Effect of Sotagliflozin on Cardiovascular Events in Patients With Type 2 Diabetes Post Worsening Heart Failure - SOLOIST-WHF
Contribution To Literature:
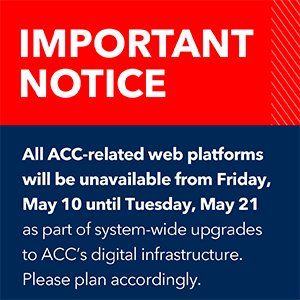
Highlighted text has been updated as of August 7, 2023.
The SOLOIST-WHF trial showed that sotagliflozin has salutary effects on CV outcomes among patients with T2DM and HF.
Description:
The goal of the trial was to assess the safety and efficacy of sotagliflozin in reducing cardiovascular (CV) events among patients with type 2 diabetes mellitus (T2DM) and recent heart failure (HF) admission.
Study Design
Eligible patients were randomized in a 1:1 fashion to either sotagliflozin 400 mg daily (n = 608) or placebo (n = 614). Sotagliflozin was started at 200 mg daily and increased to target dose if there were no unacceptable side effects. The drug was initiated either prior to or within 3 days of discharge.
- Total screened: 1,549
- Total number of enrollees: 1,222
- Duration of follow-up: median 9 months
- Mean patient age: 69 years
- Percentage female: 34%
Inclusion criteria:
- Admission with HF
- Treatment with diuretics
- Stabilized, off oxygen, transitioned to oral diuretics
- B-type natriuretic peptide (BNP) ≥150 pg/ml (≥450 pg/ml if atrial fibrillation) or N-terminal pro–BNP ≥600 pg/ml (≥1800 pg/ml if atrial fibrillation)
- T2DM
Exclusion criteria:
- End-stage HF
- Recent acute coronary syndrome, stroke, percutaneous coronary intervention, or coronary artery bypass grafting
- Estimated glomerular filtration rate (eGFR) <30 ml/min/1.73 m2
Other salient features:
- Left ventricular ejection fraction (LVEF): 35%; <50%: 79%
- Median eGFR: 50 ml/min/1.73 m2
- Median glycated hemoglobin (HbA1c): 7.2%
- Use of any renin-angiotensin-aldosterone system inhibitor: 92%
- Metformin: 52%
Principal Findings:
The trial stopped early due to loss of funding due to COVID-19. The primary endpoint of total CV death, hospitalization for HF, or urgent visit for HF for sotagliflozin vs. placebo, was 70 vs. 98 events/100 patient-years (hazard ratio 0.67, 95% confidence interval [CI] 0.52-0.85, p = 0.0009). This achieved significance by 28 days of follow-up.
Secondary outcomes for sotagliflozin vs. placebo:
- Total CV death and hospitalization for HF: 60 vs. 86 events/100 patient-years (p = 0.003)
- First CV death and hospitalization for HF: 33% vs. 48% (p = 0.003)
- CV death: 10.6 vs. 12.5 events/100 patient-years (p = 0.36)
- Change in Kansas City Cardiomyopathy Questionnaire (KCCQ)-12 score: 17.7 vs. 13.6 (p = 0.005)
- Change in eGFR: -0.34 vs. -0.18 (p = 0.78)
Safety for sotagliflozin vs. placebo:
- Diarrhea: 6.9% vs. 4.1% (p = 0.032)
- Genital fungal infections: 0.8% vs. 0.2% (p = 0.12)
- Severe hypoglycemia: 1.5% vs. 0.3% (p = 0.037)
Pooled SCORED and SOLOIST-WHF data (n = 11,784):
Total CV death, hospitalization for HF, or urgent HF visit for sotagliflozin vs. placebo was 15.5 vs. 21.1/100 patient-years (p = 0.000002).
- EF <40%: 47.8% vs. 60.4% (p = 0.02)
- EF 40 to <50%: 45.2% vs. 71.3% (p = 0.02)
- EF ≥50%: 37.5% vs. 59.0% (p = 0.009)
- No history of HF, EF ≥50%: 5.2% vs. 6.2% (p = 0.04)
Total HF hospitalization and urgent HF visits were similarly reduced in each trial with sotagliflozin, and also in the pooled analysis. CV death was not reduced in the pooled intention-to-treat analysis, but a reduction was noted in the on-treatment analysis (HR 0.77, 95% CI 0.60-0.98). Benefits were also preserved for men and women. In various analyses accounting for adherence to the study drug and desired target dose, sotagliflozin consistently reduced the primary endpoint, HF hospitalization, myocardial infarction, stroke, kidney endpoints, cardiovascular death, and all-cause mortality. The reductions in HF endpoints with the target dose of sotagliflozin were particularly pronounced.
Total hospitalizations: ≥1 hospitalization for sotagliflozin vs. placebo: 38.5% vs. 41.4% (p = 0.3); >1 hospitalization: 16.3% vs. 22.1% (p = 0.009). Mean days alive and out of the hospital: 280 vs. 267 (rate ratio 1.03, 95% CI 1.00-1.06; p = 0.027).
Time to benefit: For the primary endpoint, time to sustained reduction for sotagliflozin vs. placebo: 27 days (35 days if EF <50%; 70 days if EF ≥50%, p for interaction = 0.21). For total HF hospitalization, time to sustained reduction for sotagliflozin vs. placebo: 27 days (42 days if EF <50%; 71 days if EF ≥50%).
Early mortality and HF events: 290 sotagliflozin recipients and 306 placebo recipients started study drug a median of 7 days after admission and prior to discharge. Sotagliflozin reduced the primary endpoint at 90 days post-discharge (10.8% vs. 19.9%, HR 0.54, 95% CI 0.35-0.82, p = 0.004) and at 30 days (5.2% vs. 10.2%, HR 0.49, 95% CI 0.27-0.91, p = 0.023) and all-cause mortality at 90 days (3.1% vs. 7.4%, HR 0.39, 95% CI 0.17-0.88, p = 0.024).
Interpretation:
The results of this trial indicate that sotagliflozin has salutary effects on CV outcomes among patients with T2DM and HF. Patient-centric outcomes such as days alive and out of the hospital were also improved with sotagliflozin compared with placebo. Earlier termination may have affected the ability to see reductions in individual components of the primary outcome. Among patients hospitalized with HF, initiation of sotagliflozin prior to discharge appeared to improve outcomes within 90 days. In the pooled analysis of SCORED and SOLOIST-WHF data, benefits were preserved irrespective of baseline EF (including among patients with HF with preserved EF [HFpEF]) and prior history of HF. Time to benefit was numerically longer in patients with HFpEF but there was no statistically significant interaction of LVEF on the primary outcome.
Sotagliflozin is a sodium-glucose cotransporter-2 (SGLT2) inhibitor, but also inhibits SGLT1, which primarily exists in the gut and appears to delay glucose absorption. The results of this trial are similar to those noted with dapagliflozin in the DAPA-HF trial and with empagliflozin in the EMPEROR-Reduced trial, although these two trials included patients with HF with reduced EF, irrespective of T2DM status. In the pooled analysis of SOLOIST and SCORED, a benefit was also noted among patients with T2DM and HFpEF. This is the first agent to show this benefit; trials with other agents such as EMPEROR-Preserved with empagliflozin are ongoing. As a class, these agents will likely play a prominent role among patients with chronic kidney disease and HF, and possibly even in the absence of T2DM.
SOLOIST-WHF is the first large randomized controlled trial to show that initiation of SGLT2 inhibition in acute HF in stabilized patients prior to discharge or shortly thereafter is safe and effective. The benefits were consistent in those with HF with reduced but also preserved EF.
References:
Pitt B, Bhatt DL, Szarek M, et al. Effect of Sotagliflozin on Early Mortality and Heart Failure-Related Events: A Post Hoc Analysis of SOLOIST-WHF. JACC Heart Fail 2023;11:870-89.
Editorial Comment: Howlett JB. What Difference Does a Day Make? JACC Heart Fail 2023;11:890-2.
Verma S, Bhatt DL, Dhingra NK, et al. Time to Benefit With Sotagliflozin in Patients With Worsening Heart Failure. J Am Coll Cardiol 2023;81:1546-9.
Presented by Dr. Deepak L. Bhatt at the European Society of Cardiology Virtual Congress, August 23, 2021.
Szarek M, Bhatt DL, Steg PG, et al., on behalf of the SOLOIST-WHF Committees and Investigators. Effect of Sotagliflozin on Total Hospitalizations in Patients With Type 2 Diabetes and Worsening Heart Failure: A Randomized Trial. Ann Intern Med 2021;Jun 22:[Epub ahead of print].
Presented by Dr. Deepak L. Bhatt at the American College of Cardiology Virtual Annual Scientific Session (ACC 2021), May 17, 2021.
Bhatt DL, Szarek M, Steg PG, et al., on behalf of the SOLOIST-WHF Trial Investigators. Sotagliflozin in Patients With Diabetes and Recent Worsening Heart Failure. N Engl J Med 2021;284:117-28.
Editorial: Brosius FC, Vandvik PO. Cardioprotection With Yet Another SGLT2 Inhibitor — An Embarrassment of Riches. N Engl J Med 2021;384:179-81.
Presented by Dr. Deepak Bhatt at the American Heart Association Virtual Scientific Sessions, November 16, 2020.
Clinical Topics: Arrhythmias and Clinical EP, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, Atrial Fibrillation/Supraventricular Arrhythmias, Lipid Metabolism, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Vascular Medicine
Keywords: ACC21, ACC Annual Scientific Session, AHA20, AHA Annual Scientific Sessions, Atrial Fibrillation, Diabetes Mellitus, Type 2, Diuretics, Heart Failure, Metabolic Syndrome, Natriuretic Peptide, Brain, Patient Discharge, Secondary Prevention, Sodium-Glucose Transporter 2, Stroke Volume
< Back to Listings