Novel Adipokine Hypothesis Offers Framework to Explain Pathogenesis and Guide Treatment of HFpEF
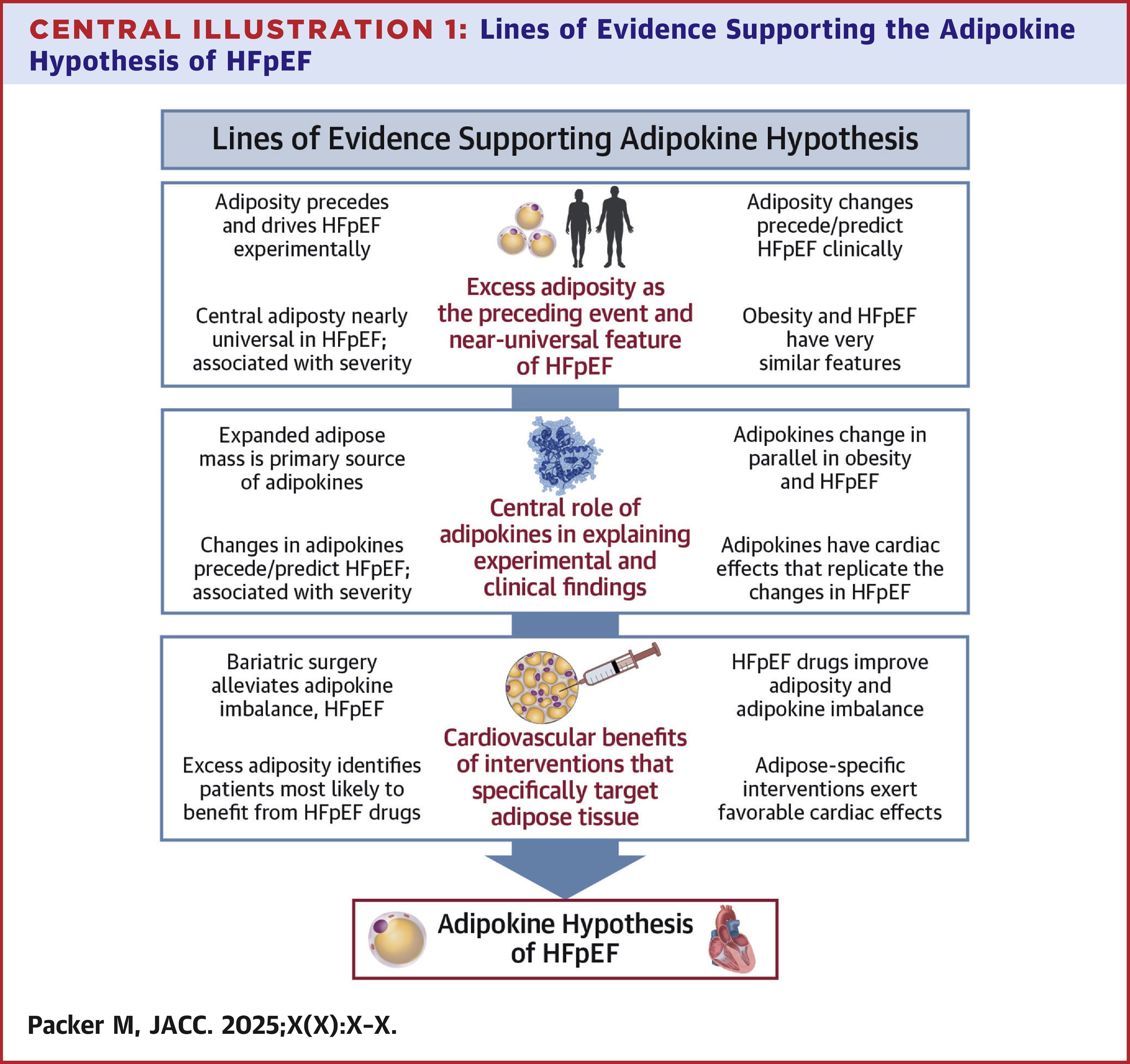
Heart failure with preserved ejection fraction (HFpEF) appears to arise "primarily from the expansion and dysfunctional transformation of visceral adipose tissue, leading to the secretion of altered suite of signaling molecules (adipokines), which causes systemic inflammation, plasma volume expansion, and cardiac hypertrophy and fibrosis," according to the Adipokine Hypothesis authored by Milton Packer, MD, FACC, and published as a State-of-the-Art Review in JACC.
"Up to now, there has been no unifying hypothesis to explain HFpEF. That has resulted in significant misunderstanding and a lack of direction in both diagnosis and therapy," said Packer, who presented the findings presented at ESC Congress 2025. "This bold new framework helps to identify the true cause of HFpEF in most people. That should make an enormous difference in guiding effective treatments."
The Adipokine Hypothesis points to the importance of using drugs that shrink fat tissue and restore its healthy biology. Many of these drugs are already approved by the U.S. Food and Drug Administration for the treatment of HFpEF, but they are not widely prescribed. In addition, GLP-1 receptor agonists – semaglutide and tirzepatide – can exert favorable effects on the release of adipokines.
According to the paper, the term obesity should not be used to identify people with excessive internal fat tissue. Obesity is defined by body mass index, which is heavily influenced by bone and muscle. Instead, the most reliable approach for identifying people with excess internal fat stores is to measure the ratio of waist to height. Normally, the ratio should be less than 0.5, meaning that the waist is less than half of the height. Nearly all patients with HFpEF have a waist-to-height ratio greater than 0.5, and often greater than 0.6. Such a ratio is clinically important, even when the body mass index does not fulfill criteria for obesity.
"In patients with an elevated waist-to-height ratio, clinicians should be very vigilant to ask patients about potential symptoms of HFpEF," Packer said. "Many people who are short of breath with walking attribute their symptoms to obesity, when in fact, these symptoms are related to HFpEF and can be effectively treated."
In a related editorial, JACC Editor-in-Chief Harlan M. Krumholz, MD, SM, FACC, calls the hypothesis "bold, densely argued and deliberately provocative," and writes: "We did not publish this work because it is definitive. We published it because it is generative. It provokes new questions, offers a coherent structure for scientific exploration, and invites rigorous challenge."
He goes on to add that the Adipokine Hypothesis "evokes Dr. Packer's earlier articulation of the neurohormonal hypothesis of heart failure with reduced ejection fraction (HFrEF), a framework that reshaped how we understood and treated that condition. Although this new hypothesis lacks the decades of confirmatory data that now support neurohormonal modulation in HFrEF, it offers a testable and coherent model of disease. It is, without question, an idea worth testing."
Access two related papers in JACC: Heart Failure:
Clinical Topics: Heart Failure and Cardiomyopathies, Acute Heart Failure
Keywords: ESC Congress, ESC25, Heart Failure, Semaglutide, Adipokines, Obesity