Editor's Corner | Stroke Prevention Beyond Atrial Fibrillation
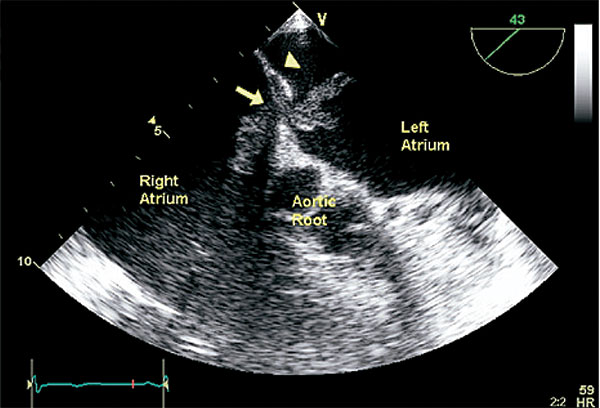 Transesophageal echocardiographic view of the short axis of the heart, showing an oblong echodensity with two distal extensions trapped in the foramen ovale (arrow), consistent with thrombus in transit. The arrowhead points to the septum primum. Reproduced with permission from J Am Coll Cardiol 2008;51:1049-59.
Transesophageal echocardiographic view of the short axis of the heart, showing an oblong echodensity with two distal extensions trapped in the foramen ovale (arrow), consistent with thrombus in transit. The arrowhead points to the septum primum. Reproduced with permission from J Am Coll Cardiol 2008;51:1049-59.
Over the past several years, we have witnessed a wide spectrum of clinical trials devoted to improving the care of patients with atrial fibrillation (AFib) and reducing their risk of stroke. We adopted the direct-acting oral anticoagulants, maintained sinus rhythm with left atrial ablation and used left atrial appendage occluders in patients who could not be treated with our usual tools for lowering stroke incidence in AFib.
In late 2017, several important clinical trials and meta-analyses described another cause of strokes associated with arterial embolic disease not related to AFib. These “cryptogenic strokes” are often found in younger patients, who after extensive workups show no cause for the stroke. Two important randomized clinical trials — CLOSE and REDUCE — demonstrated a significant relationship between cryptogenic stroke and patent foramen ovale (PFO).
Around the same time, two meta-analyses involving over 3,000 patients with cryptogenic stroke demonstrated a significant relationship between strokes and PFO in the studied populations. This relationship is not new. In the world of undersea medicine, the role of a PFO has been questioned for over a decade. Observational studies and meta-analyses have shown a significant relationship between cerebral gas embolism and PFO. A recent randomized controlled trial showed a clear relationship between PFO and arterial gas embolism related to inadequate decompression from increased environmental pressure.
The PFO is a residual communication between the right and left atrium resulting from incomplete fusion of the atrial wall with the fossa ovalis. It’s present in 25 to 30 percent of the population. In some cases of cyanotic congenital heart disease with significant right-to-left shunting, the foramen ovale persists because of the high right atrial pressures related with the congenital heart defect. In cases of severe pulmonic stenosis or pulmonary hypertension with elevated right-sided pressure, a PFO can also produce a significant right-to-left shunt. In the platypnea-orthodeoxia syndrome, a PFO is the cause of intermittent cyanosis related to postural changes.
With these recently published clinical trials confirming a relation between PFO and stroke, the first reaction would be to close the PFO in all patients — nearly a third of the population. But there seems to be something missing in this relationship. The incidence of stroke in the population below 60 years old who have no other stroke risks is clearly not 30 percent. Indeed, the incidence of stroke in an otherwise healthy population younger than 60 is extremely small, nowhere near 30 percent of the population. This observation quickly leads to the conclusion there are other important factors involved in a cause-effect relation between PFO and stroke.
"With these recently published clinical trials confirming a relation between PFO and stroke, the first reaction would be to close the PFO in all patients – nearly a third of the population. But there seems to be something missing in this relationship."
Bubble-contrast studies usually relate a large PFO with more than 25 left atrial bubbles visible within three heart cycles after injection of bubble contrast into a peripheral vein. These are readily seen on echocardiogram. Often the left atrium is filled with bubbles that crossed a PFO from the right atrium. Direct measurement of the PFO diameter usually equates a large PFO with a diameter greater than 7 mm. A large atrial aneurysm is also thought to increase risk for a stroke. This would leave about 10 percent of the population with a large PFO and at increased risk for a stroke. Even with a 10 percent incidence of large PFOs in the population, there are clearly other factors that contribute to stroke in these patients as the overall stroke incidence remains very low even in patients with a large PFO.
The question of which PFO should be closed is presently unanswered and unclear. Characteristics of the PFO and the patient need to be considered. In the decompression studies, only large PFOs with large right-to-left shunts were related to evidence of cerebral air embolism. In the CLOSE and REDUCE randomized trials of cryptogenic stroke, patients with small vessel occlusive disease, hypercoagulable states, atherosclerotic disease of proximal arteries and arterial dissection were excluded from the trials.
How should we manage a younger patient who has a stroke? Before blaming a PFO, be sure the patient has no other risks for a stroke, including paroxysmal AFib. Assess the size of the PFO using echo bubble contrast injected into a peripheral vein. Remember that about 30 percent of the population has a PFO, so presence alone should not be a criterion for closure. Identifying the high-risk patient should be the first goal of assessment of younger patients with a previous stroke.
Closing a low-risk PFO is not likely to improve the patient outcome and will put the patient at unnecessary risk of complications. While stroke risk is reduced after PFO closure, it is not eliminated. A discussion with the patient about risks and expectations should be part of the care for these patients.
Alfred A. Bove, MD, PhD, MACC, is professor emeritus of medicine at Temple University School of Medicine in Philadelphia, and a former president of the ACC.
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Valvular Heart Disease, Anticoagulation Management and Atrial Fibrillation, Atrial Fibrillation/Supraventricular Arrhythmias, Congenital Heart Disease, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Imaging, CHD and Pediatrics and Prevention, Pulmonary Hypertension, Echocardiography/Ultrasound, Hypertension
Keywords: ACC Publications, Cardiology Magazine, Foramen Ovale, Patent, Atrial Fibrillation, Atrial Appendage, Embolism, Air, Foramen Ovale, Sagittaria, Atrial Pressure, Goals, Echocardiography, Transesophageal, Stroke, Intracranial Embolism, Embolism, Thrombosis, Pulmonary Valve Stenosis, Anticoagulants, Hypertension, Pulmonary, Cyanosis, Arteries, Aneurysm
< Back to Listings


