LDL Cholesterol Lowering: Is There a Risk for Dementia and Hemorrhagic Stroke?
Quick Takes
- US and international guidelines advocate for the achievement of very low levels of LDL-C, particularly for individuals at highest risk.
- The concerns about stroke and cognitive issues with very low LDL-C levels have been refuted.
- Studies have not demonstrated an increased risk of cognitive impairment, Alzheimer's dementia, or hemorrhagic stroke associated with lowering LDL-C levels.
Introduction
Reduction in low-density lipoprotein cholesterol (LDL-C) levels has consistently demonstrated a reduced risk of atherosclerotic cardiovascular disease (ASCVD). There is extensive evidence from randomized trials that demonstrates the effectiveness of lipid-lowering agents in reducing ASCVD-related events. Studies have demonstrated that the benefit is greatest for those who achieve both the lowest LDL-C and for longer periods. The results of recent clinical trials and meta-analyses, as summarized in the 2023 American Heart Association (AHA) scientific statement on Aggressive LDL-C Lowering and the Brain, have largely refuted concerns about heightened risk of hemorrhagic stroke (HS) and cognitive impairment/dementia. Clinicians should not be dissuaded from implementing more aggressive lipid-lowering regimens to optimally reduce risk of acute cardiovascular (CV) events.
Guidelines
Randomized controlled trials (RCTs) within the last decade have provided robust evidence that the addition of nonstatin therapies improves ASCVD outcomes proportional to the absolute LDL-C level attained, even at very low levels of LDL-C (e.g., <10 or 25 mg/dL). This relationship is consistent among patients with different comorbidities, including chronic kidney disease and diabetes mellitus, and across groups with different baseline LDL-C, age, sex, and CV risk profiles. In a prespecified analysis of the FOURIER (Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects With Elevated Risk) trial, the investigators examined 500 patients with achieved LDL-C level <10 mg/dL and found their event rate was reduced compared with that of patients at any greater LDL-C level.1
Recent cholesterol guideline iterations focus on distinct patient subgroups at higher risk that derive the greatest benefit from lower target and threshold LDL-C levels, above which the addition of a nonstatin therapy is warranted. The 2022 American College of Cardiology (ACC) Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-C Lowering in the Management of ASCVD Risk and the 2019 European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) Guidelines for the Management of Dyslipidaemias defined a patient group at very high risk for which the LDL-C target should be <55 mg/dL.2,3 Evidence from RCTs, complementing genomic and epidemiological findings, supports the use of statin and specific nonstatin therapies to improve CV outcomes. The paradigms are now lower is better and lowest is best. US and international guidelines advocate for the achievement of very low levels of LDL-C, particularly for individuals at highest risk.
Cognitive Impairment and Dementia
Lowering of LDL-C is not associated with cognitive decline or dementia. Although there have been concerns with pharmacological lowering of LDL-C levels with statins, these arose from the findings of smaller and confounded studies.1 Data from RCTs, including from the PROSPER (Prospective Study of Pravastatin in the Elderly at Risk) trial, did not show an increase in cognitive impairment with statin use.1 Similarly, participants in the EEBIHGAUS trial, with very low LDL-C (<25 mg/dL), did not show any harmful effect of LDL-C lowering on executive cognitive functioning and memory.
Elevated LDL-C is also considered a risk factor for neurodegenerative disease such as Alzheimer disease (AD). The etiology of this observation is unknown, especially because LDL particles do not cross the blood-brain barrier and may be linked to the onset of neuroinflammation. For the most part, the brain produces (via astrocytes and oligodendrocytes) and manages its own supply of cholesterol (Figure 1). In a post hoc analysis, PCSK9 inhibitor associated LDL-C cholesterol lowering showed no beneficial effect on formal objective cognitive testing results.4 This was true for even those participants with AD linked APOE4 allele. Thus, although there is a signal of association between LDL-C and AD, lowering the lipid levels systemically have also not translated into clinically meaningful reduction of AD.
Lipid Level Lowering and Hemorrhagic Stroke
Concern about low levels of serum cholesterol and risk of HS was first aroused by data from the MRFIT (Multiple Risk Factor Intervention trial), which suggested that total cholesterol level <160 mg/dL at baseline in men is associated with a twofold higher risk of HS compared with that of persons with levels >160 mg/dL. Since then, the results of several analyses (including RCTs and meta-analyses) suggested a small but nonsignificant association between statin therapy and risk of HS. Such an association is difficult to rationalize because it is known that statin therapy in no way weakens the architectural integrity of arterial walls making them more prone to rupture. Other hypotheses included a role for antithrombotic and anticoagulatory effects exerted by statins.
Two studies performed with atorvastatin therapy and with adequate power to evaluate a possible association had negative findings: the SPARCL (Stroke Prevention by Aggressive Reduction of Cholesterol Levels) and the TST (Treat Stroke to Target) trials. There was no association between the magnitude of LDL-C reduction or statin therapy per se and increased risk of HS. In the SPARCL trial, the two covariates that did suggest elevated risk of HS were poorly controlled hypertension (HTN) and a history of an HS. In the TST trial, poorly controlled HTN and use of anticoagulant therapy correlated with increased risk of HS, but LDL-C level <70 mg/dL did not. More recently, results from CV outcomes trials evaluating the efficacy of proprotein convertase subtilisin/kexin type 9 monoclonal antibodies (PCSK9 mabs; evolocumab and alirocumab) did not demonstrate any association between aggressive LDL-C lowering (even to <20 mg/dL) and a heightened signal for HS. The hazard ratios for HS (PCSK9 mab plus statin vs. statin monotherapy) in the FOURIER trial was 1.16 (95% confidence interval [CI], 0.68-1.980 and in the ODYSSEY OUTCOMES (Evaluation of Cardiovascular Outcomes After an Acute Coronary Syndrome During Treatment With Alirocumab) trial was 0.83 (95% CI, 0.42-1.65).
Consistent with the results of the aforementioned studies, the results of a comprehensive meta-analysis have shown that lowering LDL-C level to <55 mg/dL (consistent with current guideline recommendations for patients at very high risk) compared with LDL-C levels above this threshold does not increase risk of HS (OR, 1.05; 95% CI, 0.85-1.31).5 Of considerable interest is a Danish population-based investigation, which included 16,235 patients with HS and 640,943 control patients. Current statin use and a longer period of current statin use (<1 year: OR, 0.86 [95% CI, 0.81-0.92]; ≥1 to <5 years: OR, 0.72 [95% CI, 0.68-0.76]; ≥5 to <10 years: OR, 0.65 [95% CI, 0.6-0.71]; ≥10 years: OR, 0.53 [95% CI, 0.45-0.62]; ptrend < 0.001) correlated with a lower risk of HS.6 There is no evidence from randomized trials or Mendelian inheritance studies that genetically low LDL-C augments risk of HS. Consistent with these findings, the 2023 AHA scientific statement on LDL-C lowering emphasized that "concern about hemorrhagic stroke risk should not deter a clinician from treating LDL-C to guideline-recommended risk-stratified targets."1
Figure 1: A Comparison of Transport of LDL-C in the Brain vs. the Peripheral Circulation
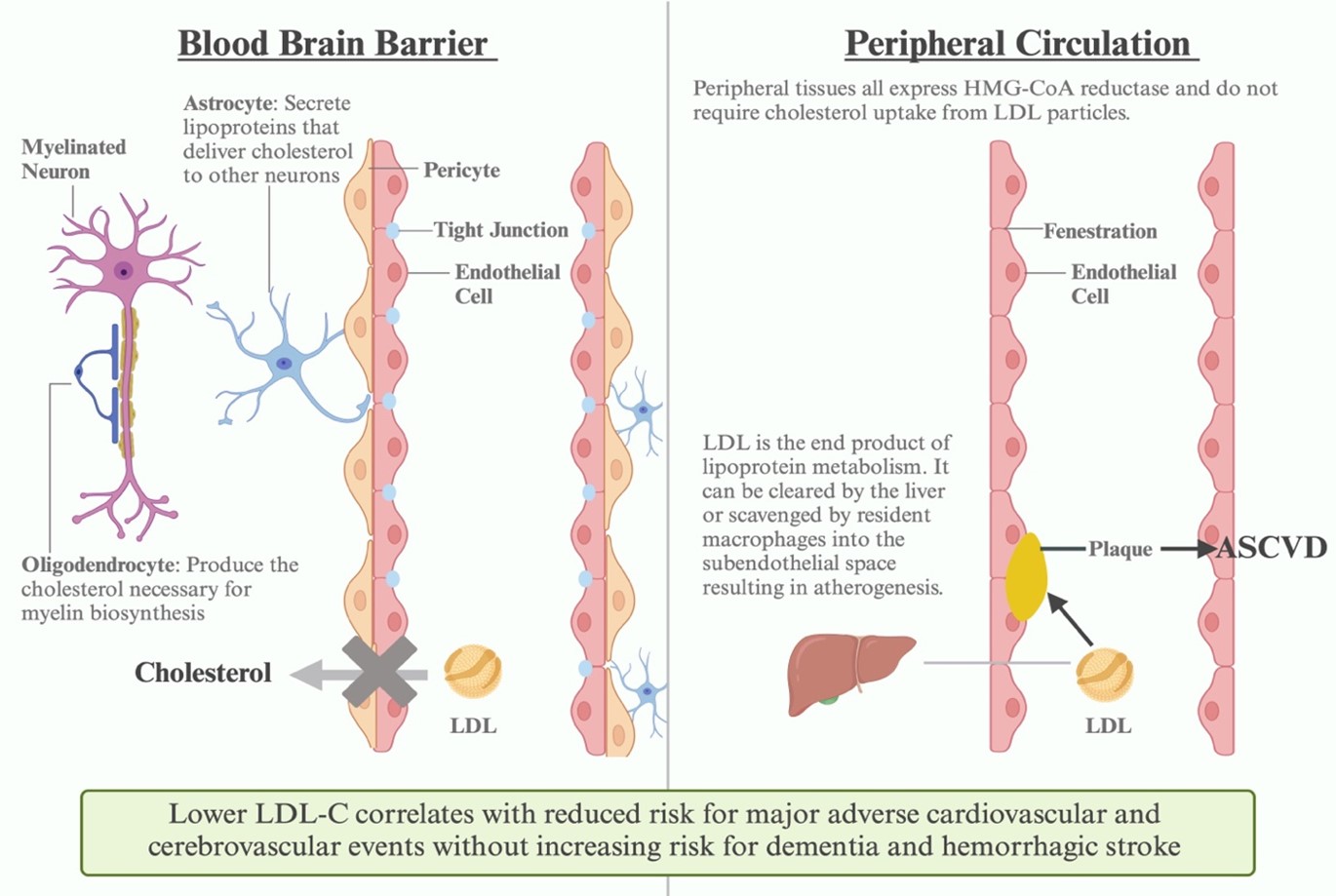
LCL-C = low-density lipoprotein cholesterol.
References
- Goldstein LB, Toth PP, Dearborn-Tomazos JL, et al.; American Heart Association Council on Arteriosclerosis, Thrombosis and Vascular Biology, Council on Cardiovascular and Stroke Nursing, Council on Peripheral Vascular Disease, Stroke Council. Aggressive LDL-C lowering and the brain: impact on risk for dementia and hemorrhagic stroke: a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol 2023;43:e404-e442.
- Lloyd-Jones DM, Morris PB, Ballantyne CM, et al.; Writing Committee. 2022 ACC expert consensus decision pathway on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol 2022;80:1366-418.
- Mach F, Baigent C, Catapano AL, et al.; ESC Scientific Document Group. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41:111-88.
- Korthauer LE, Giugliano RP, Guo J, et al. No association between APOE genotype and lipid lowering with cognitive function in a randomized controlled trial of evolocumab. PLoS One 2022;17:[ePub ahead of print].
- Masson W, Lobo M, Siniawski D, Masson G, Lavalle-Cobo A, Molinero G. LDL-C levels below 55 mg/dl and risk of hemorrhagic stroke: a meta-analysis. J Stroke Cerebrovasc Dis 2021;30:[ePub ahead of print].
- Rudolph DA, Hald SM, García Rodríguez LA, et al. Association of long-term statin use with the risk of intracerebral hemorrhage: a Danish nationwide case-control study. Neurology 2022;99:e711-e719.
Clinical Topics: Dyslipidemia, Prevention, Vascular Medicine, Lipid Metabolism, Nonstatins, Sleep Apnea
Keywords: Cholesterol, LDL, Hemorrhagic Stroke, Cognitive Dysfunction, Dementia, Primary Prevention