Feature | The Implications of Technology on Echocardiography Education

Over the last few decades, we have witnessed the exponential growth of technology, from the Commodore 64 of the 1980s to the iPhones and Androids held in our white coat pockets today. As medicine educators in the digital age, we have a tremendous opportunity to incorporate new computer-based programs into our lessons both in the classroom and at the bedside.
In some respect, it is also our responsibility to understand the benefits and limitations of the devices at our disposal. Equipped with this knowledge, we can then determine the most effective way for new technology to be applied in the clinical setting and employed as teaching tools for our trainees.
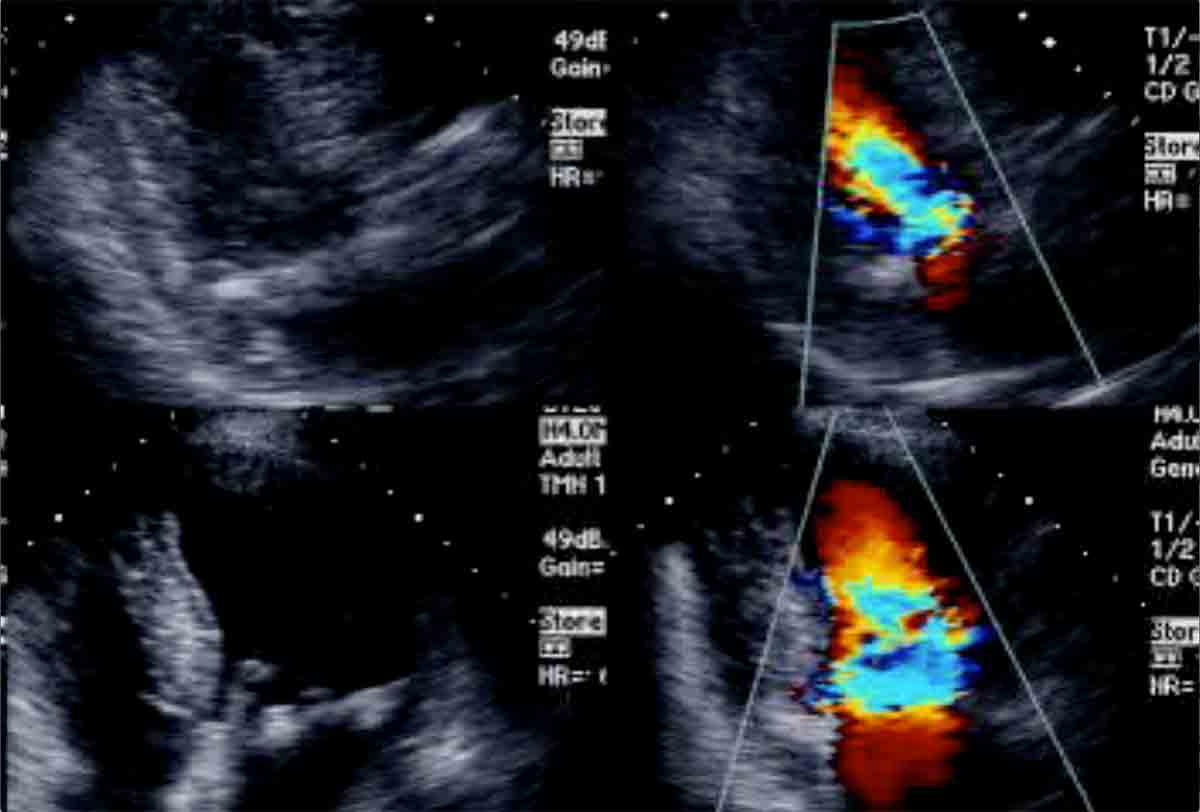
In the area of echocardiography, there has been significant development of ultrasound-based instruments to aid in the performance and interpretation of both transthoracic and transesophageal echocardiograms.
While there is significant interest in how this equipment can make clinical practice more efficient and productive, there is also a valuable educational component embedded in the programs and devices available. Specifically, handheld ultrasound, echocardiography simulators and deep learning systems are at the frontier of modern-day echocardiography education.
Handheld Ultrasound

Handheld devices revolutionized point of care ultrasound (POCUS) for cardiologists and non-cardiologists alike. Between 2007 and 2009, Siemens and General Electric unveiled their versions of pocket-sized ultrasound units — the Acuson P10 and the Vscan, respectively. Later in 2015, Philips introduced the Lumify transducer, which can be connected to a cell phone and used with an app to obtain 2-D and color Doppler images.
These “mini devices” have made the cardiac ultrasound more widely and readily available to physicians to answer focused, qualitative questions: Is there a pericardial effusion? Is the LV function normal or abnormal? While the pre-requisite training to accurately acquire and interpret POCUS images in clinical practice remains variable and uncertain, there is now both a desire and need to develop an ultrasound curriculum for medical students and trainees.
Amer M. Johri, MD, MSc, et al., recently published a review in the Journal of the American Society of Echocardiography on POCUS in medical school education. The American Society of Echocardiography (ASE) recommends that the core components of POCUS training include didactic lessons in fundamental ultrasound concepts, hands-on scanning practice and experience with image interpretation.
The review also suggests an approach to integrate ultrasound education into the medical school curriculum; first as a tool to demonstrate anatomy and physiology, then as a complement to the study of pathology, and finally as an adjunct to the physical exam in the clinical setting.
As the technology of handheld devices progresses, ultrasound will be used more frequently in a focused manner across medical specialties. This is particularly true when considering the utility of focused ultrasound to diagnose cardiac disease in a variety of clinical settings, from the emergency department to the intensive care unit.
While handheld devices afford us the opportunity to enhance our use of bedside ultrasound, they have also exposed the need for significant education and training in POCUS so that it can be used with sufficient diagnostic accuracy across a broad clinical spectrum. As cardiology educators, we are at the forefront of this developing technology, strategizing how best to incorporate POCUS into medical education and training so that it can be used as a complementary tool in clinical decision-making.
Simulation-Based Training
Transesophageal echocardiography (TEE) is an integral diagnostic modality with a growing number of clinical applications, due in part to the rapid development of transcatheter devices. As such, there is an increasing desire among cardiology trainees to become proficient in TEE.
While there is certainly a need to demonstrate competence in the live procedural setting, there can also be clinical and logistical limitations to traditional TEE training, including an untrained operator that may pose a small but significant risk to the patient; the volume of TEEs at a given institution that may not be sufficient to meet the demand for TEE training among cardiology fellows; and limitations of procedural times and availability of supervising physicians that may pose barriers to learning. These obstacles can be mitigated with the use of TEE simulation.
This model has been used in a variety of medical and surgical sub-specialties with positive results. According to a study published in the Journal of Thoracic and Cardiovascular Surgery, Jeremy Smelt, MRCS, et al., demonstrated that on pre- and post-intervention testing, cardiothoracic surgery residents assigned to TEE simulation performed as well as counterparts who were taught TEE during elective cardiac surgery.
There is also compelling data on how simulation can be used in a complementary fashion to standard TEE training. According to a study published in the Journal of the American Society of Echocardiography, Julie B. Damp, MD, FACC, et al., demonstrated that cardiology fellows introduced to simulator-based training along with a traditional TEE curriculum achieved higher total scores on a post-training transesophageal echo assessment than fellows who followed the traditional TEE curriculum alone.
While accessibility and cost of simulation-based equipment and software are obvious drawbacks to the widespread implementation of TEE simulators, there are clear benefits to acquiring procedural skill in a controlled environment without the risk of causing harm to patients.
Deep Learning Systems
Artificial Intelligence, and more specifically deep learning, is a hot topic in the technology world. According to the CloudFactory blog, improved computer processing power, massive digital datasets, and better algorithms are the forces that have paved the way for the Artificial Intelligence technology boom.
In an MIT Technology Review article, Robert D. Hof explains that deep learning software attempts to mimic the neural networks in our brains by learning to recognize patterns in digital representations of data. With respect to echocardiography and through similar pattern recognition, deep learning technology is being developed to acquire and interpret standard echo views. In fact, Bay Labs recently received US FDA 510(k) clearance for its EchoMD AutoEF algorithm that provides fully automated clip selection and calculation of LV ejection fraction.
“What is really unique is the ability of these deep machine neural networks to learn over time when presented with a vast amount of data, or in the case of echocardiography, hundreds of thousands of echocardiograms,” Randolph P. Martin, MD, FACC, past president of the ASE, emeritus professor at Emory University Medical School, and chief medical officer of Bay Labs writes. “This allows the machine learning systems to provide assistance in interpretation.”
While it is unlikely that computer systems will completely replace the echo-trained cardiologist, there is real potential for artificial intelligence to enhance the overall quality and accessibility of echocardiography through standardization and optimization of image acquisition and interpretation.
There is little data on how Artificial Intelligence can be applied to echocardiography education, although one can imagine how deep learning models could serve as a valuable teaching tool, particularly for early learners. Currently, many cardiology fellows acquire transthoracic echo skills by shadowing technicians.
This frequently leads to a variable learning experience, as there may be differences in technician experience, quality of teaching, and constraints in terms of technician time and availability. Deep learning software has the potential to provide fellows with a standardized, enhanced experience. The technology can be used to guide them to obtain appropriate views and be adapted as a modality to test or teach accurate interpretation of basic echo findings.
Martin also envisions the use of deep learning algorithms as a solution for diagnostic variability in the use of handheld devices for POCUS. He notes, “Imagine how machine learning algorithms and software embedded in ultrasound systems (even point of care or small hand held systems) ... can help with the acquisition and interpretation of echoes thereby improving the quality of the echo studies.”
While handheld ultrasound, simulation-based training and deep learning systems have not yet become the standard in echocardiography education, the future is bright. The power of technology has brought about both an exciting and challenging era, furnishing trainees with an innovative learning environment and calling upon clinician educators to determine how best to incorporate these novel modalities into modern medical education.

This article was authored by Kerry A. Esquitin, MD, FACC, director of the advanced echocardiography fellowship program and associate program director of the cardiology fellowship program at Columbia University Medical Center in New York.