Implementation of Age-Friendly Health Systems For Hospitalized Older Adults in Acute Cardiac Care Units
Quick Takes
- Age-Friendly Health Systems (AFHS) provide a structured framework for any health care setting to navigate care among older adults using the 4Ms: what matters, medication, mentation, and mobility.
- Beginning in 2025, hospitals that participate in Medicare's Hospital Inpatient Quality Reporting Program will need to report on whether they set up protocols to address and act on the measures related to the AFHS 4Ms.
- These requirements will also apply to patients in acute cardiac care units. Therefore, clinicians taking care of older adults in the acute cardiac care units should be aware of what the AFHS 4Ms framework is, how it can be integrated into routine clinical practice, and why it is critical in improving care for older adults.
Among the aging population of individuals, cardiovascular disease imposes a tremendous individual and societal impact. Moreover, providing cardiovascular care to this population of older adults requires complex consideration of the influences caused by multimorbidity, polypharmacy, reduced functional capacity, and the patient's social environment. Patients undergoing acute care in cardiac inpatient units have a higher risk of physical frailty, delirium, cerebral hypoperfusion given frequent low cardiac output, immobility due to device implantation, and complex pharmaceutical navigation of care.1 This makes it imperative to rapidly develop safe, methodical health care infrastructures, especially considering that it is estimated that the number of older adults >65 years of age is ever increasing.2
The John A. Hartford Foundation launched the Age-Friendly Health Systems (AFHS) initiative to address this challenge directly. The goals of AFHS include successfully implementing a core set of evidence-based practices, ensuring no harm, and focusing on what matters most to older adults and their family caregivers. Currently, there are >5,000 health care institutions which have been recognized as part of the AFHS initiative today, and that number continues to grow. Becoming an AFHS entails reliably providing a set of four evidence-based elements of high-quality care, known as the 4Ms, to all older adults in the system: what matters, medication, mentation, and mobility (Figure 1).3
Figure 1: Age-Friendly Health System 4Ms Framework
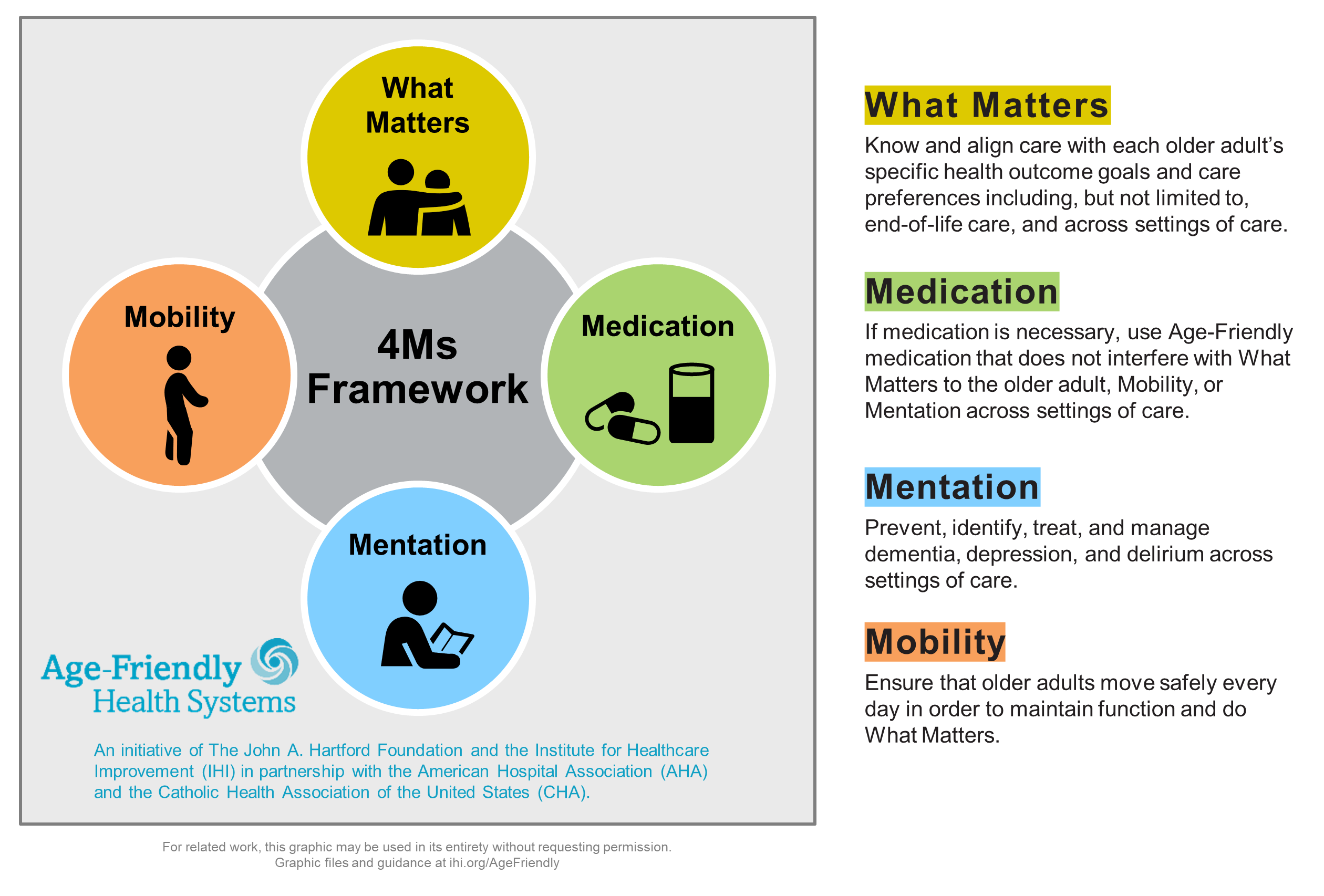
Courtesy of Institute for Healthcare Improvement, Boston, Massachusetts.
As a result of the successful dissemination of AFHS across the nation, starting in 2025, hospitals and institutions participating in Medicare's Hospital Inpatient Quality Reporting Program must report on their plans to implement all elements across multiple domains of the new Age-Friendly Hospital Measure starting in 2025.4 This article aims to describe the core components of AFHS and introduce examples of implementation strategies for these systems in caring for older patients with cardiovascular disease.
The component in the 4Ms framework called what matters suggests that providers must align the care plan with what matters to the patient. While it may be challenging to assess what matters to the patient during a busy, acute care setting, discussing the patient's value, preference, or priorities at least on admission or when the patient's condition changes could be helpful. This may allow for improved tailoring of health care to the individual needs and goals of older adults throughout their hospital stay, especially those with multiple chronic conditions.5 Moreover, how this question is framed to the patient is imperative as the need to educate with interpretable communication and readable materials has been found to have a significant role in setting patient goals. Additionally, discussing the patient's response during multidisciplinary rounds provides an avenue for direct, collaborative decision-making between the patient and their providers, improving patient health outcomes.6
Regarding the assessment of mentation, optimal delirium management is the most feasible strategy in the acute hospital setting. The acute cardiac care unit may implement a standardized delirium assessment that can be used during shift changes. For example, Confusion Assessment Methods (CAM), the most widely used assessment tool for delirium, can be implemented. In the intensive care unit (ICU), CAM for the ICU can be used among patients who are intubated.7
The medication assessment of the 4Ms framework could be implemented by pharmacists and clinicians using Beers Criteria of Potentially Inappropriate Medication Use in Older Adults or Screening Tool of Older People's Prescriptions/Screening Tool to Alert to Right Treatment criteria to avoid potentially inappropriate medications. Furthermore, it is well established in the literature that this criterion is integrated into the electronic medical record of most hospitals and institutions. Another level of active utilization of this criterion may include having a pharmacist present during multidisciplinary rounds to evaluate active medications flagged as potentially inappropriate per Beers Criteria.8 These methods can further strengthen a hospital's or institution's adherence to the medication domain of an AFHS.
Regarding the mobility assessment, a patient's care team should regularly assess and support older adults' progress toward their daily mobility goals. Within this domain, indexing tools used to evaluate a patient's fall risk or frailty may be considered. Likewise, clinician care teams may consider the early involvement of physical therapy teams during a patient's hospital course.6,9 These teams may also benefit from using the Elderly Mobility Scale to better assess this domain for a patient. Additionally, there also needs to be daily, consistent communication between a patient's physical therapy team, nursing, and clinician care team to better integrate mobility within the patient's goal setting.10
Implementing the AFHS model across hospitals and institutions offers a standardized, evidenced-based geriatric needs assessment for patients in acute care settings as patients of older age have a further predisposition to worse health outcomes.5,6,9 Beyond this framework, the early involvement of a geriatrician in a patient's care plan will also promote collaboration among cardiovascular disease specialists to navigate complex care among these patients.
References
- Metkus TS, Lindsley J, Fair L, et al. Quality of heart failure care in the intensive care unit. J Card Fail 2021;27:1111-25.
- Bureau UC. Older People Projected to Outnumber Children for First Time in U.S. History (United States Census Bureau website). 2018. Available at: https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html . Accessed 02/27/2025.
- The John A. Hartford Foundation. Age-Friendly Health Systems Initiative (The John A. Hartford Foundation website). Available at: https://www.johnahartford.org/grants-strategy/current-strategies/age-friendly/age-friendly-health-systems-initiative . Accessed 02/27/2025.
- The John A. Hartford Foundation. New CMS Measure Will Publicly Report On Hospitals' Commitment And Capabilities To Provide Age-Friendly Care (The John A. Hartford Foundation website). 2024. Available at: https://www.johnahartford.org/newsroom/view/new-cms-measure-will-publicly-report-on-hospitals-commitment-and-capabilities-to-provide-age-friendly-care . Accessed 02/27/2025.
- Kwak MJ, Jones M, Mills C, et al. Feasibility of the Age-Friendly Health System in Acute Cardiac Care Units for Delirium Detection and Management (Delirium Communications Journal website). 2023. Available at: https://deliriumcommunicationsjournal.com/article/84053-feasibility-of-the-age-friendly-health-system-in-acute-cardiac-care-units-for-delirium-detection-and-management . Accessed 02/27/2025.
- Mate K, Fulmer T, Pelton L, et al. Evidence for the 4Ms: interactions and outcomes across the care continuum. J Aging Health 2021;33:469-81.
- Miranda F, Arevalo‐Rodriguez I, Díaz G, et al. Confusion Assessment Method for the intensive care unit (CAM‐ICU) for the diagnosis of delirium in adults in critical care settings. Cochrane Database Syst Rev 2018;2018:[ePub ahead of print].
- Akande-Sholabi W, Fafemi A. Potentially inappropriate medication use in the elderly: physicians' and hospital pharmacists knowledge, practice, confidence, and barriers. J Pharm Health Care Sci 2022;8:36.
- Goyal P, Kwak MJ, Al Malouf C, et al. Geriatric cardiology: coming of age. JACC Adv 2022;1:[ePub ahead of print].
- Kava CM, Fishleder S, Steinman L, Petrescu-Prahova M, Schrodt L, Harris JR. Provider–patient communication and involvement in physical activity programs among patients receiving physical therapy services: a qualitative study. J Appl Gerontol 2020;39:1000-7.
Clinical Topics: Geriatric Cardiology
Keywords: Geriatric Cardiology, Geriatrics, Care Team, Patient Care Team