A 17-year-old male with no past medical history presented to the emergency department (ED) with acute onset, sharp, substernal non-radiating chest pain. The pain was worse with deep inspiration but was not positional. The patient's younger brother suffered from hand, foot, and mouth disease three weeks prior to symptom onset.
Vital signs were normal (T 36.9C, BP 133/72mmHg, HR 93 bpm, RR 13/min, SpO2 99% on room air).
Physical exam did not reveal any murmurs, rubs or gallops and the estimated jugular venous pressure was normal without increase in inspiration.
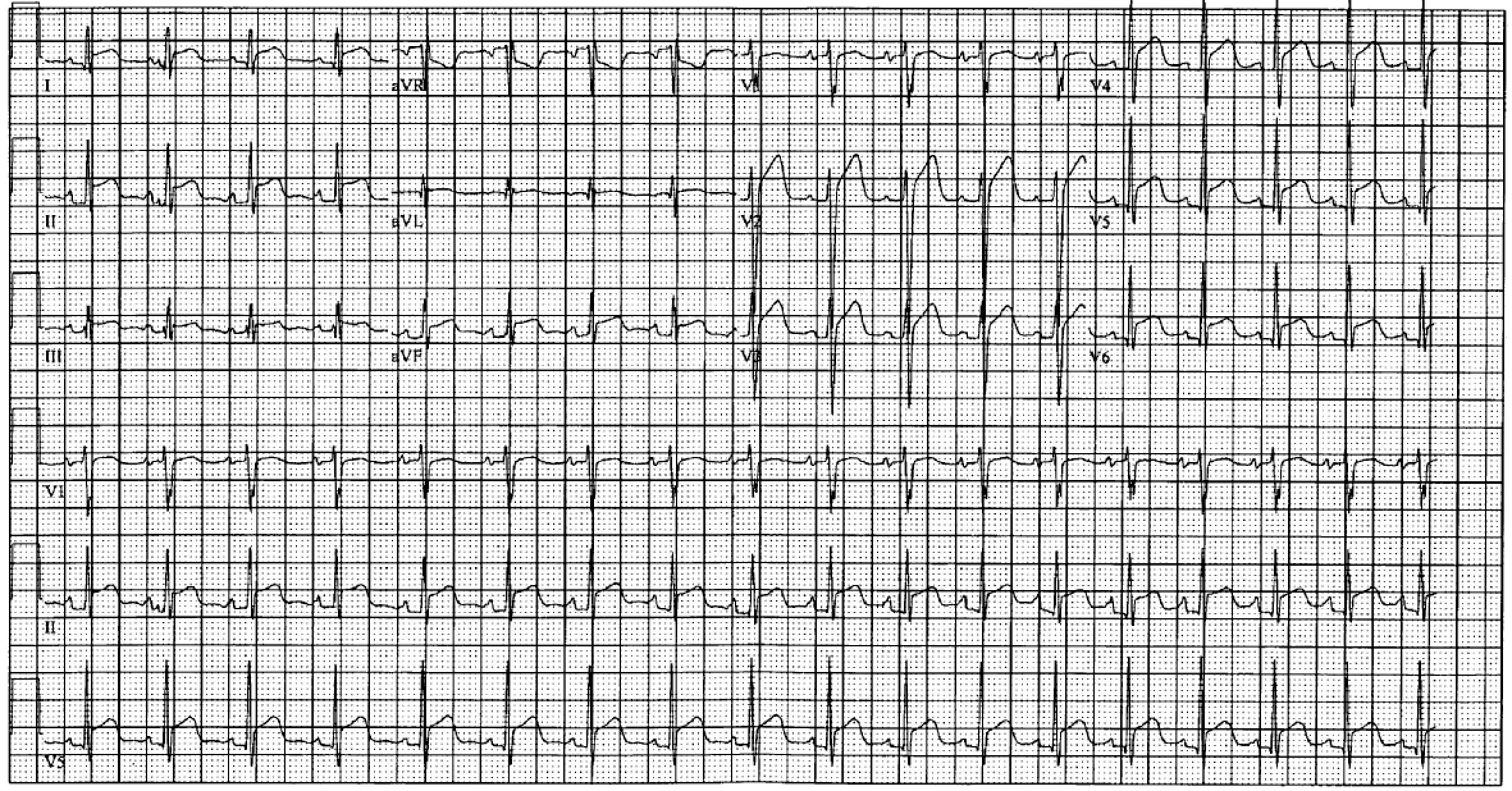
His presenting ECG showed diffuse ST elevations and PR depressions (Figure 1).
Troponin T was 0.03 ng/dl and WBC 9.0 k/ul.
A transthoracic echocardiogram (TTE) showed a small circumferential pericardial effusion and normal left ventricular function.
The diagnosis of acute pericarditis was made and the patient was discharged on ibuprofen 600mg TID and colchicine 0.6mg BID.
Figure 1
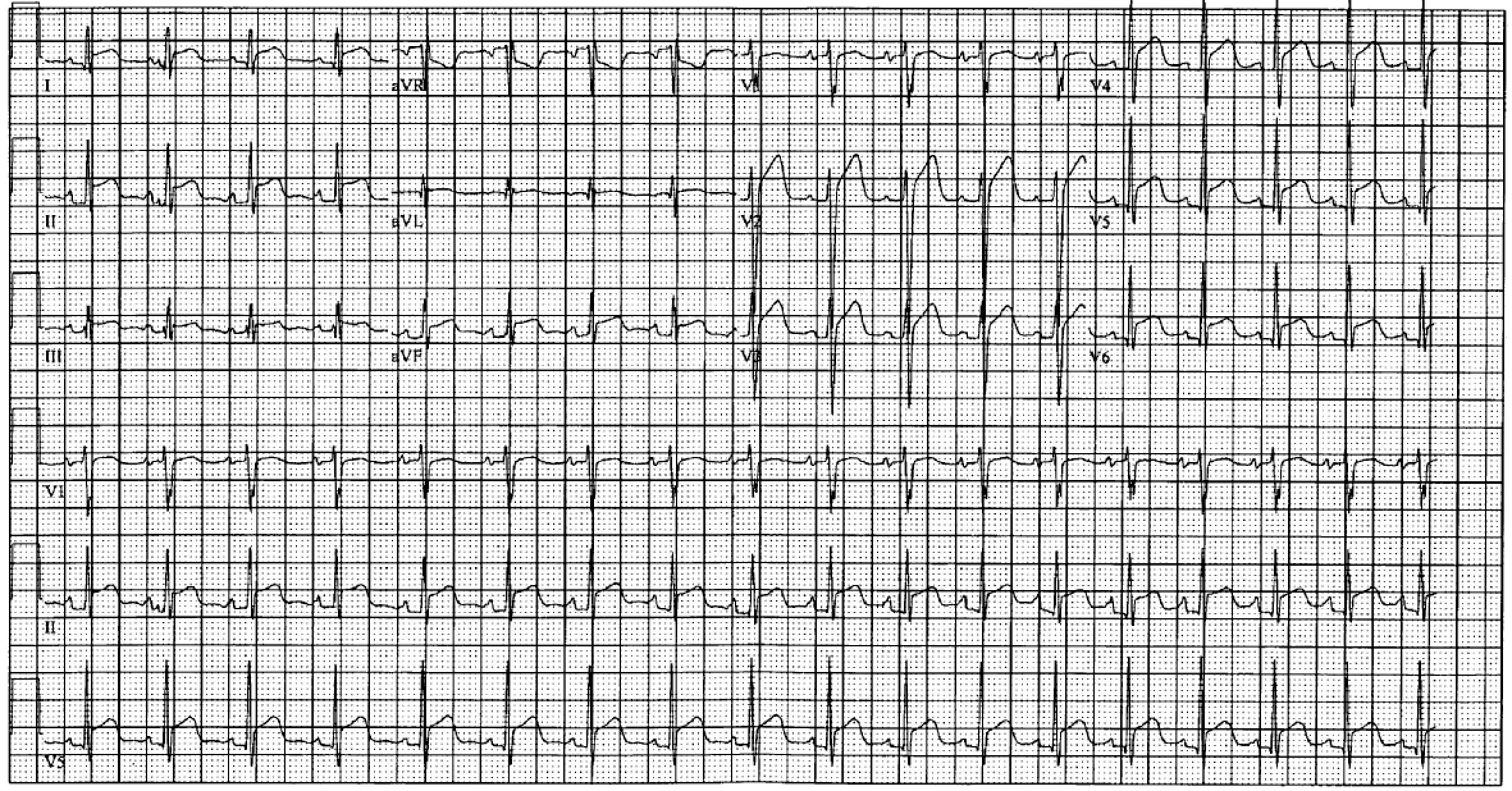 Figure 1. ECG showing diffuse ST elevations, PR depressions and PR elevation in aVR
Figure 1. ECG showing diffuse ST elevations, PR depressions and PR elevation in aVR
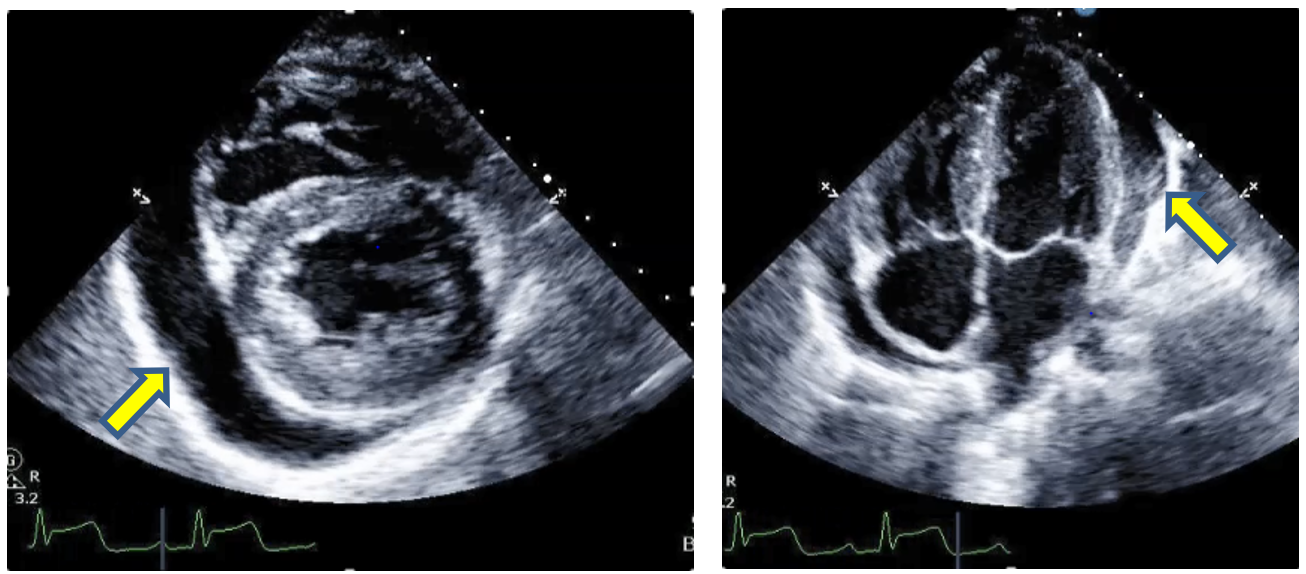
One week later he presented again to the ED with worsening chest pain and dyspnea. At that time the TTE showed worsening pericardial effusion (Figure 2). The patient underwent pericardiocentesis which yielded 400ml of exudative fluid. Gram stain, cultures and cytology were negative.
Figure 2
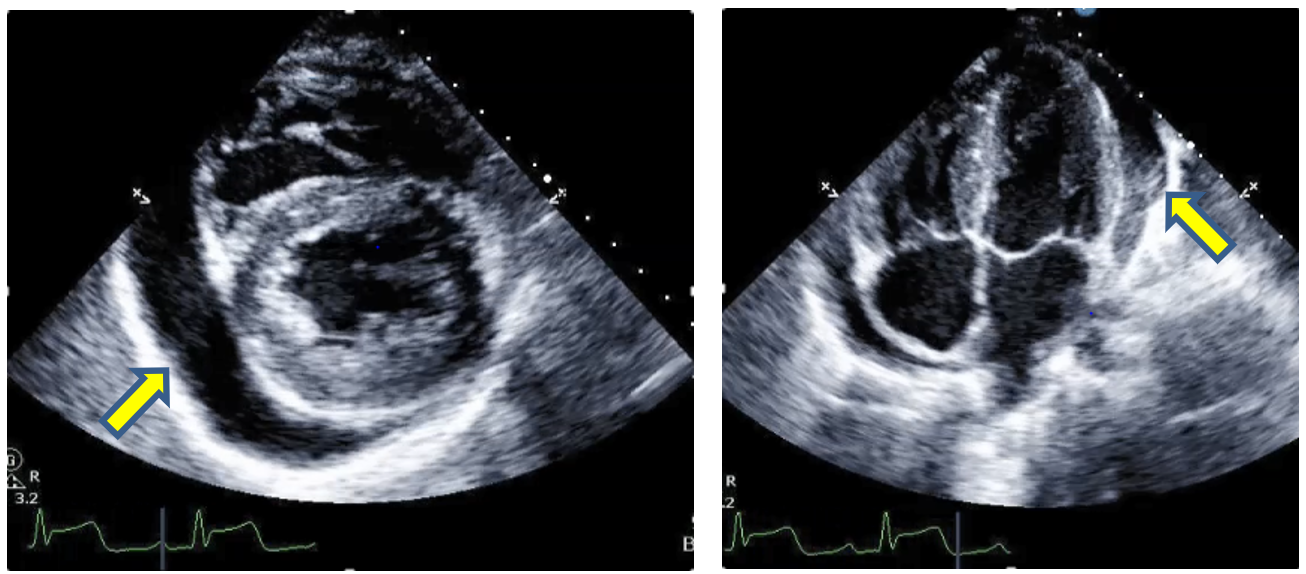 Figure 2. Transthoracic echocardiogram. Parasternal short axis at the level of papillary muscles (left) and apical 4-chamber view (right) showing a large circumferential pericardial effusion.
Figure 2. Transthoracic echocardiogram. Parasternal short axis at the level of papillary muscles (left) and apical 4-chamber view (right) showing a large circumferential pericardial effusion.
The patient was discharged on ibuprofen 800mg TID, colchicine 0.6mg BID and prednisone 40mg daily for two weeks with the instruction to taper the dose by 10mg every week. His symptoms resolved quickly within a week and he returned back to his activities, including swimming and cross country running.
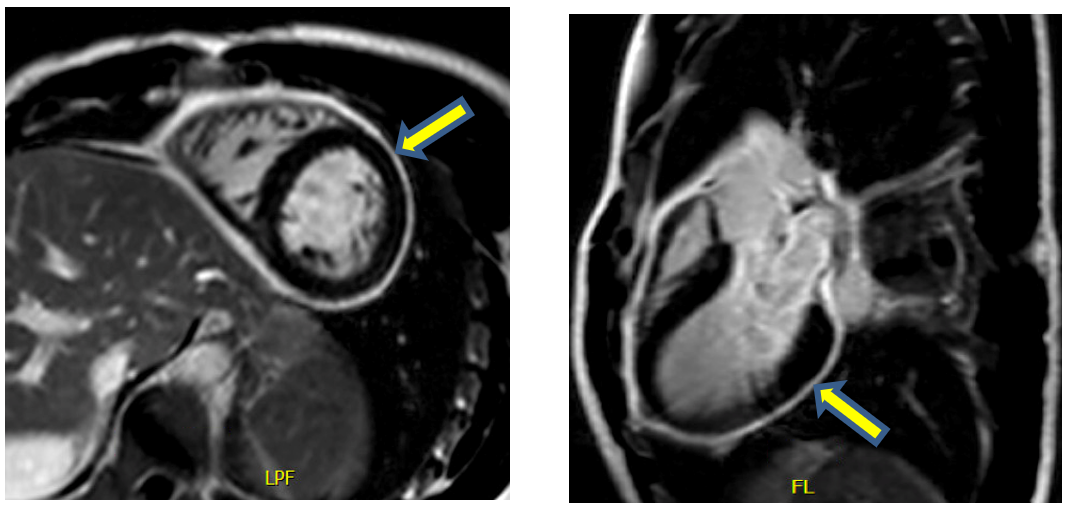
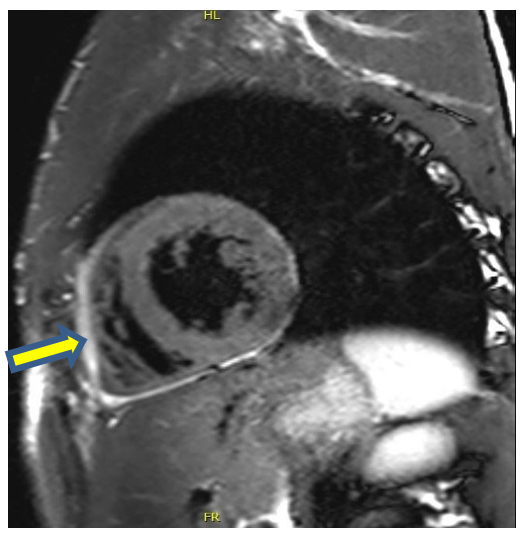
Shortly after the initiation of prednisone taper, the chest pain recurred, so the patient was referred to the Pericardial Clinic. At that time he reported pleuritic chest pain 3/10. Physical exam did not reveal any rubs, gallops, elevated JVP or Kussmaul sign. CRP was 6.3mg/dl (reference range 0.0-1.0mg/dl), ESR 21 mm/hr and Troponin T <0.01 ng/dl. A Cardiac MRI with gadolinium showed delayed gadolinium enhancement (Figure 3) as well as increased signal intensity on T2-STIR images (Figure 4).
Figure 3
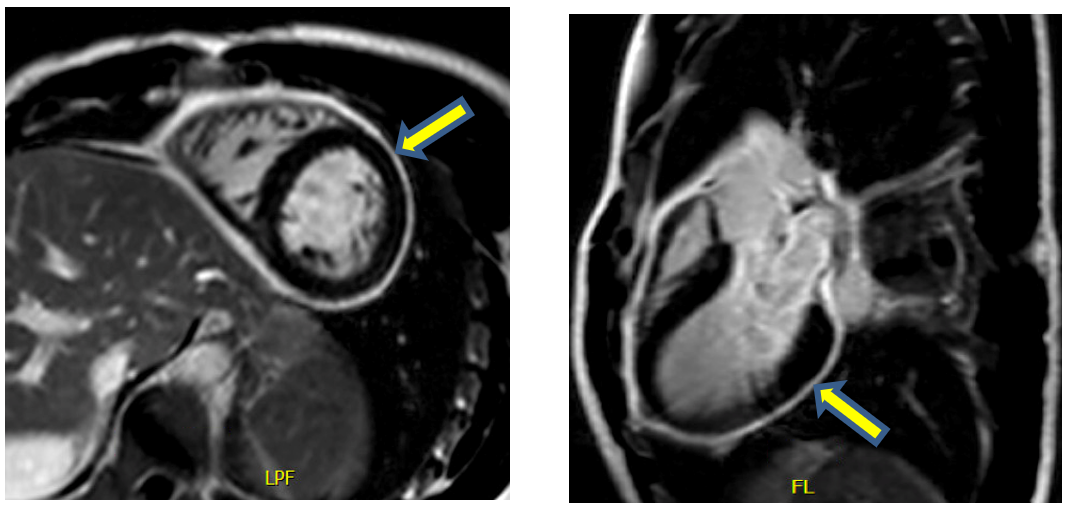 Figure 3. Cardiac MRI. Delayed gadolinium enhancement images showing diffuse pericardial enhancement.
Figure 3. Cardiac MRI. Delayed gadolinium enhancement images showing diffuse pericardial enhancement.
Figure 4
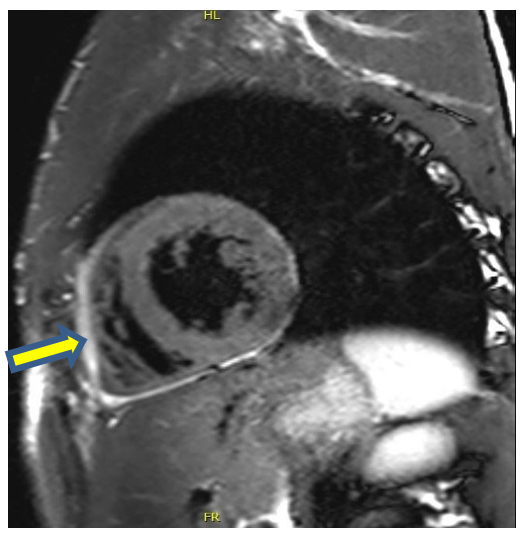 Figure 4. T2-STIR image showing increased signal mainly in the anterior portion of the pericardium.
Figure 4. T2-STIR image showing increased signal mainly in the anterior portion of the pericardium.
The correct answer is: B. Acute pericarditis.
The patient initially presented with symptoms and signs of acute pericarditis. Pericarditis remains a clinical diagnosis requiring two of the following four characteristics: 1) precordial chest pain that is worse with inspiration and when supine; 2) characteristic ST-segment elevation and PR deviation on electrocardiogram; 3) a pericardial friction rub; and 4) a pericardial effusion that is more than trivial. Supportive findings, although not included in the diagnostic criteria, include elevated inflammatory markers or other imaging evidence of pericardial inflammation.
Pericarditis is categorized according to the duration of symptoms. Pericarditis that persists for more than 4 to 6 weeks is termed incessant, and the presence of symptoms for >3 months is considered chronic pericarditis (D). If a patient is free of symptoms for at least 4 to 6 weeks, relapse is referred to as recurrent pericarditis (A).
In this case, the patient was having clinical symptoms of pericarditis for approximately 1 month and the symptom-free period was clearly less than 4 weeks, therefore the correct diagnosis is acute pericarditis.
Increased pericardial signal in T2 short-tau inversion-recovery (STIR) images on cardiac MRI is indicative of pericardial edema and active inflammation that is seen in the acute phase of pericarditis.
Late gadolinium enhancement of the pericardium is a sign of increased vascularity and angiogenesis secondary to pericardial inflammation and can be seen in all stages of pericarditis.
Besides the diagnostic value, the above MRI findings have also prognostic implications, as they are associated with the development of recurrent pericarditis and a more chronic course.
Myopericarditis (E) is used for cases of acute pericarditis that also demonstrate myocardial inflammation. Acute pericarditis and myocarditis often occur together, although they are rarely of equivalent intensity. In this case there is no biomarker or imaging evidence of myocardial involvement.
The term steroid-dependent pericarditis is used for cases when symptoms and other inflammatory findings recur during repeated attempts to taper and/or discontinue corticosteroid therapy. In this case, the symptoms recurred rather early and after the patient returned to his usual physical activities.
Finally, the clinical and imaging findings in this case do not support the diagnosis of constrictive pericarditis (F).
References
- Cremer PC, Kumar A, Kontzias A, et al. Complicated pericarditis: understanding risk factors and pathophysiology to inform imaging and treatment. J Am Coll Cardiol 2016;68:2311-28.
- Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) endorsed by: the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2015;36:2921-64.
- Kumar A, Sato K, Verma BR, et al. Quantitative assessment of pericardial delayed hyperenhancement helps identify patients with ongoing recurrences of pericarditis. Open Heart 2018;5:e000944.
- Kumar A, Sato K, Yzeiraj E, et al. Quantitative pericardial delayed hyperenhancement informs clinical course in recurrent pericarditis. JACC Cardiovasc Imaging 2017;10:1337-46.