Poll: To Ablate Atrial Fibrillation or Not in the Older Adult? A Geriatric Cardiology/Electrophysiology Dilemma
Mr. PT is an 82-year-old man who presents with persistent, mildly symptomatic atrial fibrillation (AF) of approximately 4-5 months' duration. He also has New York Heart Association (NYHA) class II heart failure with reduced ejection fraction (EF) and left ventricular (LV) EF 40%.
Mr. PT has multiple chronic conditions. His noncardiac comorbidities include ophthalmic migraine, lumbar disk degeneration, spinal stenosis, osteoarthritis of the shoulder, umbilical hernia, history of adenomatous colonic polyps, obesity, history of opioid therapy, cough variant asthma, diabetes mellitus, chronic pain, restless leg syndrome, benign essential tremor, obstructive sleep apnea, osteoarthritis, and esophageal dyskinesia. His cardiac comorbidities include hypertension, hyperlipidemia, and atherosclerosis of the aorta. His most recent presentation was due to his persistent AF and systolic dysfunction.
History:
- Surgical history: Numerous, almost all involving the knees and musculoskeletal abnormalities of the spine
- Social history: Married with good social support, denies tobacco use, endorses rare alcohol use
Cardiovascular (CV) medications: 8
- Dabigatran etexilate 110 mg twice daily
- Losartan 50 mg daily
- Potassium chloride 10 mEq daily
- Metoprolol succinate 25 mg daily
- Spironolactone 25 mg daily
- Empagliflozin 12.5 mg daily
- Atorvastatin 40 mg daily
- Nitroglycerin sublingual as needed
Non-CV medications and supplements: 13
- Oxycodone/acetaminophen 10/325 mg twice daily as needed for pain
- Albuterol 90 mcg per actuation inhaler daily
- Pramipexole 1 mg daily
- Fluticasone/salmeterol 500/50 mcg per dose inhaler twice daily
- Senna 8.6 mg two tablets daily
- Docusate to 50 mg twice daily
- Acetaminophen 500 mg every 6 hours
- Oxymetazoline 0.05% two sprays twice daily
- Naloxone 4 mcg per actuation nasal spray as needed for suspected opioid overdose
- Beta-carotene/vitamin C/vitamin E/lutein supplement daily
- Flaxseed oil 300 mg daily
- Guaifenesin 1200 mg daily
- Multivitamin one tablet daily
Vital signs:
- Blood pressure 120/82 mm Hg
- Heart rate (HR) 105 bpm
- Weight 117.5 kg
- Body mass index 33.3 kg/m2
Physical examination findings:
- Constitutional: Conversant, well developed, no acute distress, alert and oriented x 3
- Eyes: Anicteric sclerae
- Neck: No gross abnormality, minimal jugular venous distention
- CV: Irregularly irregular rhythm; soft systolic murmur
- Pulmonary: Normal respiratory effort and rate, no cyanosis or audible wheeze/stridor
- Abdomen: Soft, nontender, nondistended, bowel sounds present no specific organomegaly
- Neurology: No focal abnormalities, patient ambulating without any significant abnormalities
- Psych: Intact judgment and insights
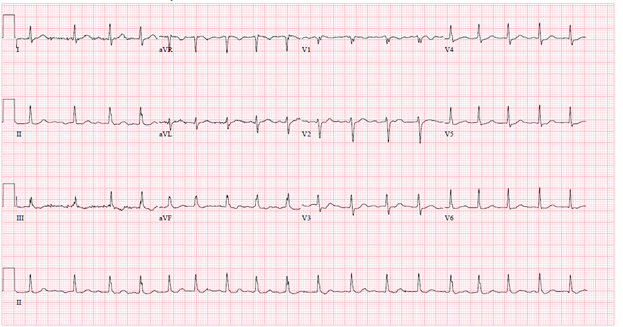
Electrocardiographic findings (Figure 1):
- AF
- HR 105 bpm
Figure 1
Echocardiographic findings:
- LV size is normal with end-diastolic dimension 5.2 cm
- EF 40%
- Right ventricle (RV): Moderately dilated, mildly reduced systolic function
- Left atrium (LA): Moderately dilated, LA volume index 30 mL/m2
- Right atrium: Moderately dilated
- Mitral valve: Mild mitral regurgitation
- Tricuspid valve: Mild tricuspid regurgitation, normal RV systolic pressure
- Pulmonary valve: Mild pulmonary regurgitation
In addition, a comprehensive geriatric assessment reveals the following:
The assessment demonstrates no abnormalities in sensory function (eyesight, hearing), normal nutrition, normal dentition, and no significant weight loss. He has experienced constipation (which is being treated) with no reports of bowel or bladder incontinence. He also has chronic pain and takes narcotics (noted earlier), with no other substance use. His wife aids him at home. He currently drives. He socializes with friends, neighbors, and his children over the holidays. He denies any substance abuse. There are no worries of elder abuse, and he has not had a fall in >2 years.
His Katz Index of Independence in Activities of Daily Living (ADLs) shows that he is independent in all his ADLs (bathing, toileting, walking/transferring, dressing, eating). His Lawton Instrumental ADLs scale demonstrates independence in telephone use, transportation, and managing his medications. He needs assistance with chores at home and chronically with managing money, which he does with his wife. His Nagi index of basic physical activities scale and Rosow-Breslau index of mobility scale results demonstrate that he needs assistance in pulling or pushing a large object, scooping, crouching, and kneeling. He is independent in lifting or carrying 4.5 kg, reaching his arms above his shoulders, writing, handling small objects, and walking up a flight of stairs. He needs complete assistance with walking a half-mile and doing heavy work around the house. He uses a cane as needed at home and outside. At present, he can walk 275 m at a slow pace without resting.
His Fried frailty phenotype results demonstrate borderline physical frailty. His cognitive assessment, performed using a Mini-Cog©, is normal with no current indications of delirium, anxiety, depression, or any other psychiatric conditions.
His predominant physical goal is to try to improve his exercise duration. His cognitive goal is to obtain an amateur (i.e., ham) radio license. He is a full code.
Clinical Topics: Arrhythmias and Clinical EP, Geriatric Cardiology, Atrial Fibrillation/Supraventricular Arrhythmias, Anticoagulation Management, Cardiovascular Care Team, Heart Failure and Cardiomyopathies
Keywords: Ablation, Geriatrics, Atrial Fibrillation