Value-Based Payment For Newly Diagnosed Atrial Fibrillation
Value-based payment (VBP) models are intended to promote delivery of high-quality care and favorable outcomes with reasonable expenses. VBP, as the larger quality strategy of the Centers for Medicare & Medicaid Services, is intended to move towards physician payments based on quality rather than quantity of care.
The VBP model of bundled payments is about shared savings. Under this structure, health care providers receive a fixed amount of money to treat a patient either for a specific condition or within a certain period. If the provider can treat the patient for less than the fixed amount provided, they're entitled to a share of the surplus for the terms of their contract. If their cost exceeds a fixed amount, then the provider misses out on the opportunity for reimbursement they could have had under traditional reimbursement models.
Past VBP models related to cardiovascular practice have been mostly targeted to specific conditions and procedures. Now the focus has gradually shifted to application of the VBP model to chronic cardiac conditions.
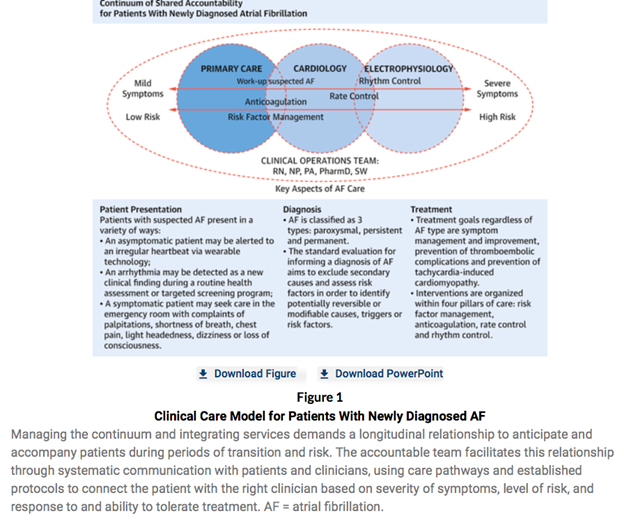
In the December issue of the Journal of the American College of Cardiology, Casale et al. describe how the VBP model could be utilized for newly diagnosed atrial fibrillation (AF), a common diagnosis predicted to increase significantly in prevalence in the coming years. AF affects a heterogenic population with an obvious need for multidisciplinary collaboration for the delivery of high-quality care. Often, primary care disciplines such as internal medicine and family medicine are involved in the detection of new onset AF, while cardiology and electrophysiology (EP) teams are tasked with the necessary medical therapy for heart rate control and/or advanced therapies (e.g., ablation) for rhythm control. A clinical operations team comprised of registered nurses, nurse practitioners, physician associates, clinical pharmacists and social workers is needed to facilitate access to the systems as well as navigate the patient through primary care, cardiology and EP services (Fig 1).
Casale et al. stress that this delivery model will be aimed at integrated delivery of guideline-supported therapies and reduction of disparate care through adherence to care pathways. Accountability for this care delivery would rest with both primary care and cardiology. As shown in the schematic diagram (Fig 1), certain aspects of care, such as risk factor modification and initiation of anticoagulation, could be started at the primary care level, while use of antiarrhythmic agents and ablative therapies are managed by cardiology or EP services. The outcomes would be defined by four pillars: Risk factor modification, initiation of anticoagulation, rate control therapies and rhythm control therapy. This model is complementary to the concept of AF Centers of Excellence, promulgated by the Heart Rhythm Society.
While VBPs ideally would provide better care for the patient at a reduced cost, it has several challenges. Considerable amount of practice resources are initially needed to monitor the processes. Shared savings programs also don't always reimburse related services outside of direct care (e.g., communications with patient's previous providers, consultations, nursing care, etc.)
It is obvious that many details of VBP for AF care that serve the needs of different types of healthcare systems need to be worked out. But this informative conceptual paper is indicative of the future of VBP models for chronic cardiovascular conditions.
This article was co-authored by Chittur A. Sivaram MBBS, FACC, and Toniya Singh MBBS, FACC.
This content was developed independently from the content developed for ACC.org. This content was not reviewed by the American College of Cardiology (ACC) for medical accuracy and the content is provided on an "as is" basis. Inclusion on ACC.org does not constitute a guarantee or endorsement by the ACC and ACC makes no warranty that the content is accurate, complete or error-free. The content is not a substitute for personalized medical advice and is not intended to be used as the sole basis for making individualized medical or health-related decisions. Statements or opinions expressed in this content reflect the views of the authors and do not reflect the official policy of ACC.