A 79-year-old female with past medical history significant for post-polio syndrome complicated by diaphragmatic weakness, restrictive lung disease, recurrent pneumonia complicated by respiratory failure, chronic mycobacterial pulmonary abscesses, bronchiectasis, moderate pulmonary hypertension, and obstructive sleep apnea presented to the emergency room (ER) with sudden onset chest pain that woke her up from sleep. She describes the pain as spreading from shoulder to shoulder and creeping up her jaw. It was dull, 6/10 in severity, and was not worse with breathing nor associated with diaphoresis. She described epigastric pressure, palpitations and shortness of breath (SOB) with eating that would last a few hours after eating. As the pain woke her up from sleep and was new for her, she called Emergency Medical Services (EMS) and was transported to the ER. She received aspirin and nitroglycerin by EMS, with no relief of symptoms.
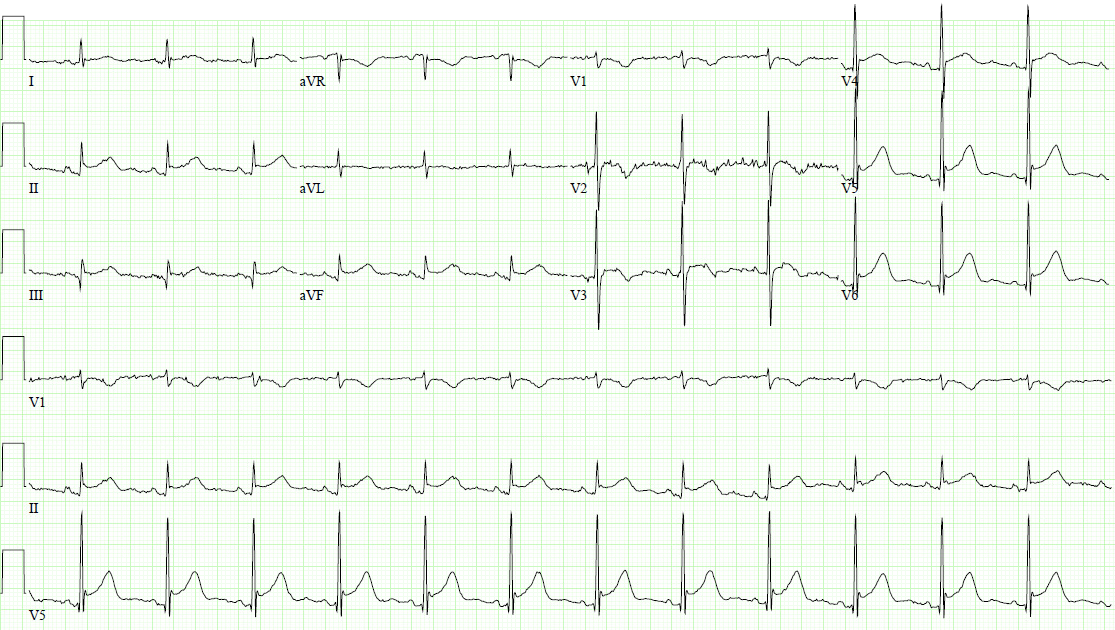
In the ER, she was afebrile and hemodynamically stable. Her initial electrocardiogram (ECG) showed ST-segment elevation in leads II, III, aVF, V3-V6, and T-wave inversions in aVR and V1 (Figure 1). Her labs showed a high-sensitivity troponin of 29 ng/L (reference range <12 ng/L). Contrast-enhanced CT chest, pulmonary embolism protocol, was negative for pulmonary embolism, aortic dissection, and pericardial effusion.
Figure 1
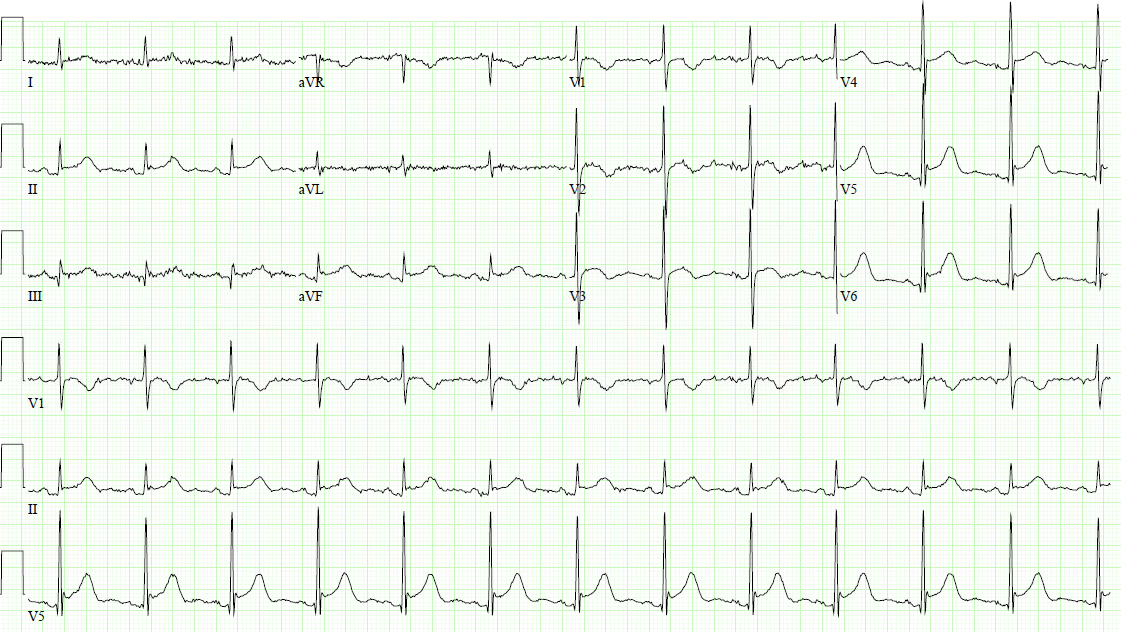
While in the ER, the patient had another episode of chest pain that was associated with ST-segment elevation in leads II, III, aVF, V4-V6 and T-wave inversions in V1-V3 (Figure 2).
Figure 2
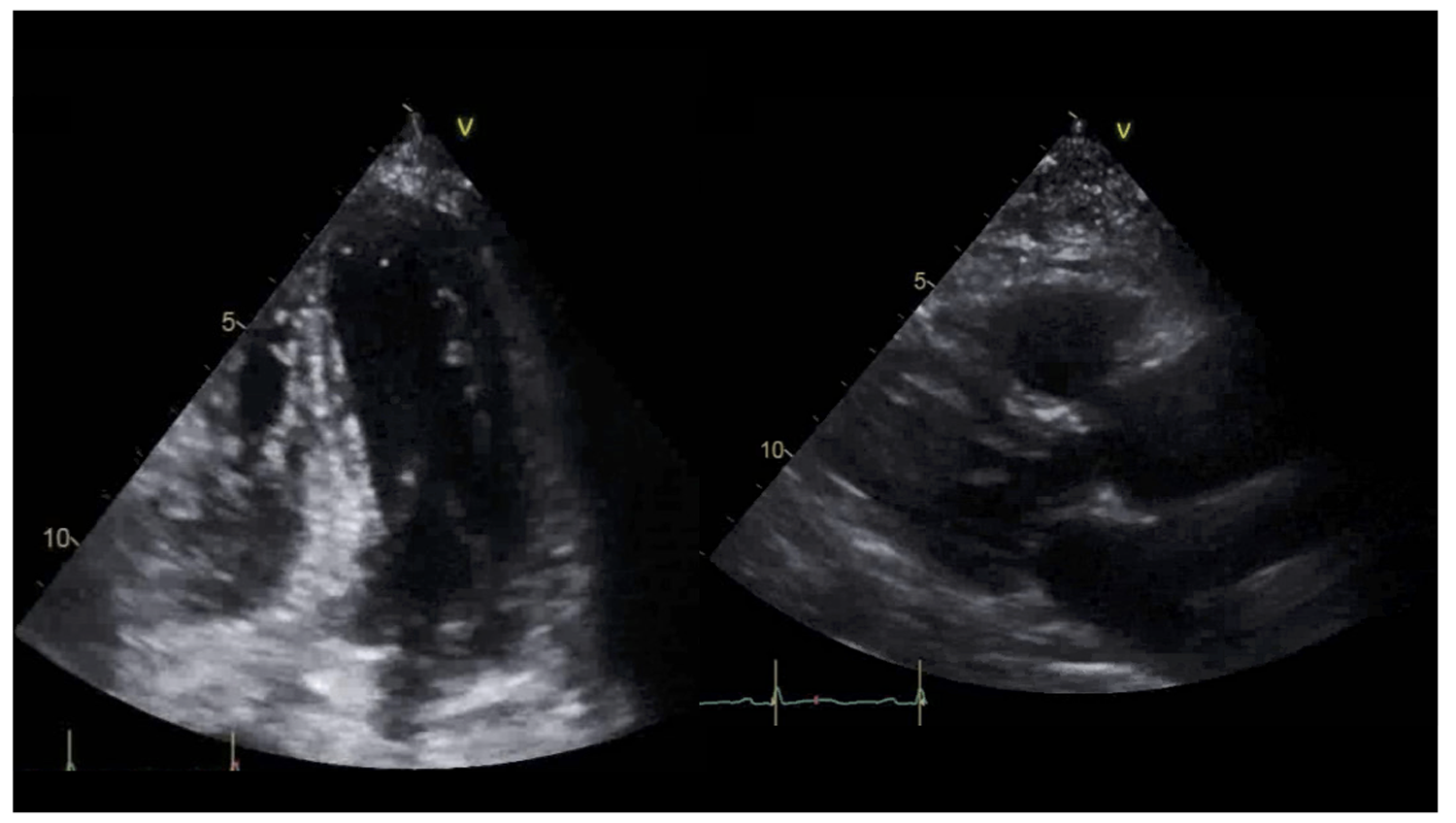
The pain resolved with the use of sublingual nitroglycerin. Repeat high-sensitivity troponin came back as 23 ng/L, ESR was 28 mm/hr (reference range 0-20 mm/hr), and CRP was 6.8 mg/dL (reference range < 0.9 mg/dL). Bedside echocardiography showed a hyperdynamic systolic function with an ejection fraction (EF) of 75%, upper septal left ventricular hypertrophy, Grade I left ventricular diastolic dysfunction, RVSP of 59 mmHg, and a small pericardial effusion measuring 0.4 cm (Figure 3). The patient was started on aspirin 650 mg 3 times a day, and colchicine 0.6 mg daily for management of acute pericarditis. The patient was discharged with an aspirin taper over 2 months and colchicine 0.6 mg daily.
Figure 3
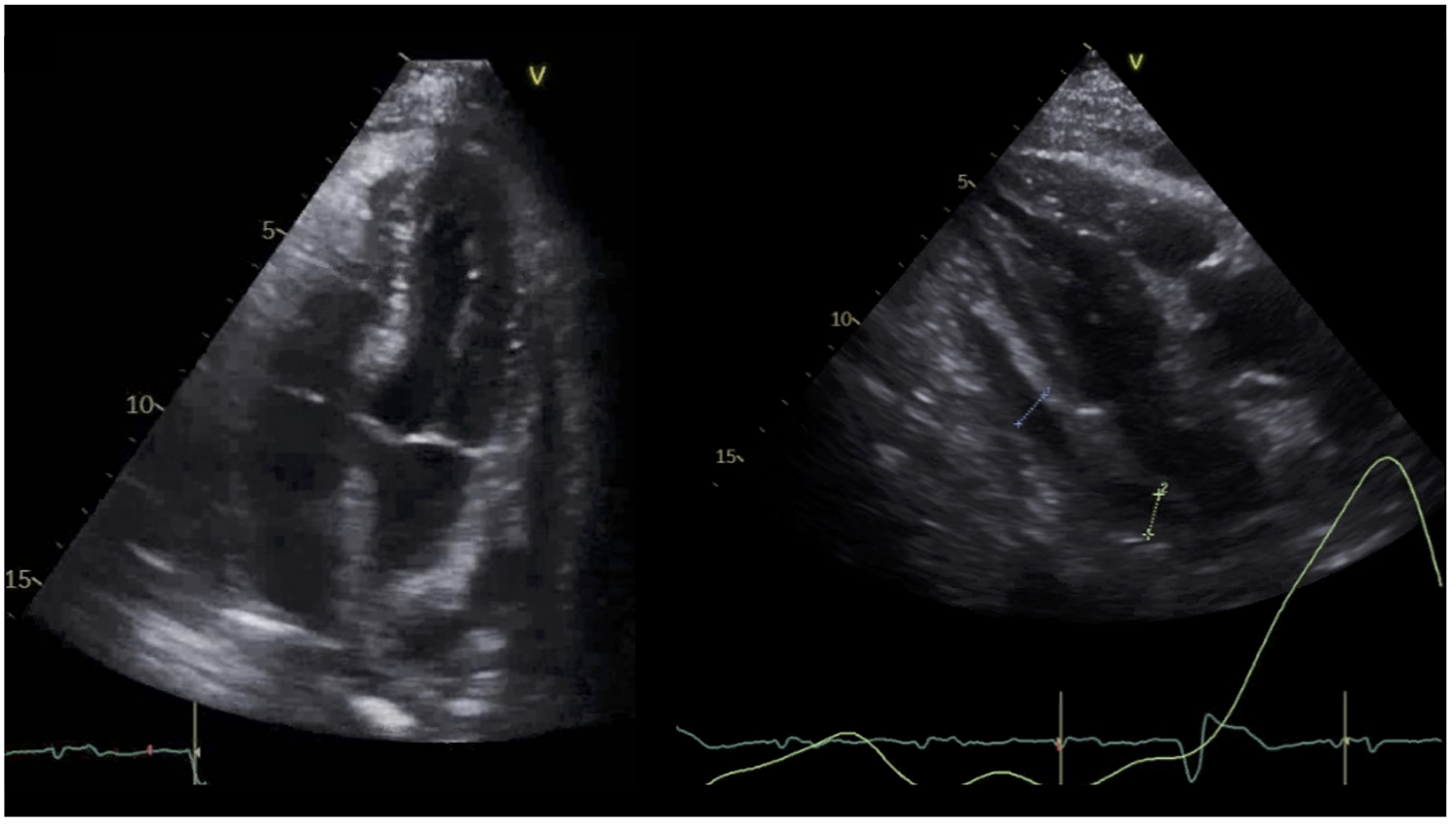
Three weeks later, the patient had recurrence of her chest pain associated with SOB. Her exam was mostly unchanged with cardiac exam showing normal S1 and S2, no murmurs, no pericardial rub or knock, no jugular venous distention, no Kussmaul's sign, and no peripheral edema. Her inflammatory markers were elevated compared to time of diagnosis; ESR was 56 mm/hr, and CRP was 8.3 mg/dL. Echocardiography was performed and showed EF of 71% with a significant interval increase in the size of the pericardial effusion now measuring 1.9 cm with some organization and a brief right atrial inversion. No significant mitral respiratory variation or definite tamponade physiology were noted (Figure 4).
Figure 4
The correct answer is: D. High dose of NSAIDs and colchicine BID should be used if chest pain recurs during initial tapering.
Nonsteroidal anti-inflammatory drugs (NSAIDs) in higher doses, i.e., ibuprofen (400–600 mg 3 times a day) or indomethacin (25–50 mg 3 times a day), with colchicine (0.6 mg twice a day) are indicated in patients who could not tolerate the initial taper of anti-inflammatory agents i.e., aspirin (650 mg 3 times a day), and daily colchicine. Colchicine is useful in both acute flares and preventing recurrences of pericarditis.1 Aspirin should be prioritized over other NSAIDs in patients who have an indication for antiplatelet therapy such as secondary prevention or following coronary artery stent placement. Colchicine should also be the last treatment to taper in that patient population. Tolerance to colchicine should be assessed at each follow up visit; it should be avoided in patients with hepatic or renal dysfunction.2,3
- Acute pericarditis presents with chest pain, ST-segment elevations, and possible elevations in cardiac biomarkers. Acute pericarditis related chest pain is usually sharp, aggravated by inspiration and coughing, and relived by leaning forward. However, in some cases the chest pain is atypical and presents as constricting or pressure-like pain that radiates to the left arm which may be confused for angina. Imaging-associated stress testing maybe beneficial in determining co-existence of coronary artery disease, however, they are not indicated routinely in patients with pericarditis and tachycardia related to exercise or stress and may aggravate pericardial inflammation; thus, worsening chest pain.
- Pericardiocentesis is indicated in patients who have pericardial effusion resulting in cardiac tamponade. Echocardiographic signs of tamponade include: 1. diastolic collapse of the right atrium (RA) and the right ventricle (RV), 2. dilatation of the inferior vena cava (IVC) with <50% reduction in diameter during respiration, 3. respirophasic septal shift, 4. exaggerated respirophasic variation in the mitral and tricuspid inflow velocities (>60% increase in TV inflow and >30% decrease in MV inflow during inspiration). Echocardiographic-guided pericardiocentesis is indicated urgently in patients with signs of pericardial tamponade regardless of effusion size. However, if pericardial effusions presented with no clinical or imaging signs of tamponade, pericardiocentesis is not indicated at that time.4
- Pericardiectomy is used after exhausting all lines of medical treatment including steroids and biologics, i.e., anakinra, rilonacept as a last resort treatment in patients with intractable disease. Pericardiectomy is associated with reduced recurrence of pericarditis; however, it should be performed by experienced surgeons at high-volume centers to minimize the risk of complications. Attempting to reduce active inflammation with maximal medical therapy should be attempted before surgery.5,6
- See above.
- Glucocorticoids are effective in suppressive inflammation in acute pericarditis; however, they are associated with a higher side effect profile as well as an increased risk of pericarditis recurrence with rapid taper. Low dose corticosteroids (0.25-0.5 mg/kg/day) should be given with a slow taper (taper by 10-20% of dose every 1-2 weeks i.e. if on 25 mg of prednisone then taper by 2.5 mg every 2 weeks, and only if the patient is asymptomatic and inflammatory markers are within normal range) as second line treatment in recurrent pericarditis in patients who fail or are unable to tolerate colchicine and NSAIDs; if second line treatment fails then third line agents such as IVIG, azathioprine, and IL-1 inhibitors should be considered. Interleukin-1 (IL-1) inhibitors such as anakinra, rilonacept, and canakinumab are emerging as effective treatment for pericarditis. At this time, IL-1 inhibitors are US Food and Drug Administration (FDA) approved for rheumatoid arthritis but not pericarditis and are being used off-label. Recent clinical trials suggest that using anakinra help reduce recurrences in patients with recurrent pericarditis on colchicine and corticosteroids.7 Recent work with rilonacept, an IL-1 alpha/beta receptor from the RHAPSODY trial, showed promising outcomes in patients with recurrent pericarditis with a faster time to resolution of symptoms as well as lower risk of recurrences.8
References
- Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2015;36:2921-64.
- Bayes-Genis A, Adler Y, de Luna AB, Imazio M. Colchicine in pericarditis. Eur Heart J 2017;38:1706-09.
- Imazio M, Gaita F, LeWinter M. Evaluation and treatment of pericarditis: a systematic review. JAMA 2015;314:1498-506.
- McIntyre WF, Jassal DS, Morris AL. Pericardial effusions: do they all require pericardiocentesis? Can J Cardiol 2015;31:812-5.
- Cremer PC, Kumar A, Kontzias A, et al. Complicated pericarditis: understanding risk factors and pathophysiology to inform imaging and treatment. J Am Coll Cardiol 2016;68:2311-28.
- Depboylu BC, Mootoosamy P, Vistarini N, Testuz A, El-Hamamsy I, Cikirikcioglu M. Surgical treatment of constrictive pericarditis. Tex Heart Inst J 2017;44:101-06.
- Brucato A, Imazio M, Gattorno M, et al. Effect of anakinra on recurrent pericarditis among patients with colchicine resistance and corticosteroid dependence: The AIRTRIP Randomized Clinical Trial. JAMA 2016;316:1906-12.
- Klein AL, Imazio M, Cremer P, et al. Phase 3 trial of Interleukin-1 trap rilonacept in recurrent pericarditis. N Engl J Med 2021;384:31-41.