SOGALDI-PEF: Dapagliflozin Plus Spironolactone More Effective Than Monotherapy
In patients with heart failure with mildly reduced or preserved ejection fraction (HFmrEF/HFpEF), the combination of dapagliflozin plus spironolactone led to a greater reduction in NT-proBNP levels than dapagliflozin alone, indicating improved cardiac stress, according to results from the SOGALDI-PEF trial published in JACC.
In the prospective, randomized, open, blinded endpoint crossover trial, João Pedro Ferreira, MD, PhD, et al., recruited 108 outpatients (median age 76 years; 57% women) from two Portuguese clinics with symptomatic HF (NYHA functional class II-IV), an LVEF >40% and evidence of structural heart disease. Among participants, median NT-proBNP was 746 pg/mL and a median Log transformed NT-proNP, the primary outcome, of 6.6 Log units. Their median eGFR was 72 mL/min/1.73m2 and serum potassium was 4.3 mmol/L; 45% had diabetes.
The patients were randomized to six different sequences for three periods of 12 weeks of dapagliflozin monotherapy, spironolactone monotherapy and combination therapy. The starting doe for dapagliflozin was 10 mg/day and for spironolactone it was 25 mg every other day if the baseline estimated glomerular filtration rate (eGFR) was <60 mL/min/1.73m2 or if eGFR was ≥60 mL/min/1.73m2 and serum potassium 5.0-5.5 mmol/L. If the eGFR was ≥60 mL/min/1.73m2 and serum potassium was <5.0 mmol, the daily dose of spironolactone was 25 mg.
Of note, spironolactone monotherapy was stopped early in the study, due to the confirmed benefits of SGLT2 inhibitors like dapagliflozin for patients.
Results showed that dapagliflozin/spironolactone reduced LogNT-proBNP levels by – 0.11 (p=0.035), a relative reduction of 11% compared to dapagliflozin alone, increasing the odds of reaching ≥20% NT-proBNP reduction (odd ratios, 2.27; p=0.016).
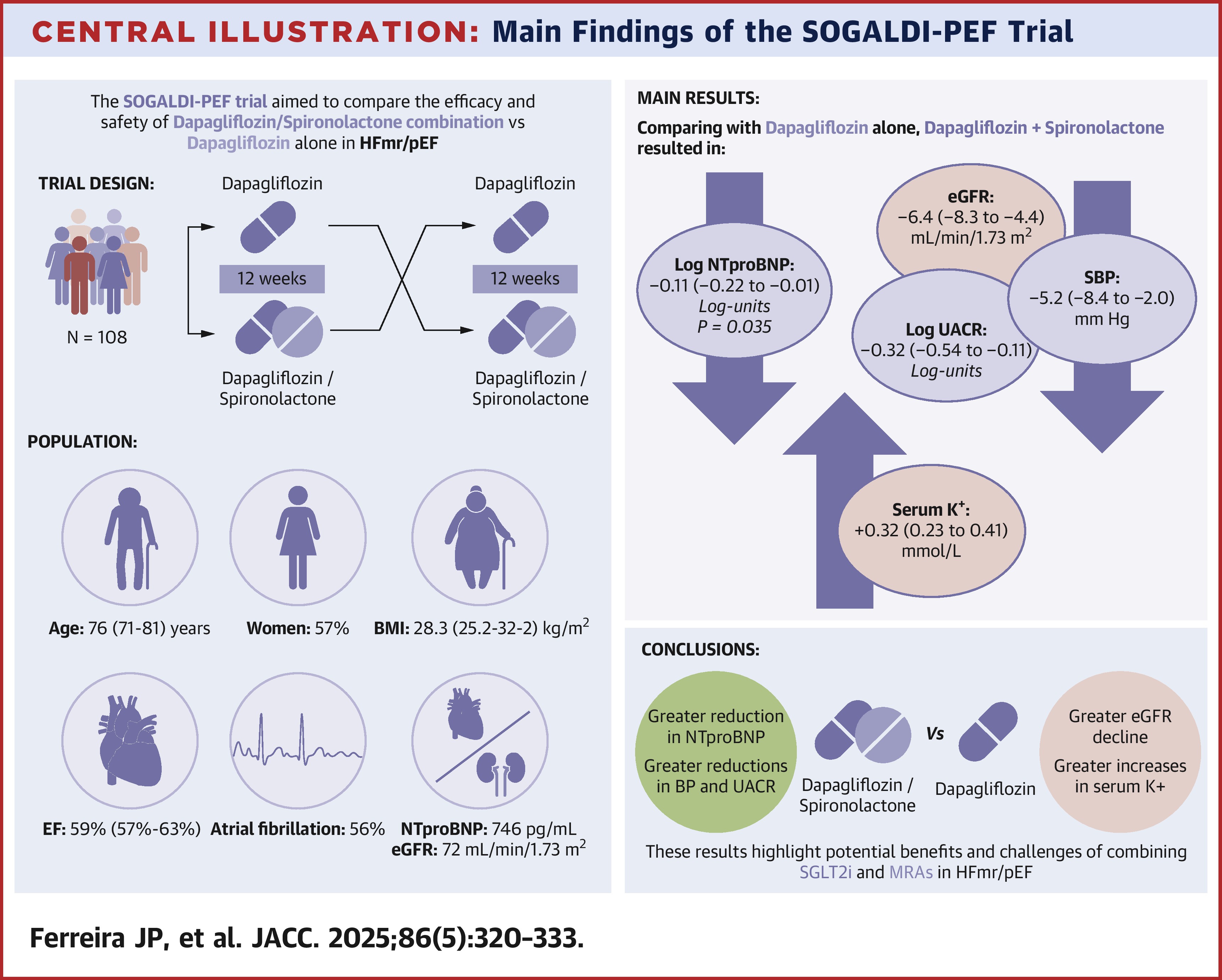
For safety outcomes, combination therapy decreased eGFR (–6.4mL/min/1.73m2) and increased serum potassium (+0.32 mmol/L), as well as reduced Logurinary-albumin-to-creatinine ratio (–0.32 Log) and increased the frequency of serum potassium >5.5 mmol/L: 5 [4.8%] vs. 1 [0.9%], and reduced systolic blood pressure (–5.2 mm Hg). Hyperkalemia, worsening kidney function and hypotension all occurred more frequently in combination therapy than with dapagliflozin alone.
"It is well-established that both [SGLT2 inhibitors] and [mineralocorticoid receptor agonists] produce an early eGFR decline that may last up to 12 weeks," write the authors, "but our study suggests that the eGFR decline is additive when using the [two] agents combined."
In an accompanying editorial comment, Muthiah Vaduganathan, MD, MPH, and Brendon L. Neuen, MBBS, MSC, PhD, stress the need for caution when evaluating patients for combination therapy. "Aligning treatment to absolute risk, minimizing therapeutic inertia, and addressing polypharmacy through high-value prescribing are now central to clinical care," they write. "SOGALDI-PEF2 contributes an important piece to this implementation puzzle, helping us refine how we deploy combination therapy to optimize outcomes for our patients and for population health alike."
Clinical Topics: Heart Failure and Cardiomyopathies, Acute Heart Failure
Keywords: Spironolactone, Heart Failure, Mineralocorticoid Receptor Antagonists, Sodium-Glucose Transporter 2 Inhibitors, Polypharmacy, Hyperkalemia, Glomerular Filtration Rate
< Back to Listings
