New Scientific Statement Deep Dives Into Risk Assessment For Guiding Blood Pressure Management
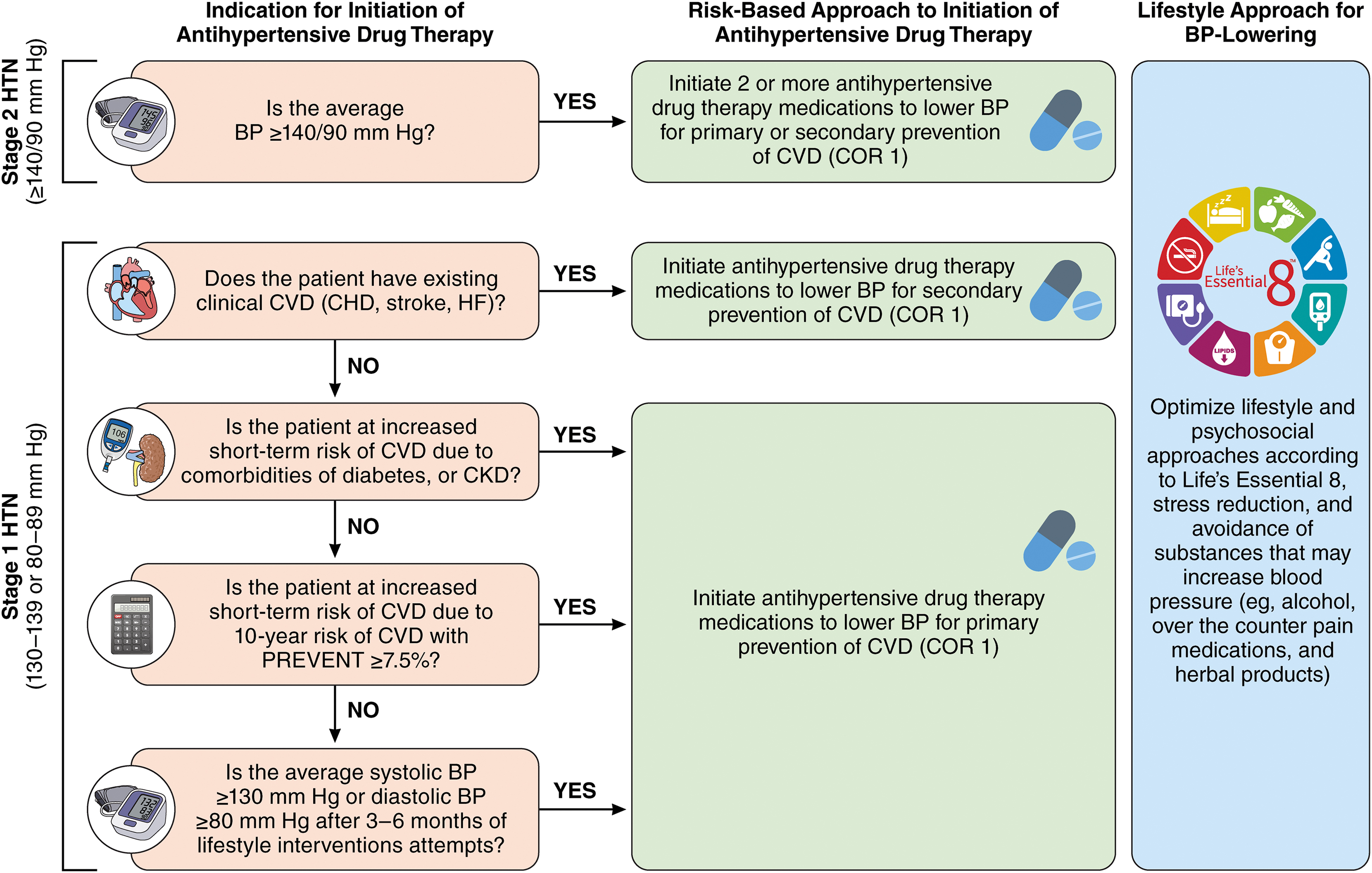
Following the release of the updated 2025 multisociety High Blood Pressure Guideline, which redefines how cardiovascular disease risk is assessed and managed in adults, a new ACC/AHA Scientific Statement introduces the PREVENT model (Predicting Risk of Cardiovascular Disease Events) and details the supporting evidence and rationale behind its use.
The use of the PREVENT risk calculator to estimate cardiovascular disease risk and guide drug treatment vs. use of pooled cohort equations is one of the biggest changes in the 2025 guideline. PREVENT, which combines measures of cardiovascular, kidney and metabolic health, delivers more precise estimates of 10-year risk of total cardiovascular disease (including atherosclerotic cardiovascular disease and heart failure).
"The PREVENT equations provide an important advancement in accurate and precise CVD risk prediction and therefore improve the identification of individuals for risk-based hypertension management," write Sadiya S. Khan, MD, MSC, FACC, chair of the Scientific Statement Writing Committee, Vice Chair Donald M. Lloyd-Jones, MD, SCM, FACC, et al.
In addition to providing evidence of the PREVENT model's benefits, including recent clinical trial data, the Scientific Statement addresses the population-level implications of the recommended new risk threshold of ≥7.5% for initiation of antihypertensive therapy in patients with stage 1 hypertension. The authors also offer practical advice and best practices for implementing risk assessment as part of the comprehensive approach to hypertension management.
"Remaining gaps in awareness and treatment of hypertension underscore the need for innovative strategies to improve implementation of and adherence to risk-based guideline recommendations, including automation of risk assessment in electronic health records, decision-support aids, and refinement of risk assessment to equitably improve the initiation of antihypertensive drug therapy, blood pressure control, and outcomes," the authors write.
They urge continued efforts to further evaluate the generalizability of PREVENT in datasets and settings not included in the original development, including Hispanic and Asian communities and outside the U.S. They also note that future studies should assess the impact of social drivers of health (SDOH), pregnancy and other risk-enhancing factors in context with PREVENT.
Meanwhile, with blood pressure (BP) continuing to make headlines, two new studies published in the Annals of Internal Medicine provide more food for thought on the cost-effectiveness of intensive BP targets and agreement between different types of blood pressure monitoring (BPM), respectively.
In the first study, Karen C. Smith, PhD, Thomas A. Gaziano, MD, FACC, and colleagues evaluated the impact of measurement error on the cost-effectiveness of intensive systolic blood pressure (SBP) targets in SPRINT-eligible patients at high cardiovascular risk without diabetes or prior stroke. Their findings showed that a target of <120 mm Hg seemed to be cost-effective and "may provide good value in many clinical settings," with the exception of scenarios with high measurement error (≥14.6 mm Hg in the <120 mm Hg target), higher-than-expected cardiovascular risk at low SBPs, and higher-than-expected disutility from antihypertensive medications.
In the second study, Jiunn-Tyng Yeh, MD, PhD, Chi-Jung Huang, PhD, et al., conducted a systematic review and network meta-analysis comparing and evaluating different monitoring methods across varying BP levels. "Our study has two important clinical implications," they said. "First, we provide estimated values for each BPM technique across different BP ranges, which can help selection of treatment targets or diagnostic thresholds in clinical practice and when designing clinical trials. Second, we showed that the differences among BPM methods are not fixed but instead depend on the underlying SBP and DBP."
In a related editorial, Gregory Murphy, MB BCh, and John W. McEvoy, MB BCh, MHS, PhD, say the two new studies provide important new knowledge about the modern landscape of hypertension management. "We hope that these data will help alleviate clinicians' hesitancy to embrace lower BP targets," they write.
Citations:
- Khan, S, Lloyd-Jones, D, Abdalla, M. et al. Use of Risk Assessment to Guide Decision-Making for Blood Pressure Management in the Primary Prevention of Cardiovascular Disease: A Scientific Statement From the American Heart Association and American College of Cardiology. J Am Coll Cardiol. Published Aug. 28, 2025. doi:10.1016/j.jacc.2025.08.001
- Smith KC, Gaziano TA, Mushlin AI, Cutler DM, Menzies NA, Pandya A. Effect of Systolic Blood Pressure Measurement Error on the Cost-Effectiveness of Intensive Blood Pressure Targets. Ann Intern Med. Published online August 19, 2025. doi:10.7326/ANNALS-25-00560
- Yeh JT, Huang CJ, Lee CW, et al. Agreement Between Different Types of Blood Pressure Monitoring : A Systematic Review and Network Meta-analysis. Ann Intern Med. Published online August 19, 2025. doi:10.7326/ANNALS-24-02142
Clinical Topics: Prevention, Hypertension
Keywords: Antihypertensive Agents, Heart Disease Risk Factors, Blood Pressure, Cost-Benefit Analysis, Hypertension
< Back to Listings
