporting the use of the CAC score to inform discussions about preventive therapy use. Similarly, not all patients with T2DM are at equal risk of a future ASCVD event. Indeed, the results of the MESA are consistent with those of other studies showing heterogeneity with respect to CAC score among those with T2DM: 46% of SA patients with prediabetes had any CAC (CAC score >0) and 72% with DM had any CAC (CAC score >0), representing individuals at higher risk who would benefit from statin therapy.9 Alternatively, among other racial and ethnic groups, adults with T2DM and CAC score of 0 (without ASCVD) remain at low short-term ASCVD risk. Nonetheless, the 2023 ADA guidelines and 2018 multisociety Guideline on the Management of Blood Cholesterol suggest the use of a moderate-intensity statin for all adults 40-75 years of age without established ASCVD.7 An expanded role for CAC testing in SA adults with T2DM may therefore guide the use of (sometimes costly) DM-specific therapy (sodium-glucose cotransporter-2 inhibitors or glucagon-like peptide-1 receptor agonists),10 motivate the use of aspirin (if CAC score >100), prioritize the use of more costly therapy such as proprotein convertase subtilisin/kexin type 9 inhibitors (conservative use if CAC score = 0), guide testing for lipoprotein(a) levels (elevated in roughly 25% of SA adults), and act as a catalyst to identify and intensify therapy for other traditional risk factors such as dyslipidemia and hypertension.4
Conclusion
SA individuals with T2DM have a higher prevalence of subclinical atherosclerosis than do individuals from other racial and ethnic groups (Figure 1). Clinicians should be aware that the risk of T2DM may be high despite a traditional BMI <25 kg/m2 in this population. The use of CAC testing in adults with prediabetes or T2DM may help identify a higher-risk phenotype that would benefit from aggressive lifestyle interventions and pharmacotherapy, when indicated.
Figure 1: Screening and Treatment of T2D
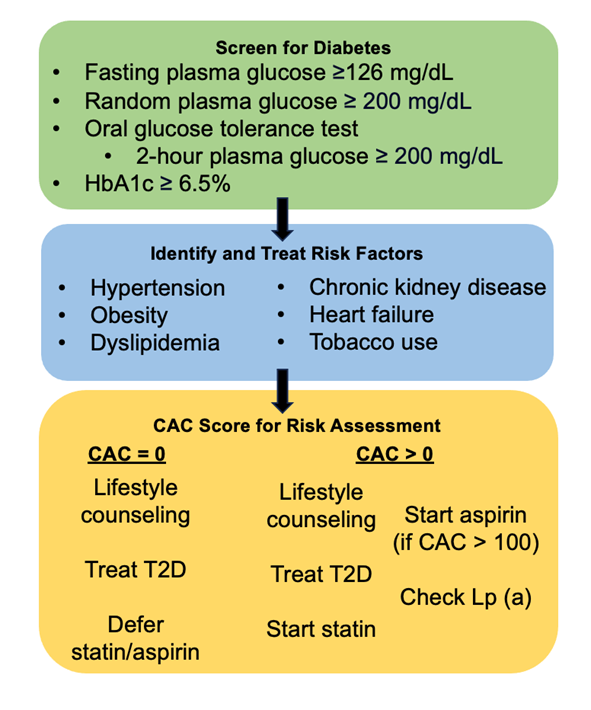
CAC = coronary artery calcium; HbA1c = hemoglobin A1c; Lp (a) = lipoprotein(a); T2D = type 2 diabetes mellitus.
References
- Premyodhin N, Fan W, Arora M, et al. Association of diabetes with coronary artery calcium in South Asian adults and other race/ethnic groups: the multi-ethnic study of atherosclerosis and the mediators of atherosclerosis in South Asians living in America study. Diab Vasc Dis Res 2023;20:[ePub ahead of print].
- Bancks MP, Bertoni AG, Carnethon M, et al. Association of diabetes subgroups with race/ethnicity, risk factor burden and complications: the MASALA and MESA studies. J Clin Endocrinol Metab 2021;106:e2106-e2115.
- Li Y, Liu Y, Liu S, et al. Diabetic vascular diseases: molecular mechanisms and therapeutic strategies. Signal Transduct Target Ther 2023;8:152.
- Agarwala A, Satish P, Al Rifai M, et al. Identification and management of atherosclerotic cardiovascular disease risk in South Asian populations in the U.S. JACC Adv 2023;2:[ePub ahead of print].
- Bhatt R, Ingle S, Sackpraseuth A, et al. Differences in the age of diagnosis of diabetes in Asian subgroups: analysis of data from the National Health Interview Survey (NHIS) 2006-2018. J Asian Health 2021;July 14:[ePub ahead of print].
- Gujral UP, Narayan KMV, Kandula NR, Liu K, Kanaya AM. Incidence of diabetes and prediabetes and predictors of glycemic change among South Asians in the USA: the MASALA study. BMJ Open Diabetes Res Care 2020;8:[ePub ahead of print].
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:e285-e350.
- Al Rifai M, Cainzos-Achirica M, Kanaya AM, et al. Discordance between 10-year cardiovascular risk estimates using the ACC/AHA 2013 estimator and coronary artery calcium in individuals from 5 racial/ethnic groups: comparing MASALA and MESA. Atherosclerosis 2018;279:122-9.
- Malik S, Zhao Y, Budoff M, et al. Coronary artery calcium score for long-term risk classification in individuals with type 2 diabetes and metabolic syndrome from the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol 2017;2:1332.
- Gan S, Dawed AY, Donnelly LA, et al. Efficacy of modern diabetes treatments DPP-4i, SGLT-2i, and GLP-1RA in white and Asian patients with diabetes: a systematic review and meta-analysis of randomized controlled trials. Diabetes Care 2020;43:1948-57.
Clinical Topics: Prevention, Noninvasive Imaging, Diabetes and Cardiometabolic Disease, Dyslipidemia
Keywords: Primary Prevention, Secondary Prevention, Calcium, Diabetes Mellitus, Type 2, Prediabetic State, Asia, Southeastern, Asian Continental Ancestry Group, Asian Americans