Cardiopulmonary Exercise Testing in Congenital Heart Disease: Key Points From the Recent AHA Scientific Statement
Quick Takes
- Data from cardiopulmonary exercise testing (CPET) provides important information about the functional status of patients with a range of congenital heart disease (CHD).
- CPET data in patients with CHD, even those with simple lesions, reveal consistently suboptimal cardiorespiratory fitness compared with unaffected peers and may be improved by exercise therapy.
- CPET variables, especially on serial testing, can be strong prognostic indicators of future cardiovascular outcomes and can be used to guide decision-making and therapy.
The recent scientific statement titled Cardiopulmonary Exercise Test Interpretation Across the Lifespan in Congenital Heart Disease: A Scientific Statement From the American Heart Association provides an updated evidence-based approach to interpreting cardiopulmonary exercise testing (CPET) in children, adolescents, and adults with congenital heart disease (CHD).1 Historically, there has been widespread underutilization of this key diagnostic tool due to lack of both exposure to exercise testing and understanding of the clinical relevance of the data. This scientific statement serves to improve clinician understanding of CPET findings for diverse patients with variable exercise performance based on underlying lesion and physiology (Figure 1).
Figure 1: The Range of Peak V̇O2 Across the Spectrum of CHD
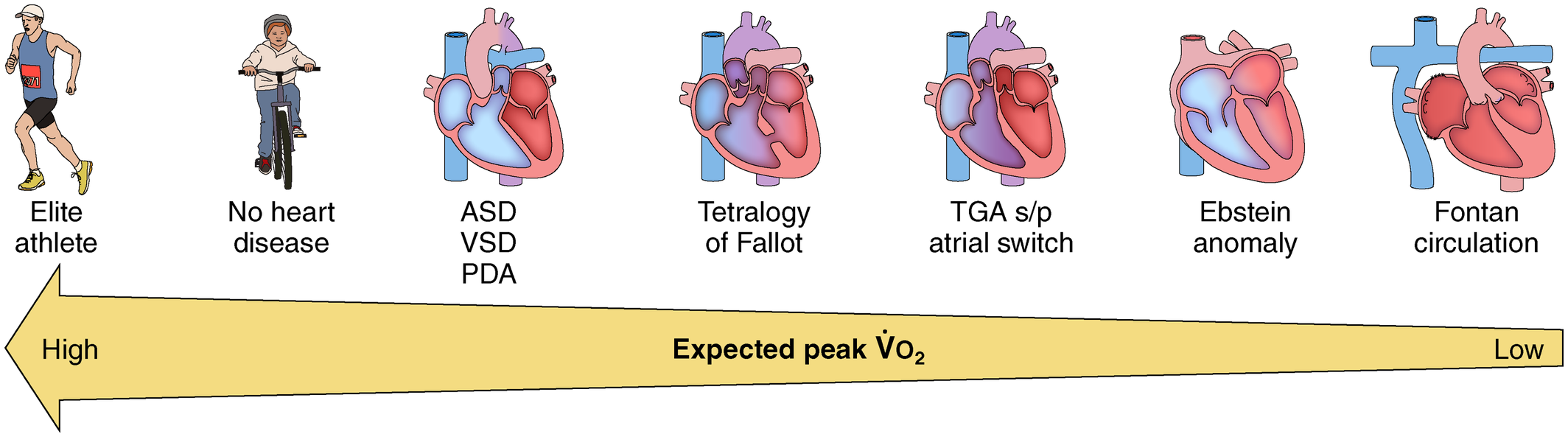
Reprinted with permission from Cifra B, Cordina RL, Gauthier N, et al. Cardiopulmonary exercise test interpretation across the lifespan in congenital heart disease: a scientific statement from the American Heart Association. J Am Heart Assoc. 2025;14(4):e038200. doi:10.1161/JAHA.124.038200
ASD = atrial septal defect; CHD = congenital heart disease; PDA = patent ductus arteriosus; s/p = status post; TGA = transposition of the great arteries; V̇O2 = oxygen consumption; VSD = ventricular septal defect.
The scientific statement focuses on indications for CPET, expected findings, key variables by pathology, and how CPET should guide clinical decision-making. Included in the scientific statement are supplemental tables that provide a helpful, concise resource for a range of lesions (Table 1 is one such example).
Table 1: Typical CPET Findings for Patients With Tetralogy of Fallot Compared With Unaffected Healthy Peers
| Diagnosis | Important Findings Compared With Healthy Peers |
| Tetralogy of Fallot |
|
Adapted with permission from Cifra B, Cordina RL, Gauthier N, et al. Cardiopulmonary exercise test interpretation across the lifespan in congenital heart disease: a scientific statement from the American Heart Association. J Am Heart Assoc. 2025;14(4):e038200. doi:10.1161/JAHA.124.038200
a Poor outcomes include hospitalization, need for reintervention, cardiac-related events, and cardiac-related mortality.
BP = blood pressure; CPET = cardiopulmonary exercise testing; ECG = electrocardiogram; HR = heart rate; PFT = pulmonary function test; PVR = pulmonary valve replacement; SpO2 = oxygen saturation; QRSd = QRS duration; VE/VCO2 =minute ventilation/carbon dioxide production; VO2 = oxygen consumption.
There are 10 key take-home points from this scientific statement:
- CPET provides a reliable measure of exercise capacity that has significant prognostic ability in patients with CHD (Figure 2).
- Serial testing beginning in childhood can reveal abnormalities associated with poor outcomes and enable earlier treatment, including catheter- and surgical-based interventions.
- In patients with corrected atrial septal defects, ventricular septal defects, and patent ductus arteriosus, the peak oxygen consumption (VO2) is often abnormally low and declines faster than in nonaffected individuals.
- CPET in patients with dextro-transposition of the great arteries repaired via atrial switch often shows profoundly decreased peak VO2 secondary to impaired chronotropy and stroke volume (SV), whereas the peak VO2 in those repaired by arterial switch is usually well preserved unless there is residual right ventricular outflow tract obstruction.
- CPET in patients with tetralogy of Fallot has been extensively studied with abnormalities seen in multiple variables that can guide clinical decision-making (Table 1), including timing of transcatheter pulmonary valve placement.
- Patients with Fontan circulation often have low peak VO2, chronotropic incompetence, and impaired SV secondary to the absence of a subpulmonary pump. Patients with a Fontan circulation and peak VO2 > 80% predicted tend to participate more in regular moderate and vigorous physical activity.
- Patients with Ebstein anomaly often have lower peak VO2 than seen in other cardiac lesions, and peak VO2 <60% is associated with poor clinical outcomes in adults.
- Exercise-induced hypertension (HTN) is common even in patients with well-repaired coarctation of the aorta and is linked with the development of later HTN. Peak VO2 may be normal or reduced.
- In patients with aortic valve stenosis, peak VO2 may be normal or mildly reduced. The presence of ischemic changes on exercise electrocardiography is associated with poor outcomes.
- The scientific statement provides a framework and context for understanding CPET results to improve the utilization of testing, allow a more accurate application of test results for patient management, and provide data to assist with improved patient outcomes.
Figure 2: Key Noteworthy Cardiopulmonary Values That Carry Specific Prognostic Significance in Certain CHD Lesions
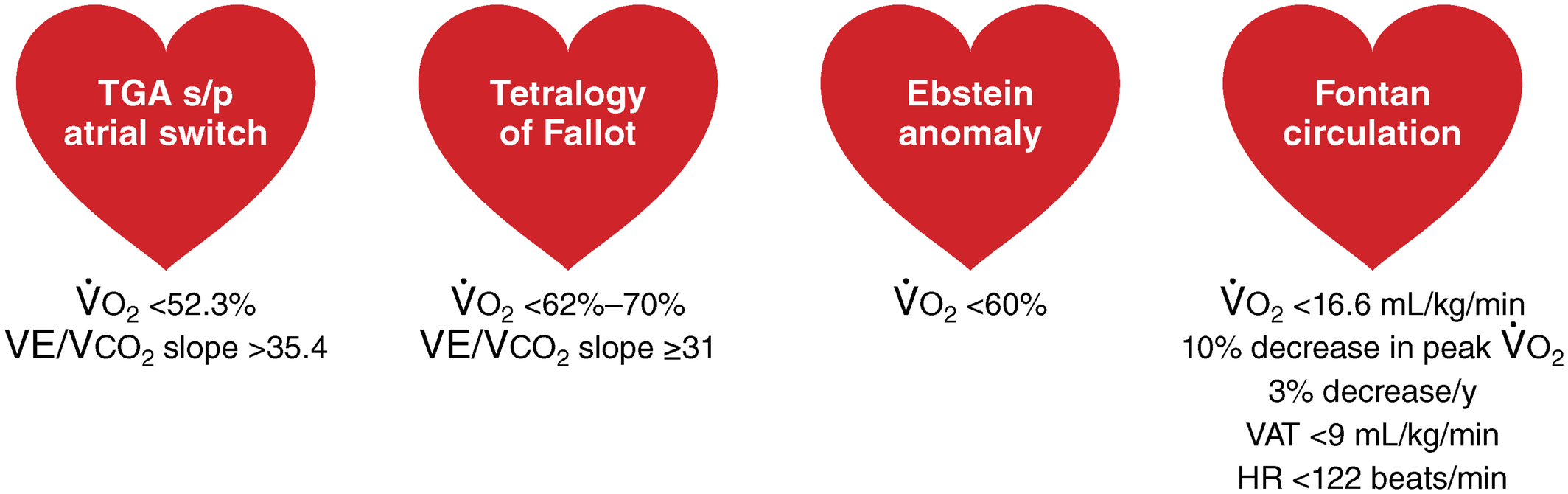
Reprinted with permission from Cifra B, Cordina RL, Gauthier N, et al. Cardiopulmonary exercise test interpretation across the lifespan in congenital heart disease: a scientific statement from the American Heart Association. J Am Heart Assoc. 2025;14(4):e038200. doi:10.1161/JAHA.124.038200
CHD = congenital heart disease; HR = heart rate; s/p = status post; TGA = transposition of the great arteries; VAT = ventilatory anaerobic threshold; VE/VCO2 = minute ventilation/carbon dioxide production; V̇O2 = oxygen consumption.
References
- Cifra B, Cordina RL, Gauthier N, et al. Cardiopulmonary exercise test interpretation across the lifespan in congenital heart disease: a scientific statement from the American Heart Association. J Am Heart Assoc. 2025;14(4):e038200. doi:10.1161/JAHA.124.038200
Clinical Topics: Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Congenital Heart Disease, Sports and Exercise Cardiology
Keywords: American Heart Association, Exercise Test, Heart Defects, Congenital, Pulmonary Heart Disease, Quality of Life, Survivorship