Disparities in Hypertension Across Age Spectrum Among Asian American Adults: The Power of Data Disaggregation
Quick Takes
- Filipino American adults have a higher prevalence of early onset hypertension than any other Asian American subgroup and would benefit from earlier screening.
- Implementing culturally tailored lifestyle interventions, such as community education workshops or development of low-sodium Filipino recipes, is necessary to promote hypertension prevention and management in this group.
- Coronary artery calcium scoring may have utility in guiding early antihypertensive therapy in high-risk Filipino individuals.
Commentary based on Gordon NP, Lien IC, Rana JS, Lo JC. U.S. Filipino adults have elevated prevalence of hypertension across the adult lifespan: findings from a cross-sectional electronic health record study. AJPM Focus 2024;3:[ePub ahead of print].1
Background
There is an increasing appreciation of the racial differences in cardiovascular disease (CVD) risk profiles and subsequent outcomes. This recognition has led to meaningful changes in clinical practice, such as screening for diabetes mellitus earlier in Hispanic American adults and at a lower body mass index threshold for Asian American adults.2 The Asian American population is a quickly growing racial group in America, with recent research focused on understanding the often earlier onset of adverse CVD events in this group. Despite trends from larger ethnic studies revealing key differences in CVD trends among Asian subgroups, very limited disaggregated data exist.3
To address this gap, Gordon et al. conducted a disaggregated analysis of electronic health record data from a large, diverse cohort within the Kaiser Permanente Northern California health care system to compare the prevalence of hypertension (defined using diagnosis codes) among six racial groups: white, Black, Hispanic, Chinese, Filipino, and South Asian. Out of 1,839,603 adults, 55% were white, 8% Black, 19% Hispanic, 7% Chinese, 7% Filipino, and 4% South Asian. Adjusting for covariates, the study found that across all ages between 30-79 years, Black and Filipino adults had a similar and much higher prevalence of hypertension than South Asian, Chinese, Hispanic, and white adults. The greatest disparities were observed for adults aged <60 years and particularly in women.
Commentary
The present study builds on existing evidence that disaggregating data is crucial to revealing the unique CVD patterns within Asian subgroups. Often, Asian American adults are viewed and clinically managed as a monolithic group. However, as this study highlights, understanding the key distinctions in profiles can lead to more targeted health screening practices and interventions.
Despite having smaller sample sizes with comparatively lower representation of Filipinos, similar cohort studies also found high prevalence of hypertension (>30%) in Filipino adults (Figure 1).4-5 These studies also highlighted a high prevalence of early onset hypertension and, importantly, a rapidly growing incidence of hypertension over the past few decades. The etiology of this high rate of hypertension is likely multifactorial with variable contributions from genetics, dietary differences, health literacy, social stressors, and for immigrants, acculturation to life in the United States.6
Figure 1: Prevalence of Hypertension Among Asian American Subgroups
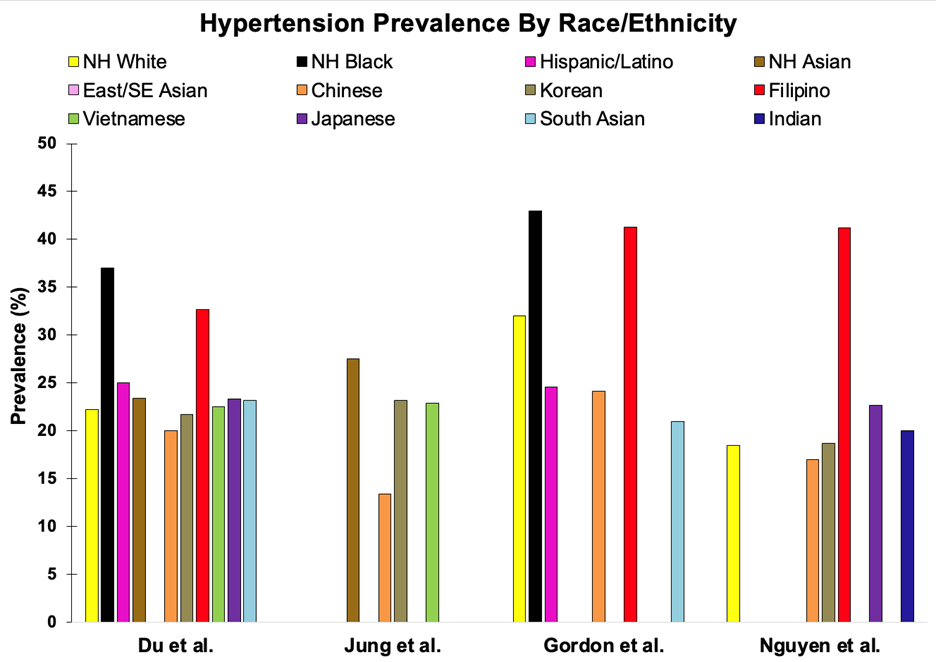
NH = non-Hispanic; SE = Southeast.
Given these findings, focused interventions have been developed in the recent years to address the unique risk factors and health behaviors that lead to increased hypertension burden in the Filipino population. A community-based participatory research study by Ma et al. showed that culturally tailored education workshops on physical activity and reduced salt intake improved hypertension awareness, medication adherence, and self-management behaviors in a Filipino community in Greater Philadelphia.7 Recognizing the increased salt sensitivity in Asians, Sijangga et al. developed a cookbook with healthy, low-salt versions of traditional Filipino recipes and found it to be effective in promoting positive dietary changes in a pilot sample of Filipino participants with hypertension.8
Despite the promising findings of these lifestyle modification interventions, significant gaps remain in hypertension prevention and early detection. Most studies, including the one by Gordon et al., primarily focused on individuals with existing hypertension or those at-risk based on older age and other comorbidities. As Gordon et al. highlight, however, hypertension prevalence in Filipino and Black individuals prematurely starts between the ages of 30 to 39 compared with the ages of 40 to 49 for other racial groups.1 This trend not only underscores the importance of earlier screening but also the necessity for heightened awareness and efforts to identify at-risk individuals prior to disease onset. Current risk calculators for adverse CVD outcomes, such as the Pooled Cohort Equations and the Predicting Risk of cardiovascular disease EVENTs risk calculator estimate 10-year atherosclerotic cardiovascular disease (ASCVD) risk; however, they may inaccurately capture risk in Asian subgroups and fail to predict risk before the onset of conditions such as hypertension, diabetes mellitus, or obesity.9 Tailored risk assessment tools therefore are necessary to address the high prevalence of premature hypertension in Filipinos.
Beyond risk-stratification, the question of when to initiate medical therapy in this high-risk population also remains. While medical therapy is generally initiated when blood pressure is >140/90 mm Hg or if ASCVD risk is >10%, lifestyle modifications are usually first line for stage 1 hypertension. Given that ASCVD risk is likely to be underestimated in Asian subgroups, Filipino American adults with early onset hypertension may not be initiated on antihypertensive therapy, despite the otherwise high burden of adverse CVD outcomes.6
Coronary artery calcium (CAC) scoring has increasingly been described to be beneficial in identifying high-risk individuals, and studies have found that even non-Asian individuals with elevated CAC scores and hypertension have poorer outcomes.9 There is high interest in utilizing CAC scoring to guide care in South Asian American adults, who also have a disproportionately high burden of adverse CVD outcomes.9 There is limited application of CAC scoring to the Filipino population, but it could potentially be an avenue to identify those with hypertension who may benefit the most from pharmacotherapy and lifestyle modifications.
The intensity of antihypertensive therapy is another area that needs to be explored.The recent ESPRIT (Effects of Intensive Systolic Blood Pressure Lower Treatment in Reducing Risk of Vascular Events) trial, a large randomized controlled trial conducted in China, found that intensive systolic blood pressure control (<120 mm Hg), as compared with standard control (<140 mm Hg), reduced major cardiovascular events in a population with high cardiovascular risk.10 Generalizability of these findings to a Filipino population is unclear given the differences Gordon et al. illustrated between Chinese and Filipino clinical profiles. However, the results do warrant studying the potential benefit of more intensive antihypertensive therapy in Filipino individuals.
Conclusion
CVD in Asian American adults is complex due to differences in the clinical risk factors that lead to adverse outcomes among the subgroups. The current study identifies a higher prevalence of hypertension, especially early onset hypertension, in the Filipino subgroup as compared with other Asian subgroups and reveals the necessity of improved risk stratification and tailored treatment strategies. CAC testing may prove to be helpful to guide initiation and intensification of antihypertensive therapy among Asian subgroups, although outcome data are needed to help clarify widespread recommendations.
References
- Gordon NP, Lien IC, Rana JS, Lo JC. U.S. Filipino adults have elevated prevalence of hypertension across the adult lifespan: findings from a cross-sectional electronic health record study. AJPM Focus 2024;3:[ePub ahead of print].
- Standards of medical care in diabetes--2015: summary of revisions. Diabetes Care 2015;38 Suppl:[ePub ahead of print].
- Manjunath L, Chung S, Li J, Shah H, Palaniappan L, Yong CM. Heterogeneity of treatment and outcomes among Asians with coronary artery disease in the United States. J Am Heart Assoc 2020;9:[ePub ahead of print].
- Du Y, Shih M, Lightstone AS, Baldwin S. Hypertension among Asians in Los Angeles County: findings from a multiyear survey. Prev Med Rep 2017;6:302-6.
- Nguyen KT, Li J, Peng AW, et al. Temporal trends in cardiovascular disease prevalence among Asian American subgroups. J Am Heart Assoc 2024;13:[ePub ahead of print].
- Coronado G, Chio-Lauri J, Cruz RD, Roman YM. Health disparities of cardiometabolic disorders among Filipino Americans: implications for health equity and community-based genetic research. J Racial Ethn Health Disparities 2022;9:2560-7.
- Ma GX, Bhimla A, Zhu L, et al. Development of an intervention to promote physical activity and reduce dietary sodium intake for preventing hypertension and chronic disease in Filipino Americans. J Racial Ethn Health Disparities 2021;8:283-92.
- Sijangga MO, Pack DV, Yokota NO, Vien MH, Dryland ADG, Ivey SL. Culturally-tailored cookbook for promoting positive dietary change among hypertensive Filipino Americans: a pilot study. Front Nutr 2023;10:[ePub ahead of print].
- Gami A, Bisht S, Satish P, Blaha MJ, Patel J. The utility of coronary artery calcium scoring to enhance cardiovascular risk assessment for South Asian adults. Prog Cardiovasc Dis 2024;84:7-13.
- Liu J, Li Y, Ge J, et al.; ESPRIT Collaborative Group. Lowering systolic blood pressure to less than 120 mm Hg versus less than 140 mm Hg in patients with high cardiovascular risk with and without diabetes or previous stroke: an open-label, blinded-outcome, randomised trial. Lancet 2024;404:245-55.
Clinical Topics: Prevention, Hypertension, Pulmonary Hypertension and Venous Thromboembolism
Keywords: Hypertension, Asian Americans, Primary Prevention