Evaluation of Pulmonary Hypertension in Patients With Cancer
Quick Takes
- Evaluation for pulmonary hypertension (PH) in patients with cancer must include either lung ventilation/perfusion scan or dual-energy computed tomography of the chest to evaluate for acute and/or chronic thromboembolic disease.
- Targeted therapies for cancer known to increase the risk of PH include specific tyrosine kinase inhibitors (dasatinib, bosutinib, and ponatinib), proteasome inhibitors (carfilzomib and bortezomib), alkylating agents (e.g., cyclophosphamide and mitomycin C), trastuzumab, and gemcitabine.
- Rapidly progressive dyspnea in patients with metastatic solid organ tumors should prompt evaluation for PH with a high index of suspicion for pulmonary tumor thrombotic microangiopathy. Diagnostic evaluation includes right heart catheterization with pulmonary artery catheter sample of blood sent for cytology to look for malignant cells, imaging to identify fluorodeoxyglucose-avid disease in the chest, and multidisciplinary clinical correlation.
Pulmonary hypertension (PH) is a rare condition that reportedly affects 1% of the global population,1 although estimates vary on the basis of age group and setting.2 The most common cause of PH is left-sided heart failure (HF) and underlying pulmonary disease. However, in a minority of cases, PH is a disorder of the pulmonary vasculature, secondary to excessive vasoconstriction, arterial stiffening, vascular wall hypertrophy, and/or intraluminal obstruction. Patients with cancer are at higher risk of developing PH due to: 1) shared risk factors for cancer and PH such as smoking, obesity, and advanced age; 2) hypercoagulable state; and 3) the cancer and targeted therapies. Currently, the prevalence and etiology of PH in cancer remains unknown and understudied. One of the challenges in diagnosis of PH in patients with cancer is the significant overlap in symptoms of cancer and PH, such as dyspnea, fatigue, peripheral edema (e.g., with hypoalbuminemia and cancer therapy–related edema), and dizziness. As such, clinicians should have a high degree of vigilance in patients with cancer and employ screening tools for PH in suspected cases.
Initial screening for PH includes several noninvasive testing strategies.1 A transthoracic echocardiogram is the first-line screening tool to estimate the right ventricular systolic pressure (RVSP) using the tricuspid regurgitation jet, although it can be limited by severity of the regurgitant jet or insufficient visualization. The most common causes of elevated pulmonary pressures are elevated left-sided filling pressures, acute pneumonia/pneumonitis, or exacerbations of chronic lung conditions, as well as acute pulmonary embolism, which can improve with targeted treatments. If RVSP is elevated in the absence of these underlying acute pathologies, other supportive signs of PH should be evaluated, including right ventricular (RV) and right atrial size, RV outflow tract Doppler signals, pulmonary artery diameter, and RV functional parameters. Other supportive signs of PH may include enlarged pulmonary artery diameter on computed tomography (CT) of the chest and reduced diffusion capacity of the lungs for carbon monoxide that is out of proportion to the forced vital capacity measured in pulmonary function testing. Definitive testing should include right heart catheterization to define pulmonary hemodynamics and categorize patients into the three hemodynamic subgroups: 1) precapillary PH (pulmonary capillary wedge pressure [PCWP] ≤15 mm Hg and pulmonary vascular resistance [PVR] >2 Wood units [WU]), isolated postcapillary PH (PCWP >15 mm Hg and PVR ≤2 WU), or combined postcapillary and precapillary pulmonary hypertension (CpcPH; PCWP >15 mm Hg and PVR >2 WU).1
Patients who are found to have postcapillary PH or CpcPH should undergo workup and treatment for congestive HF. Patients may present with traditional risk factors such as hypertension, diabetes mellitus, and smoking, as well as cancer-specific causes such as cancer therapy–related cardiac dysfunction or myocarditis. Guideline-directed medical therapy for congestive HF should be initiated unless there are contraindications.
For patients with precapillary PH or CpcPH that is out of proportion to the wedge pressure, there are specific considerations in a cancer population. First, patients with cancer carry a fourfold to sevenfold higher risk of developing venous thromboembolic disease.3 As such, it is paramount to perform appropriate, noninvasive testing to assess for pulmonary perfusion defects. The most common test is a lung ventilation/perfusion (V/Q) scan, which should be performed as single-photon emission computed tomography images (SPECT-CT) since it has superior sensitivity to planar V/Q scan and single-energy CT pulmonary angiogram for chronic thrombi distal to the subsegmental level. If available, dual-energy CT is the reference standard for assessing perfusion defects and planning for procedures, such as balloon pulmonary angioplasty and pulmonary endarterectomy.
Second, specific cancer therapies have known associations with drug-induced pulmonary arterial hypertension (PAH). The French PH Registry has clearly demonstrated the association with dasatinib,4 a tyrosine kinase inhibitor commonly used to treat chronic myeloid leukemia, as well as carfilzomib,5 a proteasome inhibitor for the treatment of multiple myeloma. Other treatments with possible association include bosutinib, ponatinib, bortezomib, and certain immune checkpoint inhibitors.6 As new cancer-targeted therapies are developed, pharmacovigilance will be paramount to understand how they may affect pulmonary vascular biology.7
Third, patients with primary or metastatic tumors in the lungs may have pulmonary vascular obstructions that subsequently lead to PH. In some such cases, pulmonary artery stenting has been shown to be helpful in relieving symptoms of dyspnea.8 Myeloproliferative neoplasms are also known to cause PH, with poor survival outcomes comparable to those of patients with World Health Organization (WHO) Group 1 PAH.9 Currently, the pathogenic mechanisms of pulmonary vascular remodeling in these cases and the optimal therapeutic strategies remain unclear and are an important area for research.
Finally, patients with metastatic solid organ tumors can develop a rare form of precapillary PH called pulmonary tumor thrombotic microangiopathy.10 This is a rapidly progressive condition in which smooth muscle cells in the pulmonary vascular wall undergo progressive proliferation and intraluminal obstruction. Patients can present with a cough in addition to the typical symptoms associated with PH, likely due to bronchial irritation from metastatic cancer burden. A high index of suspicion is paramount in these cases and rapid evaluation to achieve the diagnosis, including cytology sent from pulmonary artery catheter to confirm the presence of malignant cells, may be helpful.
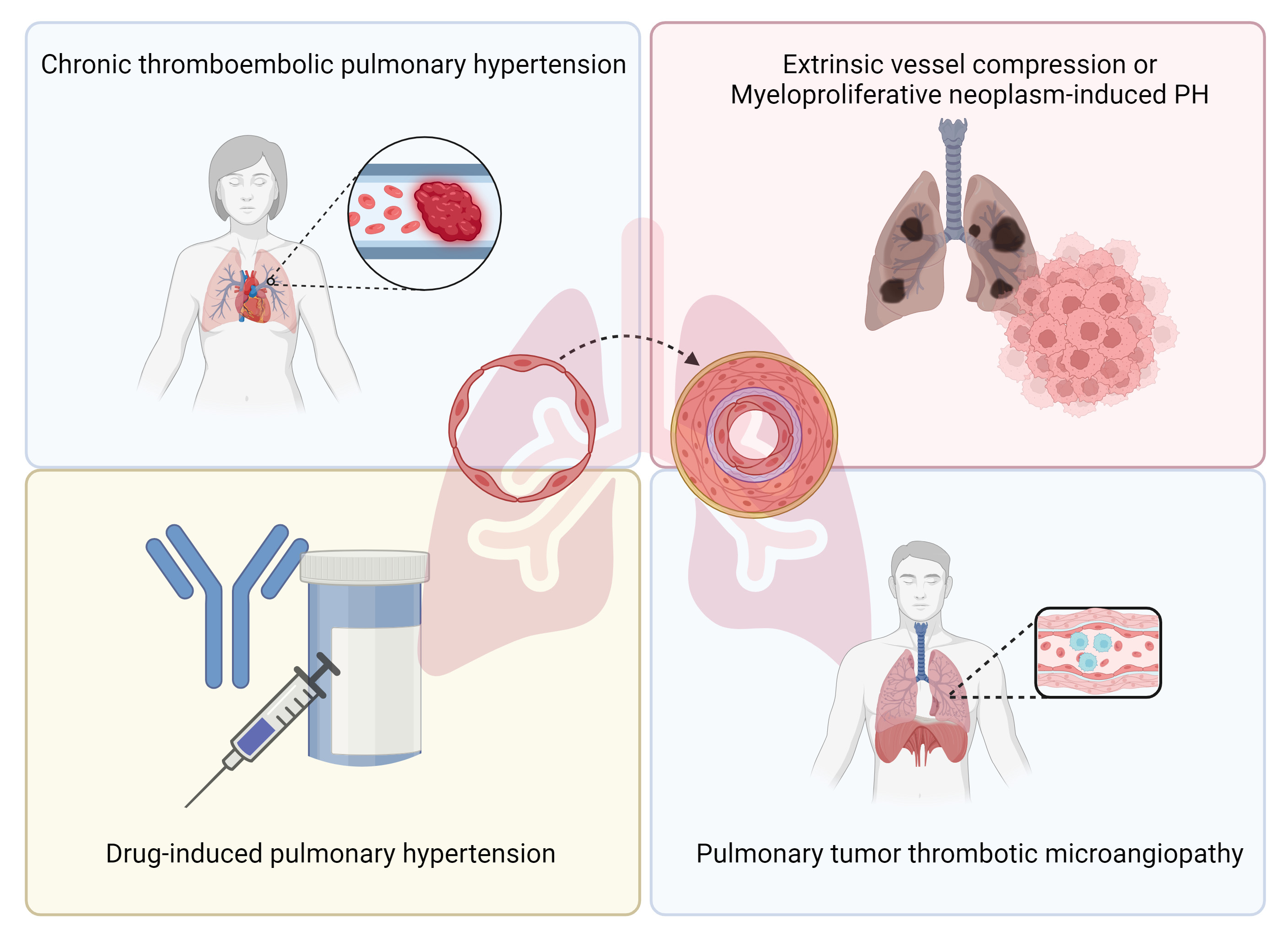
Future research in PH and cancer will need to consider the multiple mechanisms that are contributing to the development of pulmonary vasculopathies. Collaboration between oncologists and clinicians specializing in PH will be paramount to evaluate how PH impacts functional and survival outcomes of patients with cancer. Risk identification and stratification for developing PH in patients with cancer as well as assessment of therapeutic response will likely vary from the traditional ones relied on for PAH (Figure 1).
Figure 1: Diagnoses to Consider for Pulmonary Hypertension in Cancer
References
- Humbert M, Kovacs G, Hoeper MM, et al.; ESC/ERS Scientific Document Group. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J 2022;43:3618-731.
- Hoeper MM, Humbert M, Souza R, et al. A global view of pulmonary hypertension. Lancet Respir Med 2016;4:306-22.
- Mukai M, Oka T. Mechanism and management of cancer-associated thrombosis. J Cardiol 2018;72:89-93.
- Weatherald J, Chaumais MC, Savale L, et al. Long-term outcomes of dasatinib-induced pulmonary arterial hypertension: a population-based study. Eur Respir J 2017;50:[ePub ahead of print].
- Grynblat J, Khouri C, Hlavaty A, et al.; French PH Network PULMOTENSION Investigators. Characteristics and outcomes of patients developing pulmonary hypertension associated with proteasome inhibitors. Eur Respir J 2024;63:[ePub ahead of print].
- Palassin P, Maria ATJ, Ladhari C, et al. Pulmonary hypertension reported with immune checkpoint inhibitors: a pharmacovigilance study. Cancer Immunol Immunother 2022;71:3093-7.
- Umoru G, Taitano M, Beshay S, Niravath P, Sahay S. Pulmonary arterial hypertension in breast cancer patients on HER2-targeted therapy: a review of FDA Adverse Events Reporting System data. ERJ Open Res 2020;6:[ePub ahead of print].
- Gupta J, Patel R, Patel N, Wynne D, Ghasemi-Rad M. Pulmonary artery stenting in cancer patients: a single-center experience. Radiol Case Rep 2024;19:5370-5.
- Montani D, Thoré P, Mignard X, et al. Clinical phenotype and outcomes of pulmonary hypertension associated with myeloproliferative neoplasms: a population-based study. Am J Respir Crit Care Med 2023;208:600-12.
- Godbole RH, Saggar R, Kamangar N. Pulmonary tumor thrombotic microangiopathy: a systematic review. Pulm Circ 2019;9:[ePub ahead of print].
Clinical Topics: Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Vascular Medicine, Pulmonary Hypertension, Hypertension, Cardio-Oncology
Keywords: Hypertension, Pulmonary, Cardio-oncology, Cancer