Study Sheds Light on Journey From HFrEF to HFimpEF
With the prevalence of heart failure with improved ejection fraction (HFimpEF) expected to increase as new treatments for heart failure with reduced ejection fraction (HFrEF) become more broadly available, findings from a new study published in JACC suggests a need for further research to optimize sustained guideline-directed medical therapy (GDMT) adherence and therapeutic strategies and to better personalize care models in this patient group.
"Although HFimpEF is associated with improved clinical outcomes, compared with persistent HFrEF, the residual burden of morbidity and mortality remains significant," write Kyung H. Min, MD, and colleagues, who studied the rates of worsening HF events and death in approximately 30,000 patients diagnosed with incident HFrEF between January 2013 and December 2022 across the Kaiser Permanente Northern California health system. Of these participants, roughly 8,600 experienced HFimpEF within 12 months of HFrEF diagnosis.
Overall results showed that use of GDMT "marginally decreased" across most medication categories during the study period after incident HFimpEF. Compared with patients with HFrEF, rates of worsening HF were fewer among patients with HFimpEF (17.4 per 100 person-years vs. 34.1 per 100 person-years). Rates of death were also fewer in the HFimpEF group (5.7 per 100 person-years vs. 11.0 per 100 person-years).
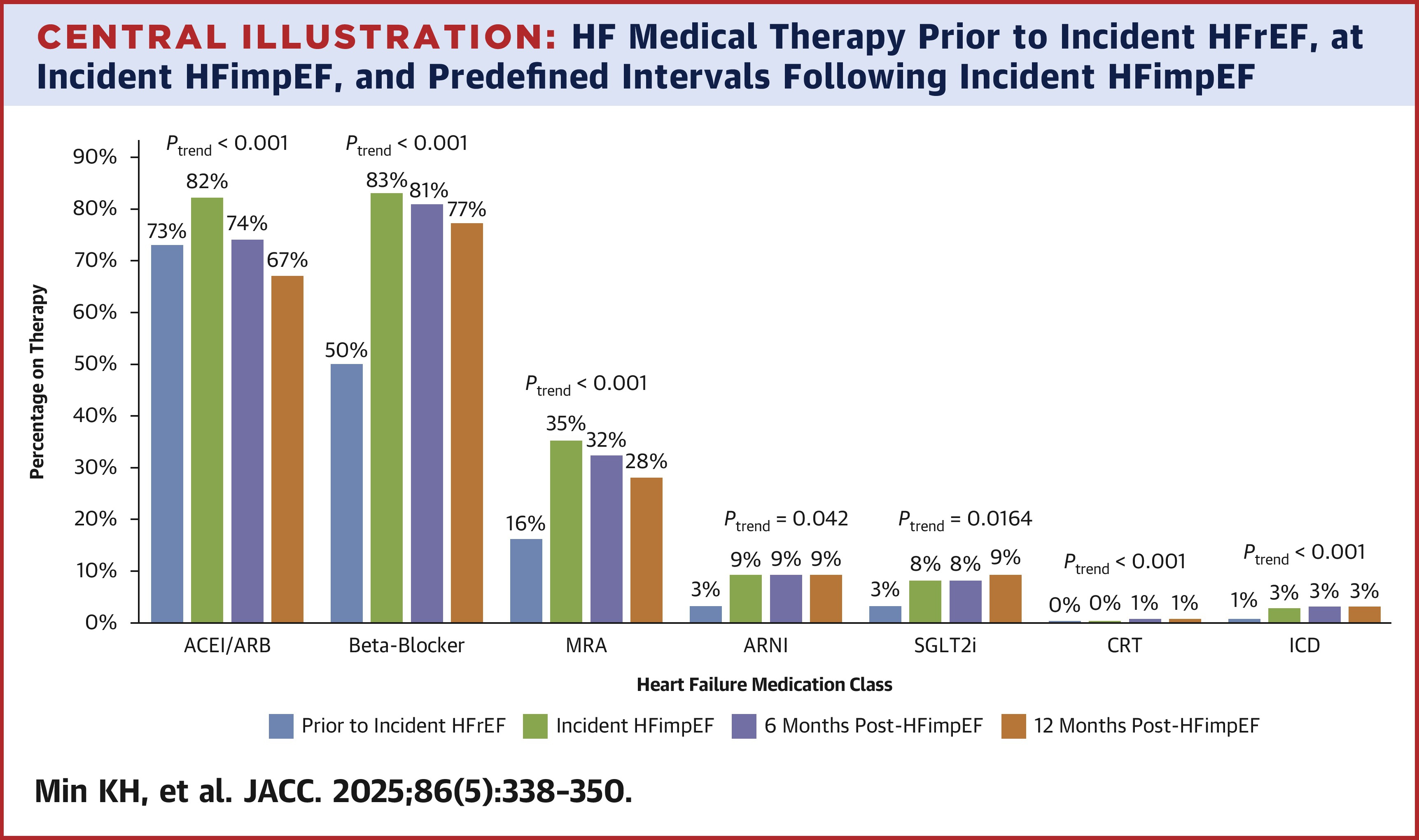
In other findings, study investigators noted that those patients who experienced incident HFimpEF were generally younger and with fewer comorbidities. They also highlighted that while GDMT improved from the time of incident HFrEF to HFimpEF, it declined over 12 months following improvement in EF. This withdrawal of GDMT was modestly associated with greater clinical risk.
"Given the continued clinical risk faced by patients with HFimpEF, prospective trials in HF should enroll patients with HFimpEF to better understand whether incremental pharmacotherapy may provide additional risk reduction in this common and understudied population," said Kim, et al. "In addition, implementation science efforts to prioritize sustaining medical therapy in this population are needed."
In a related editorial comment, Andrew S. Perry, MD, and Lynne Warner Stevenson, MD, FACC, applaud the study for illuminating the journey to and from HFimpEF in a large, diverse U.S. population. "The journey to improvement will hopefully include new lanes as GDMT continues to evolve beyond traditional triple therapy," they write.
Clinical Topics: Heart Failure and Cardiomyopathies, Acute Heart Failure
Keywords: Implementation Science, Heart Failure
< Back to Listings
