Note: Drs. Singh and Tsutsui share co-first authorship.
A 52- year-old woman with history of paroxysmal atrial fibrillation and recurrent pericarditis with recurrent pericardial effusion presented with sharp chronic chest pain affecting her daily activities. Her ESR was 40 mm/hr and CRP was 33.3 mg/dl. Other investigative workup was negative for infection, autoimmune disorders, and malignancy. She had undergone one pericardiocentesis and two pericardial windows over the past 2 years for her recurrent pericardial effusions. She had been treated with ibuprofen, colchicine, azathioprine, methotrexate, and chronic corticosteroids. She was on 20mg of prednisone daily with failure to taper. She had significant side effects from steroids including cushingoid features, cataract, and severe osteoporosis.
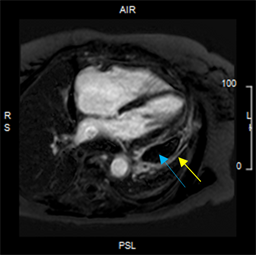
Her initial cardiac magnetic resonance imaging (MRI) showed moderate localized pericardial effusion along anterolateral, inferolateral left ventricular wall, left atrial and right atrial free wall, but no pericardial thickening or evidence of constrictive physiology. There was trivial delayed enhancement of lateral parietal pericardium (Figure 1). Due to her recurrent symptoms and side effects of the anti-inflammatory therapy, she then underwent a radical pericardiectomy. The pericardium was incised systematically from the left, right, and posterior leaving behind a thin strip along the phrenic nerves bilaterally. Post-pericardiectomy, her symptoms improved and cardiac MRI at 3 months showed interval improvement with only mild residual enhancement of remaining fibrinous material/visceral pericardium on T2STIR as well as post gadolinium delayed enhancement imaging suggestive of mild inflammation. She was continued on aspirin and colchicine, and steroids were slowly tapered off.
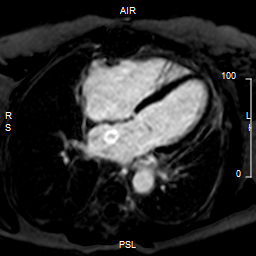
Over the next 2 years she had only two episodes of pericarditis flare, while being off steroids. Follow up cardiac MRI at 2 years showed complete interval resolution of the mild residual enhancement that was noted on previous study. There was no abnormal peri/epicardial signal intensity on STIR imaging to suggest pericardial edema (Figure 2). She remained symptom free and was taking only aspirin 650 mg twice daily.
Figure 1: Pre-pericardiectomy. Delayed enhancement image demonstrating a loculated lateral pericardial effusion (blue arrow) with mild pericardial delayed enhancement (yellow arrow).
Figure 2: Post-pericardiectomy. Delayed enhancement image demonstrating pericardial stripping and resolution of the pericardial effusion and inflammation.
The correct answer is: C. Offers complete cure.
European guidelines have classified pericarditis into three categories: incessant, recurrent, and chronic.1 Pericarditis that persists for more than 4 to 6 weeks but less than 3 months is termed incessant, and pericarditis lasting for more than 3 months is considered chronic. If a patient is free of symptoms for at least 4 to 6 weeks before a relapse, it is termed as recurrent pericarditis.1,2 Recurrent or relapsing pericarditis affects one-third of patients with pericarditis.3,4 Cremer et al. has emphasized on the role of inflammasome activation in recurrent pericarditis and potential role of cardiac magnetic resonance imaging in early recognition of progression of pericarditis.5
Non-steroidal anti-inflammatory drugs (NSAIDS) and colchicine are the first-line treatment for initial episodes of relapsing pericarditis.5-7 Corticosteroids are used in the cases who fail first-line therapy and their use has been associated with more relapses.5-7 Immunosuppressive drugs are used in patients with autoimmune diseases.5,6 Surgical pericardiectomy has been proposed for relapsing pericarditis in patients who are resistant to steroids or have severe side effects from medical therapy (Answer A).8
Khandaker et al.8 in their retrospective review of 184 patients (1994-2005) showed no significant difference in the mortality between the patients undergoing pericardiectomy versus medical therapy. Survival curves showed no difference in all-cause death at follow up for 16 years (P = 0.26) (Answer B). Pericardiectomy for relapsing pericarditis does not guarantee a complete cure as there can be subsequent relapses. 8.6 percent of post-pericardiectomy patients suffered from relapse in the review (Answer C).8 However, pericardiectomy reduces the number of relapses when compared to medical therapy. Kaplan-Meier curves for relapse showed early separation in the follow up period, with post-pericardiectomy patients having significantly fewer relapses (P = 0.009) (Answer D).8 The use of medications including NSAIDs, colchicine, and prednisone was also reduced after the surgery.8 Hence, pericardiectomy can be considered safe and effective when performed by a well experienced surgeon (Answer E).8 It provides longer symptom free periods and hence improved quality of life.9
Recent analysis by Gillaspie et al.10 showed that pericardiectomy performed for relapsing pericarditis had significantly higher survival than for chronic constrictive pericarditis (Answer F). The type of surgical approach (median sternotomy, left thoracotomy, or clamshell) did not affect the overall survival.
References
- Adler Y, Charron P, Imazio M, et al. 2015 ESC guidelines for the diagnosis and management of pericardial diseases: the task force for the diagnosis and management of pericardial diseases of the European Society of Cardiology (ESC) endorsed by: the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2015;36:2921-64.
- Imazio M, Adler Y, Charron P. Recurrent pericarditis: modern approach in 2016. Curr Cardiol Rep 2016;18:50.
- Imazio M, Bobbio M, Cecchi E, et al. Colchicine as first-choice therapy for recurrent pericarditis: results of the CORE (COlchicine for REcurrent pericarditis) trial. Arch Intern Med 2005;165:1987-91.
- Imazio M, Brucato A, Cemin R, et al. Colchicine for recurrent pericarditis (CORP): a randomized trial. Ann Intern Med 2011;155:409-14.
- Cremer PC, Kumar A, Kontzias A, et al. Complicated pericarditis: understanding risk factors and pathophysiology to inform imaging and treatment. J Am Coll Cardiol 2016;68:2311-28.
- Imazio M, Adler Y. Treatment with aspirin, NSAID, corticosteroids, and colchicine in acute and recurrent pericarditis. Heart Fail Rev 2013;18:355-60.
- Artom G, Koren-Morag N, Spodick DH, et al. Pretreatment with corticosteroids attenuates the efficacy of colchicine in preventing recurrent pericarditis: a multi-centre all-case analysis. Eur Heart J 2005;26:723-7.
- Khandaker MH, Schaff HV, Greason KL, et al. Pericardiectomy vs medical management in patients with relapsing pericarditis. Mayo Clin Proc 2012;87:1062-70.
- Hatcher CR Jr, Logue RB, Logan WD Jr, Symbas PN, Mansour KA, Abbott OA. Pericardiectomy for recurrent pericarditis. J Thorac Cardiovasc Surg 1971;62:371-8.
- Gillaspie EA, Stulak JM, Daly RC, et al. A 20-year experience with isolated pericardiectomy: analysis of indications and outcomes. J Thorac Cardiovas Surg 2016;152:448-58.