Worsening Tricuspid Regurgitation Following Pericardiectomy: What is the Predictor?
A 75-year-old man with underlying disease of type 2 diabetes, hypertension, dyslipidemia, and a 10 pack-year history of smoking presents for progressive pedal edema, pleural effusion, ascites, and shortness of breath for 9 months. He previously had an acute MI and underwent percutaneous coronary intervention with three drug eluting stents at the right coronary artery 15 months ago.
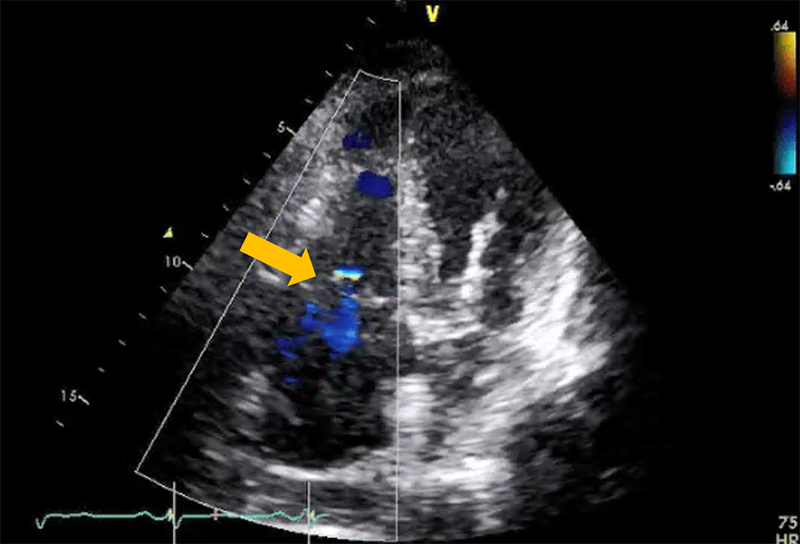
At the office, his blood pressure was 166/79 mmHg, his pulse was 79 beats per minute, and his oxygen saturation was 99% on room air. On exam, he had jugular venous distension to the angle of jaw, clear lungs, and regular S1 and S2 with no murmurs or pericardial knock. He had ascites and 2+ bilateral lower extremity edema. Chest X-ray (CXR) showed normal heart size but increase of pulmonary vasculature suggestive of elevated pulmonary venous pressure. No pericardial calcification visualized. Electrocardiogram showed sinus rhythm, generalized low voltage, borderline left axis deviation, no ST-T change. Echocardiography showed normal LV size and function (EF = 57%), septal bounce with diastolic flattening of posterior wall, 1+ mitral regurgitation and 1+ tricuspid regurgitation (TR) (Figure 1), moderate right ventricular (RV) and right atrial (RA) dilatation, tethering of RV and RA free wall. Tricuspid valve annulus (TVA) was 31 mm. Saline agitation showed no intracardiac shunt. Inferior vena cava (IVC) was markedly dilated with blunted respiratory response; estimated right ventricular systolic pressure (RVSP) was 28 mmHg. Mitral inflow Doppler showed E/A ratio was 1.56. Mitral medial e' was 12 cm/sec and lateral e' was 7 cm/sec consistent with annulus reversus. RV function was impaired (tricuspid annular peak systolic velocity (RV S') was 6 cm/sec, tricuspid annular systolic excursion (TAPSE) was 12 mm, right ventricular fractional area change (FAC) was 34%. Mitral inflow variation was 12%. Tricuspid inflow variation was 20%. Hepatic vein expiratory end-diastolic reversal velocity/forward flow velocity ratio was 0.77.
Figure 1
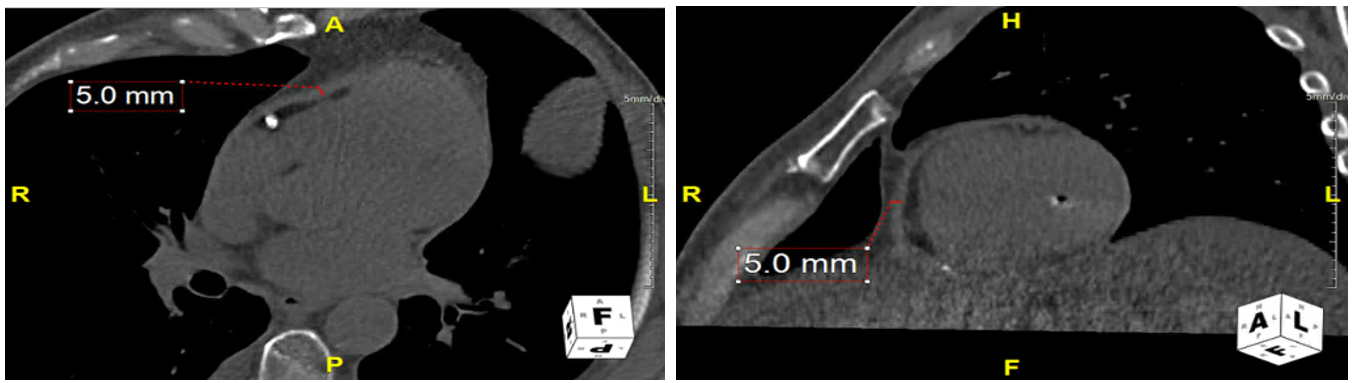
Cardiac (computed tomography) CT showed no pericardial calcification, no pericardial effusion. The thickest part of pericardium was 5 mm anterior to RV (Figure 2).
Figure 2
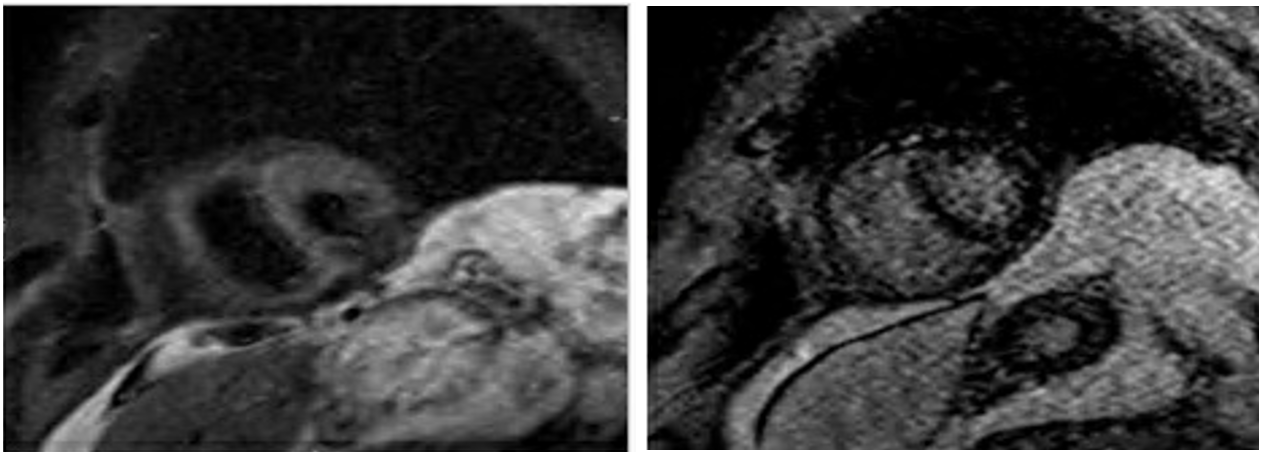
Cardiac magnetic resonance (CMR) imaging showed normal signal intensity on T2 STIR imaging, no definitive delayed enhancement of myocardium (Figure 3). Right heart catheterization showed equalization of left ventricle (LV) and RV diastolic pressures and respiratory discordance of systolic pressures consistent with pericardial constriction.
Figure 3
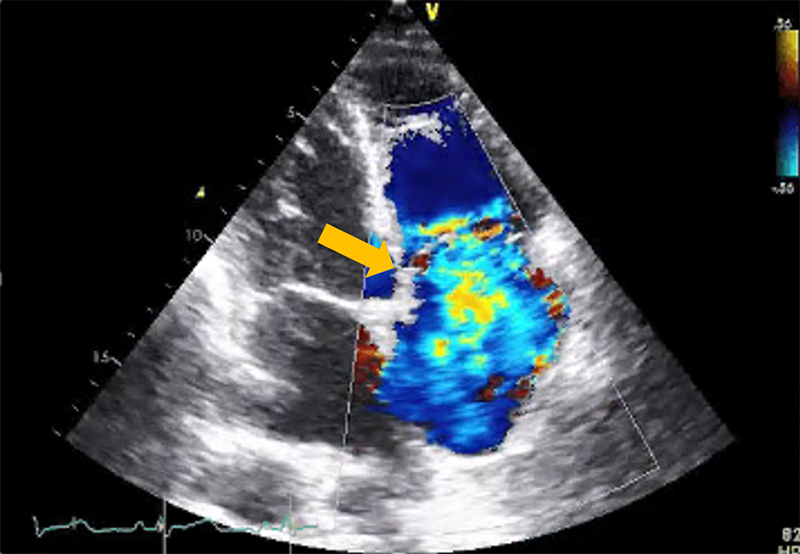
He underwent radical pericardiectomy. Pathological study of pericardium revealed mild chronic pericarditis and marked fibrosis. CXR post-operative showed increase heart size. Bilateral pleural effusion. Two weeks after discharge, his body weight increased by 3 pounds with 1+ bilateral legs edema. He had no shortness of breath. Echocardiography showed LVEF = 60%, no septal bouncing. MR was increased from 1+ to 2+. Diastolic LV D-shaped consistent with RV volume overload. RV is larger than pre op echo. TVA was increased from 31 to 35 mm. Poor coaptation of TV with 4+TR (Figure 4). Estimated RVSP was 36 mmHg. RV S' was reduced from 6 to 5 cm/sec. TAPSE was reduced from 12 to 4 cm/sec. RV FAC was increased from 34 to 46%. Hepatic vein Doppler showed systolic flow reversal consistent with severe TR.
Figure 4
Which of the following pre-operative echo parameters best predicts worsened post-operative tricuspid regurgitation?
Show Answer