A Collegiate Football Player With Left Ventricular Hypertrophy and an Intracavitary Gradient: Athletic Heart or Hypertrophic Cardiomyopathy?
An 18-year-old white male recruited to play Division I collegiate football as a defensive tackle was flagged during pre-participation screening due to anterior T-wave inversions on electrocardiogram (ECG) and a family history of premature coronary artery disease. He has played competitive sports (hockey, football, and basketball) for most of his life. He has never experienced exertional chest pain or pressure, dyspnea, syncope, lightheadedness, or palpitations. He works out five times per week with a focus on power lifting and feels faster and stronger than others his size (6'5", 286 lbs.). There is no family history of sudden or unexplained death or hypertrophic cardiomyopathy. His maternal grandfather, a smoker and heavy drinker, suffered a myocardial infarction and died at the age of 49. Physical examination is normal.
The team physician recommended an exercise stress echocardiogram as the initial step to evaluate the abnormal ECG. Resting images revealed an ejection fraction (EF) of 65%, left ventricular (LV) hypertrophy with septal and posterior wall thickness of 13mm and 12mm, respectively, end diastolic LV internal diameter of 58mm, a normally tapering non-hypertrophied LV apex, normal diastolic function and minimal resting systolic anterior motion (SAM) of the subvalvular mitral valve (MV) apparatus (Video 1, 2). He exercised to 12.8 METS and 89% maximum predicted heart rate without symptoms and had a normal blood pressure response. He had appropriate LV augmentation but a peak left ventricular outflow track gradient (LVOT) of 57mmHg was noted. The study conclusion indicated the presence of hypertrophic cardiomyopathy (HCM) with dynamic obstruction and he was deemed ineligible for competitive football by the team's local cardiologist.
Video 1
Video 2
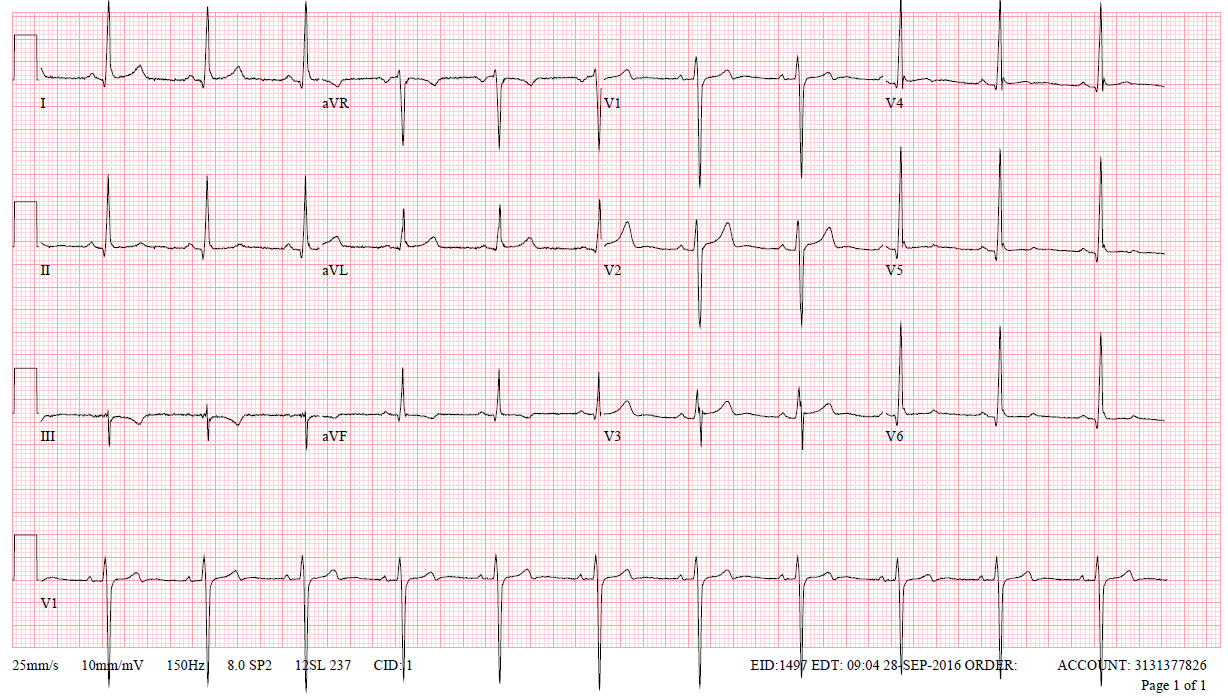
He was referred for a second opinion. A follow up ECG is shown in Figure 1. Cardiac MRI was performed revealing an EF of 60% with normal chamber size, maximal wall thickness of 12 at the mid-septum and no evidence of fibrosis or scarring (Figure 2). There were no premature ventricular contractions or alternative arrhythmias on a 24-hour Holter monitor. After review of the data, it was thought that findings were not suggestive of HCM but rather "athletic heart" and that he did not require sport disqualification.
Figure 1: Electrocardiogram
Figure 2: Cardiac MRI: Delayed Imaging

Due to conflicting opinions, he was next referred to a renowned academic HCM program where his evaluation started with a bicycle stress echocardiogram. He exercised for 12 minutes 43 seconds, 9 METS and 96% maximum predicated heart rate without symptoms or hemodynamic abnormalities. Exercise revealed severe SAM of the MV and chords, an LVOT gradient of 92mmHg at peak stress, but no increase in mitral regurgitation. Genetic testing was unrevealing. It was recommended that he de-train and be reassessed in six months.
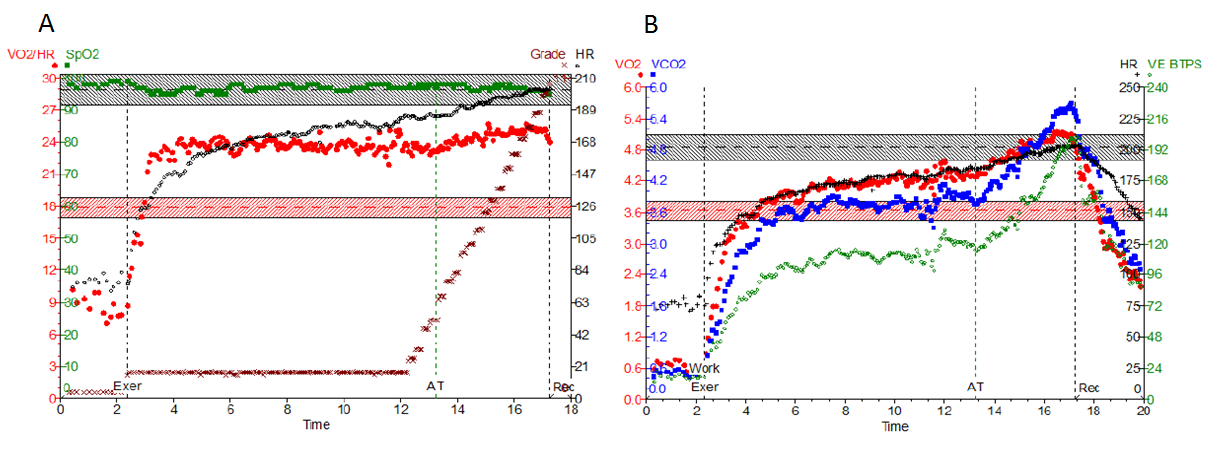
The athlete and his parents were not satisfied with the explanations and conclusions that were drawn up to this point and wanted to be more engaged in the decision-making. They sought out a local cardiologist with an interest in sports cardiology and he recommended a cardiopulmonary exercise test (CPET) in hopes that it would provide more clarity to the diagnosis. The test was stopped early (11 minutes 13 seconds, RER 0.96) due to a failure of the O2 pulse to augment. The athlete did not report any symptoms and did not have any hemodynamic abnormalities. The CPET report documented a peak exercise capacity of 5.6 METS and peak VO2 of 45 % age and gender predicted with findings suggestive of an exercise induced fall in cardiac output. With multiple different opinions and test results, the patient and family are referred to an academic center with a sports cardiology program.
Which of the following is the best recommendation for this patient?
Show Answer