A Nudge Towards Cardiovascular Health
Cardiovascular disease (CVD) remains the leading cause of mortality and morbidity in the United States1 and globally, despite the widespread availability of highly evidence-based therapies intended to prevent and treat it. Time and again, we see these therapies, ranging from guideline-directed medical therapy in heart failure2 to cardiac rehabilitation in ischemic heart disease3, are underutilized in inequitable fashion. Why is this? Ultimately, human behavior, particularly the behavior of patients and health care teams, is the final common pathway through which therapies reach patients. This gives rise to the need for the design and evaluation of deliberate strategies to modify or nudge human behavior to achieve optimal health outcomes and groups embedded in health care systems focused on doing so.
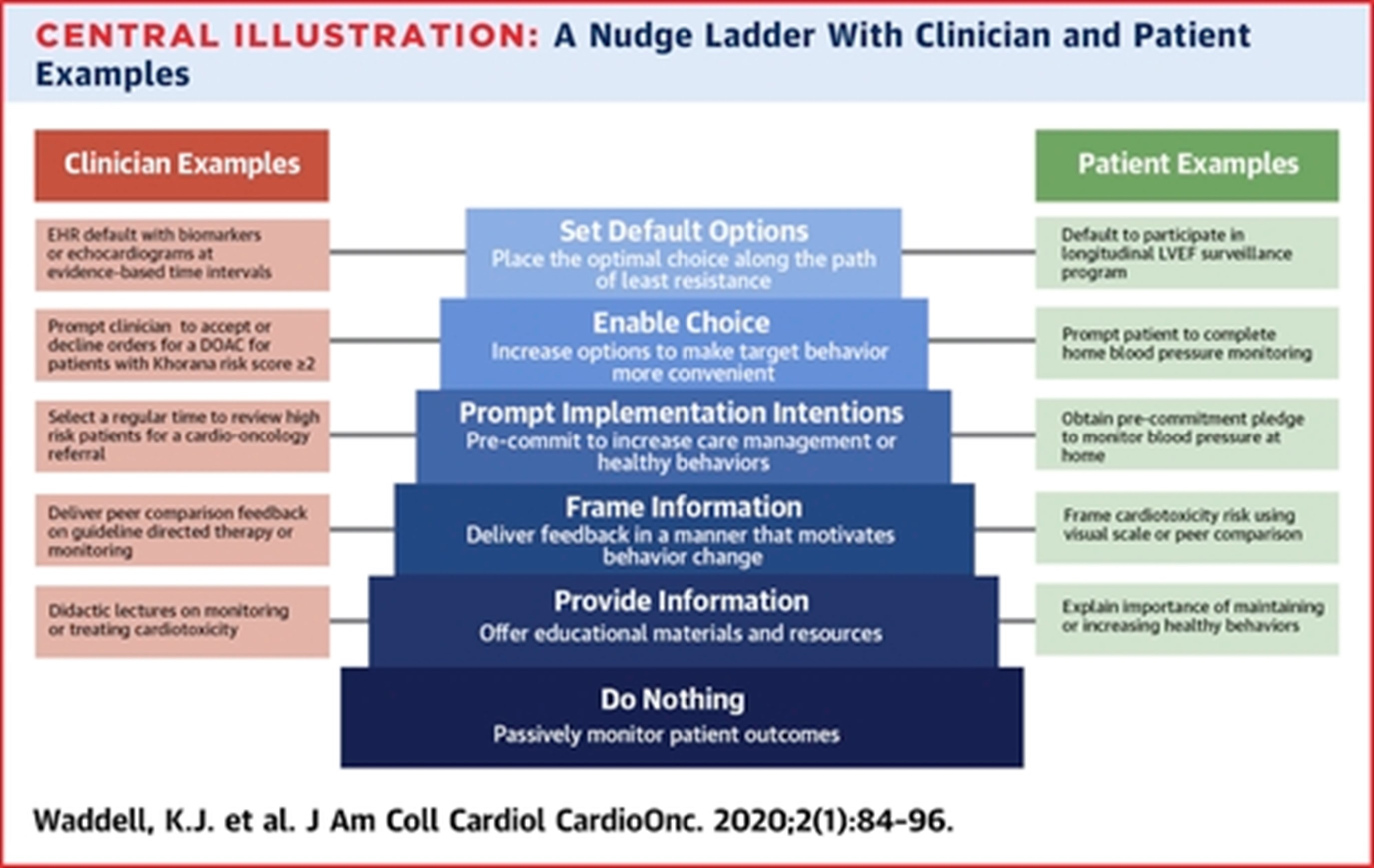
Simply put, a nudge is a change in the way choices are presented or information is framed that is meant to guide or motivate decision-making. The theory behind nudging originates from behavioral science, or the study of human behavior, as well as implementation science, which promotes the uptake of evidence-based practices at scale in healthcare. Optimal targets for nudges are situations in which patients, clinicians, or others on the care team who are critical to good outcomes don't make the right choice, or it's just too hard or inefficient to make the decision that achieves optimal health. The increased prevalence of patient and health care team-facing digital choice environments, such as the electronic health record and patient portals, has given rise to a variety of platforms to nudge individuals and methods through which to capture data on effectiveness of those strategies. Ideal nudges prompt and motivate decision-making and focus on simplifying the decision-making process or choice environment (i.e., the electronic health record), thereby making the right thing to do the easy thing to do4. If appropriately designed and, importantly, devised in conjunction with the group of individuals being nudged, nudges can be subtle changes in design that result in outsized positive impacts on human behavior.
Nudges have been studied in a variety of areas relevant to cardiovascular medicine. For example, implementing a pathway using the approach of default options5 increased clinician referral to cardiac rehabilitation by 47 percentage points sustained over time. As another example, financial incentives, when framed to patients as a loss rather than a gain and studied within the framework of a randomized clinical trial, significantly increased physical activity among patients with ischemic heart disease. Illustrations of additional potential nudges are shown in figure 1 and listed here. As the evidence base continues to develop around nudges and associated clinical use cases, consideration can be given to incorporating these behavioral change strategies into clinical guidelines as a method of translating evidence to practice.
Ultimately, to achieve our common mission of ensuring our patients receive guideline-directed care in equitable fashion and making it easy for clinicians to deliver that care, we need to focus on optimizing human behavior – and nudges towards cardiovascular health are one strategy to accomplish this.
References
- FastStats - Deaths and Mortality. Available at: https://www.cdc.gov/nchs/fastats/deaths.htm. Accessed March 9, 2022.
- Greene SJ, Butler J, Albert NM, et al. Medical Therapy for Heart Failure With Reduced Ejection Fraction: The CHAMP-HF Registry. Journal of the American College of Cardiology 2018;72:351–366.
- Sukul D, Seth M, Barnes GD, et al. Cardiac Rehabilitation Use After Percutaneous Coronary Intervention. J Am Coll Cardiol 2019;73:3148–3152.
- Behavior Model. behaviormodel. Available at: https://behaviormodel.org/. Accessed March 9, 2022.
- Adusumalli S, Jolly E, Chokshi NP, et al. Referral Rates for Cardiac Rehabilitation Among Eligible Inpatients After Implementation of a Default Opt-Out Decision Pathway in the Electronic Medical Record. JAMA Netw Open 2021;4:e2033472.
- Waddell KJ, Shah PD, Adusumalli S, Patel MS. Using Behavioral Economics and Technology to Improve Outcomes in Cardio-Oncology. JACC: CardioOncology 2020;2:84–96.
This article was authored by Srinath Adusumalli, MD, MSHP, MBMI, FACC, deputy director of Penn Medicine Nudge Unit.
This content was developed independently from the content developed for ACC.org. This content was not reviewed by the American College of Cardiology (ACC) for medical accuracy and the content is provided on an "as is" basis. Inclusion on ACC.org does not constitute a guarantee or endorsement by the ACC and ACC makes no warranty that the content is accurate, complete or error-free. The content is not a substitute for personalized medical advice and is not intended to be used as the sole basis for making individualized medical or health-related decisions. Statements or opinions expressed in this content reflect the views of the authors and do not reflect the official policy of ACC.