Frozen Frontiers: Understanding Cardiovascular Dynamics in Winter Sport Athletes
Quick Takes
- Athletes face unique cardiovascular challenges when participating in winter sports, primarily related to environmental factors, including cold temperatures and altitude-associated hypobaric hypoxia and their impact on the cardiovascular system.
- At the competitive or elite level, medical staff should be well-versed in common cardiac conditions associated with participation in winter sports for appropriate counseling, prevention, and treatment of cardiovascular conditions in this population.
- More research is needed to understand sport-specific cardiac remodeling as it relates to the winter athlete's heart.
Introduction
Interest and research in exercise science is growing, though winter sports are underrepresented.1 Much of the existing research on winter sports is focused on injuries. Less has been written about the cardiovascular stressors, adaptations, and implications of participation in winter sports.1 In addition, winter sport popularity is rising in the aftermath of the coronavirus disease 2019 pandemic. Across the 2022-2023 season, an estimated 29.9 million individuals engaged in winter sports in the United States, up from 25 million in prior years.2 Ski mountaineering is one sport driving this increase, partially due to its inclusion in the 2026 Olympic Winter Games. Ski mountaineering imposes significant demand on the cardiovascular system due to environmental extremes such as high-altitude uphill skiing and descents on unprepared slopes.3 As more individuals engage in winter athletic pursuits, particularly recreational and master athletes, medical professionals will play a role in patient risk stratification and treatment.
In this review, considerations for the cardiovascular care of winter athletes are identified. Several aspects of the environment that impact cardiovascular function, including ambient temperature and altitude, are focused on. The main cardiovascular adaptations in response to these conditions are described. Finally, the clinical implications of these observations are reviewed, and areas of future research are proposed.
Temperature
Prior studies have demonstrated an inverse relationship between ambient temperature and acute coronary syndrome.4 Several mechanisms have been proposed, including an increase in circulating catecholamines in response to cutaneous thermoreceptor activation. This catecholamine surge leads to peripheral vasoconstriction and increased heart rate, resulting in increased blood pressure, left ventricular end-diastolic pressure and volume, and ultimately increased cardiac workload and myocardial oxygen demand.4 Coronary artery spasm may occur if arterial vasoconstriction involves the coronary vessels, resulting in anginal symptoms.5
Endothelial dysfunction has also been proposed to explain increased cardiovascular events in cold weather. Lower brachial artery flow-mediated dilation in winter may suggest that microvascular vasodilator function is impaired by cold temperature.5 Sudden cardiac death during winter may be associated with arrhythmias or with abrupt coronary plaque rupture related to changes in blood pressure and hemostasis.4 Finally, cold weather likely exhibits negative effects on hemostasis and inflammation, demonstrated by a greater tendency to form clots in the peripheral circulation.6 While these changes are likely less significant for athletes without underlying coronary artery disease (CAD), those with a diagnosis of atherosclerotic CAD may have reduced performance or be at increased risk of ischemia.
Altitude
Many winter sports take place at elevation, which significantly impacts cardiovascular physiology due to hypobaric hypoxia. Acute exposure to altitude results in increased sympathetic tone, leading to increased heart rate, blood pressure, and cardiac output. This may aggravate pre-existing arrhythmias.7 Individuals with hypertension have a variable response to altitude, though increases in systolic blood pressure of 30-40 mm Hg above baseline are rare and transient, typically resolving with descent below 3000 m.7 Short-term altitude exposure has also been proposed as an independent risk factor for hypercoagulability.6 Finally, athletes who ascend to high altitude may develop associated illnesses, including acute mountain sickness, high altitude pulmonary edema, and high altitude cerebral edema.7
Chronic altitude exposure can be beneficial to athletic performance, primarily through hypoxemia-induced polycythemia and resultant increase in oxygen carrying capacity.8 Altitude training may therefore be advantageous to endurance athletes' performance in the long-term. Strategies to mitigate short-term effects of altitude on performance include slow ascent, adequate hydration, pharmacologic prophylaxis, and simulated altitude training prior to competition.9
The Winter Athlete's Heart
Structural, physiological, and electrophysiological adaptations to exercise training have been collectively termed the "athlete's heart" (Figure 1). These changes can be observed with diagnostic testing (electrocardiography), cardiac imaging (echocardiography and cardiac magnetic resonance imaging), and exercise performance evaluation by cardiopulmonary exercise testing (CPET). As with all athletes, sport-specific backgrounds and training patterns must be considered when evaluating the winter athlete's heart. For example, Zimmerman et al. (2022) demonstrated sport-specific adaptation patterns when comparing cardiac physiologic changes between ski mountaineering, Nordic-cross country, and biathlon athletes.10 Differences in left atrial volume index, left ventricle global longitudinal strain, and left ventricle mass index were noted between disciplines. While all athletes had excellent aerobic capacity by CPET, there were significant differences between maximum respiratory minute volume and maximum oxygen pulse level between ski mountaineering and the Nordic and biathlon athletes. Thus, there are likely sport-specific and dynamic cardiac remodeling patterns distinct to winter athletes.
Figure 1: Overview of the Winter Athlete's Heart
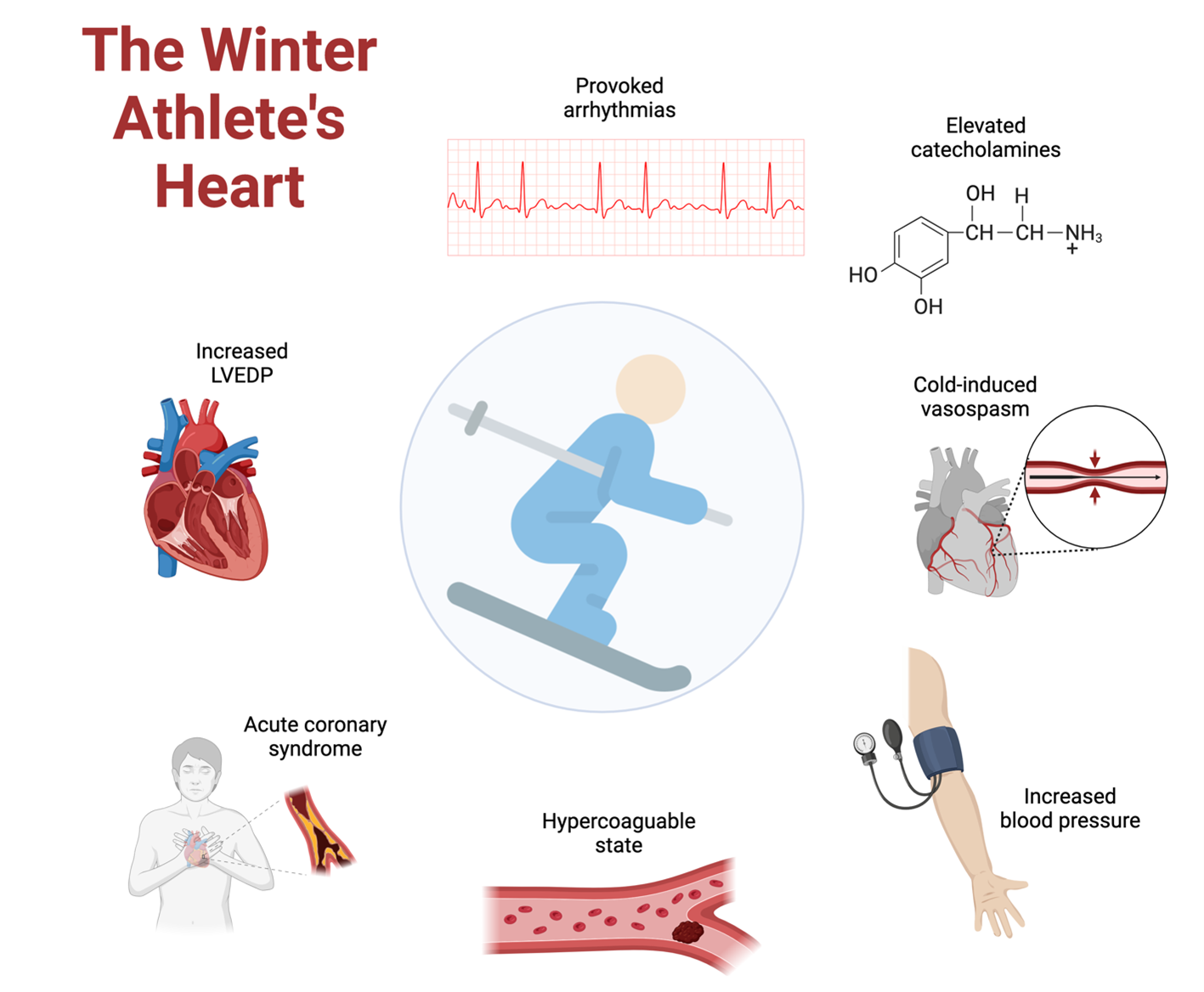
LVEDP = left ventricular end-diastolic pressure.
Clinical Implications
Clinical guidance for winter athletes is most relevant for those at risk of, or living with, established cardiovascular disease. Exposure to cold, and subsequent peripheral and coronary arterial vasoconstriction, can be deleterious to patients with a history of ischemic heart disease. Winter athletes at risk may benefit from cardiovascular risk assessment prior to engaging in high-intensity winter sports, though the utility of universal cardiac assessment is likely low. Patients with a history of coronary vasospasm may consider discussing treatment options with their healthcare provider. Athletes with pre-existing arrhythmias would benefit from a discussion regarding the risk of provoking symptoms when engaging in winter sport.
Athletes with hypertension should be educated regarding the impact of participation in cold weather sports and activities at high altitude. Athletes may continue antihypertensives as prescribed, though there is no consensus on treating athletes whose hypertension worsens at altitude. Several experts suggest using nocturnal oxygen for individuals with labile or resistant hypertension exercising in this environment.8
In addition to gradual ascent, pharmacological prophylaxis can be considered to help prevent altitude-associated illnesses. Prophylaxis options include acetazolamide, dexamethasone, nifedipine, phosphodiesterase-5 inhibitors, and salmeterol.9 Notably, data on the effectiveness of agents other than acetazolamide are limited. Cardiologists caring for individuals training and competing at high altitude should review recent expert consensus statements and consider collaboration with primary care sports medicine practitioners to individualize treatment plans.
Conclusion
Winter athletes face cardiovascular challenges, primarily related to cold temperatures and altitude-associated hypobaric hypoxia. It is important to discuss individual participation risks with athletes who have pre-existing cardiovascular conditions. At the elite level, medical staff should be well-versed in common pathologies associated with participation in winter sports. More research is needed to understand sport-specific cardiac remodeling as it pertains to the winter athlete's heart.
References
- Millet GP, Brocherie F, Burtscher J. Olympic sports science-bibliometric analysis of all summer and winter olympic sports research. Front Sports Act Living 2021;3:772140.
- Shop Eat Surf. SIA Releases 2022-23 Participation Study (SES website). 2023. Available at: https://shop-eat-surf.com/2023/09/sia-releases-2022-23-participation-study/. Accessed 07/01/2024.
- Bortolan L, Savoldelli A, Pellegrini B, et al. Ski mountaineering: perspectives on a novel sport to be introduced at the 2026 Winter Olympic Games. Front Physiol 2021;12:737249.
- Abrignani MG, Lombardo A, Braschi A, Renda N, Abrignani V. Climatic influences on cardiovascular diseases. World J Cardiol 2022;14:152-69.
- De Vita A, Belmusto A, Di Perna F, et al.; CLIMPS Group. The impact of climate change and extreme weather conditions on cardiovascular health and acute cardiovascular diseases. J Clin Med 2024;13:759.
- Honda H, Igaki M, Komatsu M, Tanaka SI. Seasonal variations on endothelium-dependent flow-mediated vasodilation in adults with type 2 diabetes and nondiabetic adults with hypertension and/or dyslipidaemia who perform regular exercise. Endocrinol Diabetes Metab 2020;4:e00168.
- Xiong S, Hou J, Yang H, et al. The profiles of venous thromboembolism at different high altitudes. High Alt Med Biol 2024;Apr 29:[ePub ahead of print].
- Shroff NA, Balbin J, Shobitan O. High-altitude illness: updates in prevention, identification, and treatment. Emerg Med Pract 2021;23:1-24.
- Luks AM, Beidleman BA, Freer L, et al. Wilderness medical society clinical practice guidelines for the prevention, diagnosis, and treatment of acute altitude illness: 2024 update. Wilderness Environ Med 2024;35:2S-19S.
- Zimmermann P, Schöffl I, Schöffl V, et al. Physiological effects of training in elite German winter sport athletes: sport specific remodeling determined using echocardiographic data and CPET performance parameters. J Cardiovasc Dev Dis 2022;9:235.
Clinical Topics: Sports and Exercise Cardiology
Keywords: Sports, Sports Medicine, Snow Sports, Athletes