Feature | Hypertriglyceridemia: Insights on Needs of Cardiologists, CV Team to Reduce Residual Risk
In the lipid arena, lowering LDL-C continues to be a major focus for reducing the risk of cardiovascular events. Cardiovascular outcomes trials have shown benefit with ever-lower LDL-C levels and even a growing armamentarium of drugs. Yet there’s residual risk that continues to contribute to a risk of cardiovascular events that is too high, including in patients whose triglyceride levels remain elevated despite optimized statin therapy.
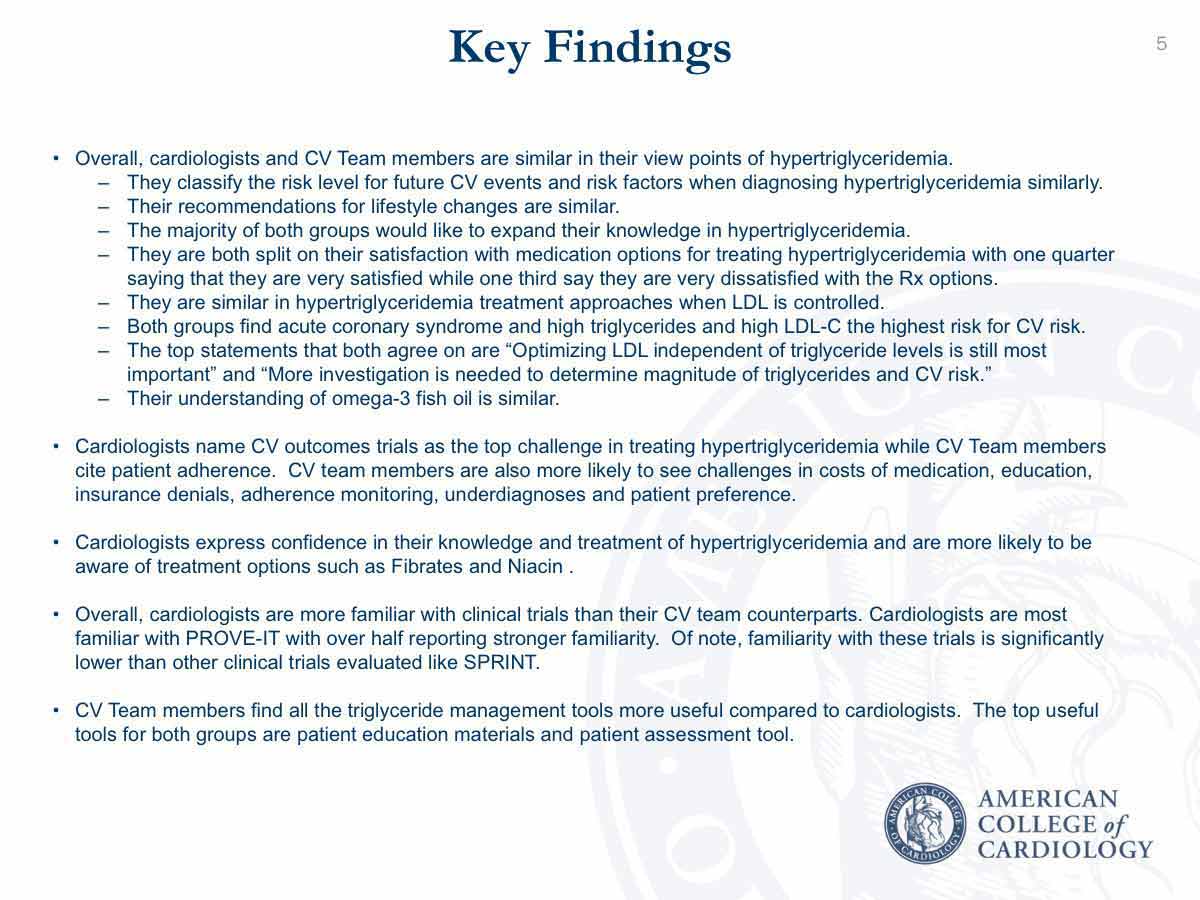
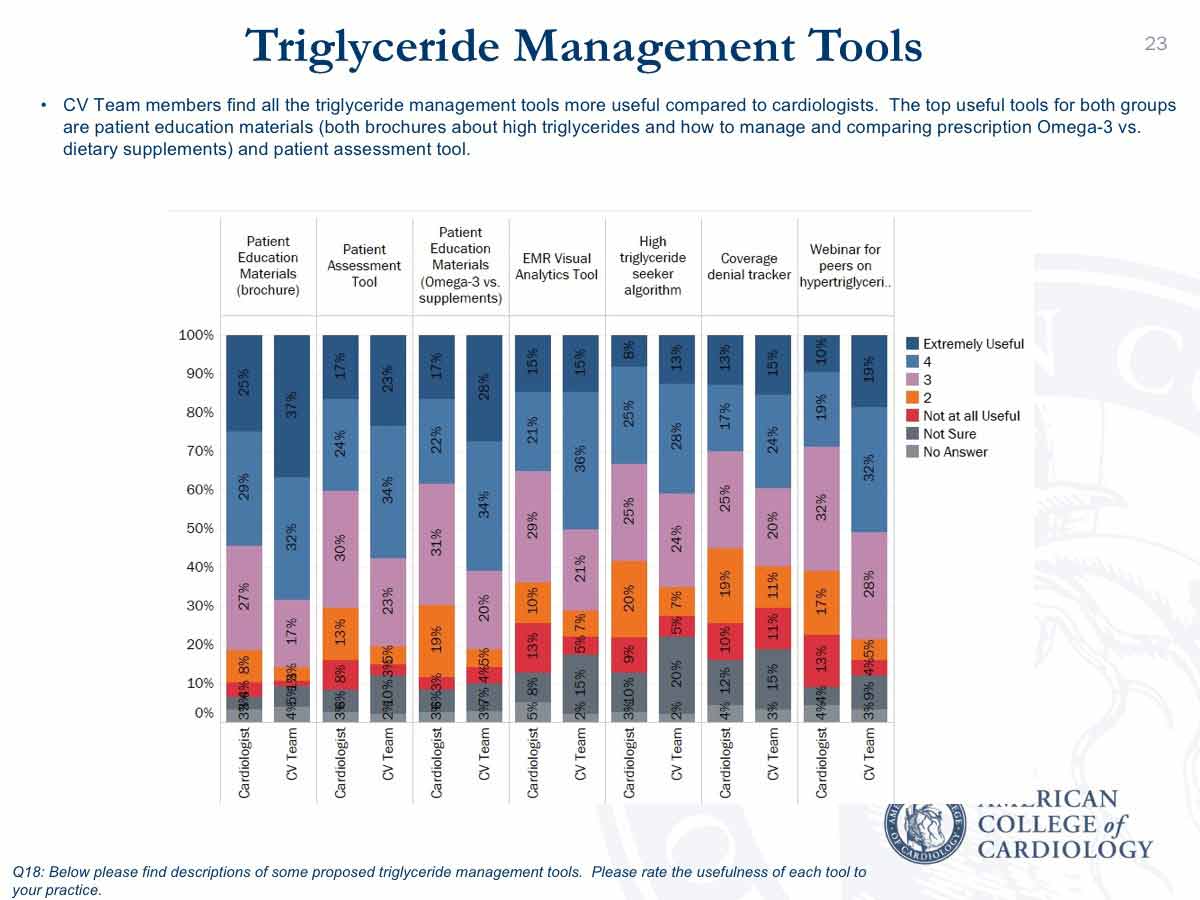
What is needed to bring triglycerides down to the levels required to reduce this residual risk? According to a recent ACC survey of cardiologists and cardiovascular team (CV Team) members who treat patients with dyslipidemia or hypertriglyceridemia, education and evidence from cardiovascular outcomes trials of effective agents that reduce events are among the top needs and challenges.
The challenge that clinicians face because of the lack of data from randomized clinical trials is perhaps not an unexpected finding. “Currently, we have equipoise,” says Michael Shapiro, MD, FACC, chair of the Dyslipidemia Work Group of ACC’s Prevention Council.
The association between triglycerides and cardiovascular disease, particularly atherosclerotic cardiovascular disease (ASCVD), is a consistent finding across epidemiologic data. Similar with how the epidemiologic data are consistent for the association between LDL-C and ASCVD and the inverse relation between HDL-C and ASCVD. “The randomized trial evidence for LDL-C is coherent and consistent,” says Shapiro, and there is now evidence in support of a number of LDL-C lowering drugs (statins, ezetimibe, PCSK9 inhibitors) that improve cardiovascular outcomes.” But, this did not hold true for randomized data for HDL-C. “Hence, the medical community is waiting for results from the ongoing clinical trials to help us better guide treatment,” says Shapiro.
Three randomized clinical trials are underway that have the potential to provide this evidence. The STRENGTH trial is investigating epanova, an omega-3-carboxylic acid, in high-risk patients being treated with a statin and is expected to be completed in late 2019. The PROMINENT trial is examining pemafibrate in patients with type 2 diabetes being treated with a statin and is expected to be completed in 2022.
"The randomized trial evidence for LDL-C is coherent and consistent and there is now evidence in support of a number of LDL-C lowering drugs that improve cardiovascular outcomes. But, this did not hold true for randomized data for HDL-C. Hence, the medical community is waiting for results from the ongoing clinical trials to help us better guide treatment." — Michael Shapiro, MD, FACC
The third trial, REDUCE-IT, is likely to be reported later this year, perhaps in the third quarter. REDUCE-IT is studying whether icosapent ethyl, a highly purified ethyl ester of eicosapentaenoic acid, will improve cardiovascular outcomes in statin-treated patients. “If the results are positive, REDUCE-IT will be a practice changing trial,” says Seth S. Martin, MD, MHS, FACC.
This international trial has enrolled about 8,000 patients ≥45 years with established cardiovascular disease or age ≥50 years with diabetes and one additional risk factor. Participants have fasting triglycerides of 150 to <500 mg/dL and LDL-C >40 to ≤100 mg/dL with stable statin (± ezetimibe) therapy. The primary outcome is a composite of cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, coronary revascularization or unstable angina.
Who Was Surveyed?
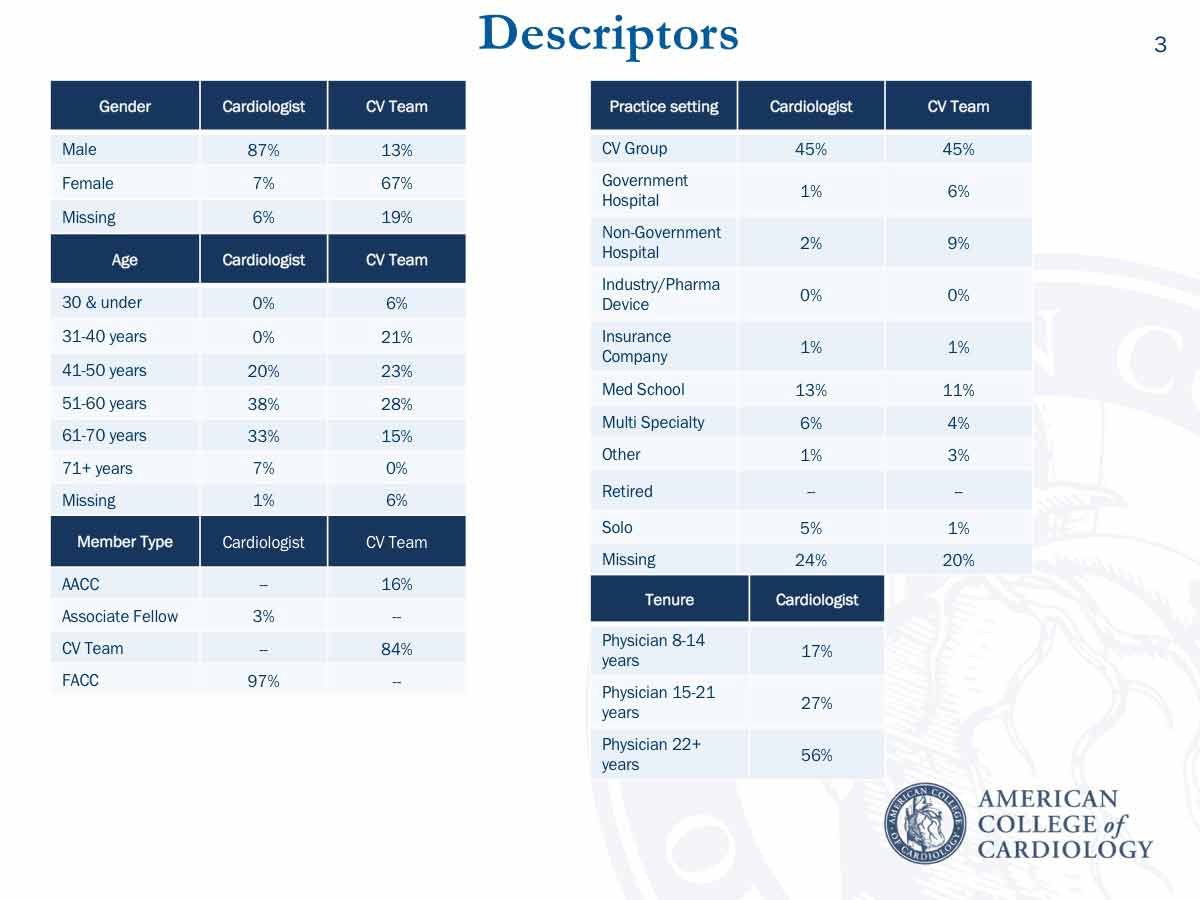
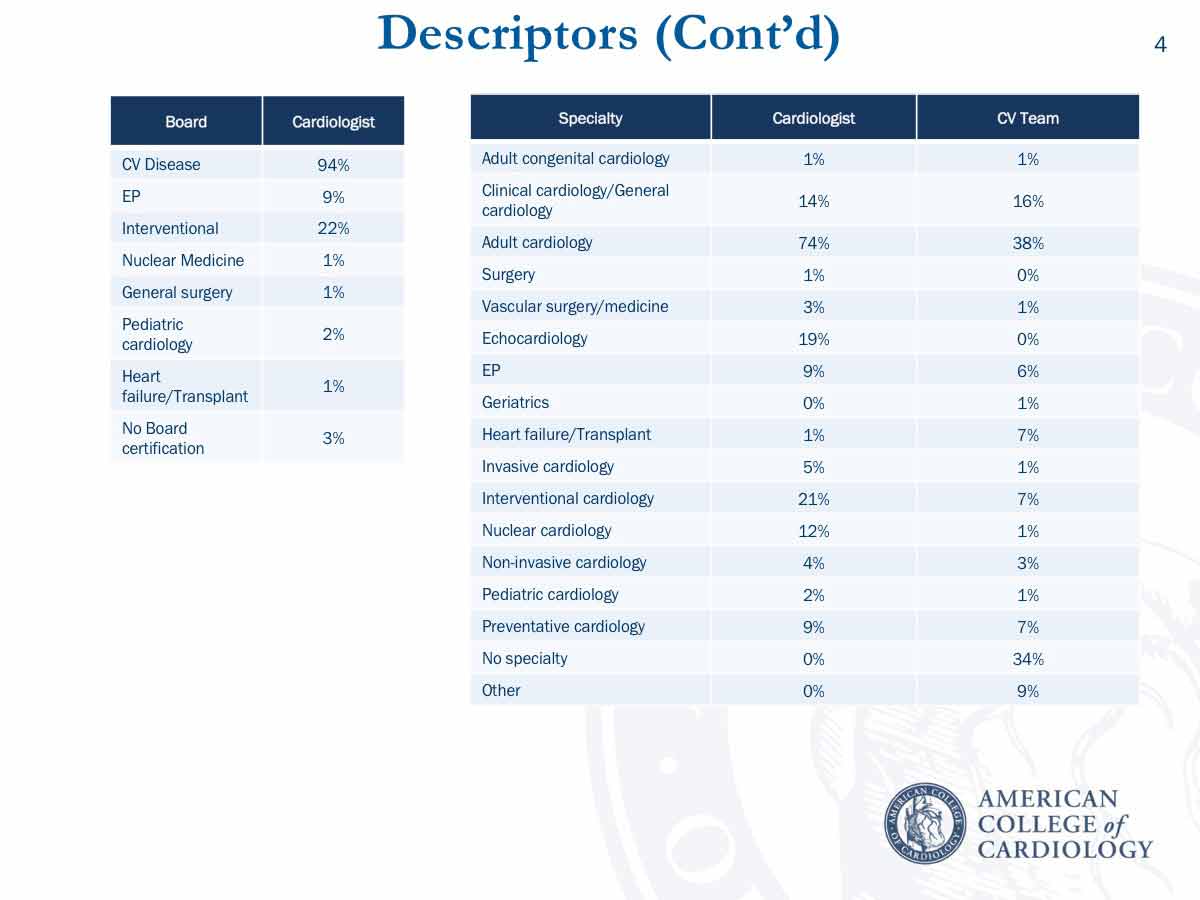
Conducted online from October to December 2017, the survey was sent to 3,648 cardiovascular specialists and had an 8 percent response rate. A total of 156 cardiologists responded. Of the 149 CV Team members who responded, 115 were a prescribing provider (nurse practitioner, physician assistant) and 10 were a clinical cardiovascular pharmacist.
Nearly all (97 percent) of the cardiologists were FACC and 16 percent of CV Team members were AACC. Most of the responding cardiologists were men (87 percent) and nearly half (46 percent) worked in a cardiovascular group and 13 percent in a medical school practice; board certification in cardiovascular disease was held by 94 percent and in interventional cardiology by 22 percent. Adult cardiology was the specialty of 74 percent and interventional cardiology of 21 percent.
Of the responding CV Team members, 67 percent were women and 45 percent worked in a cardiovascular group and 11 percent in a medical school practice setting. Adult cardiology was the specialty for 38 percent of the CV Team, clinical cardiology/general cardiology for 16 percent and 34 percent did not state a specialty.
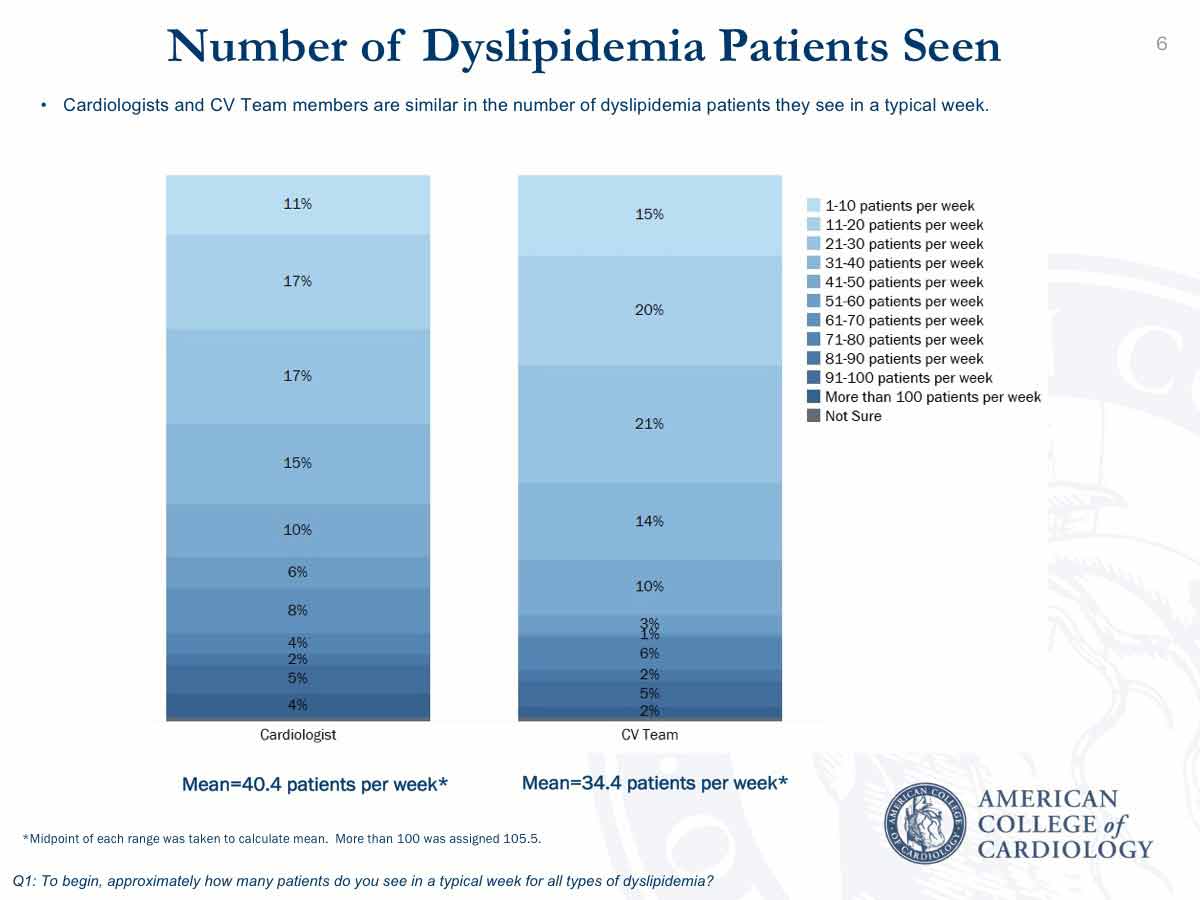
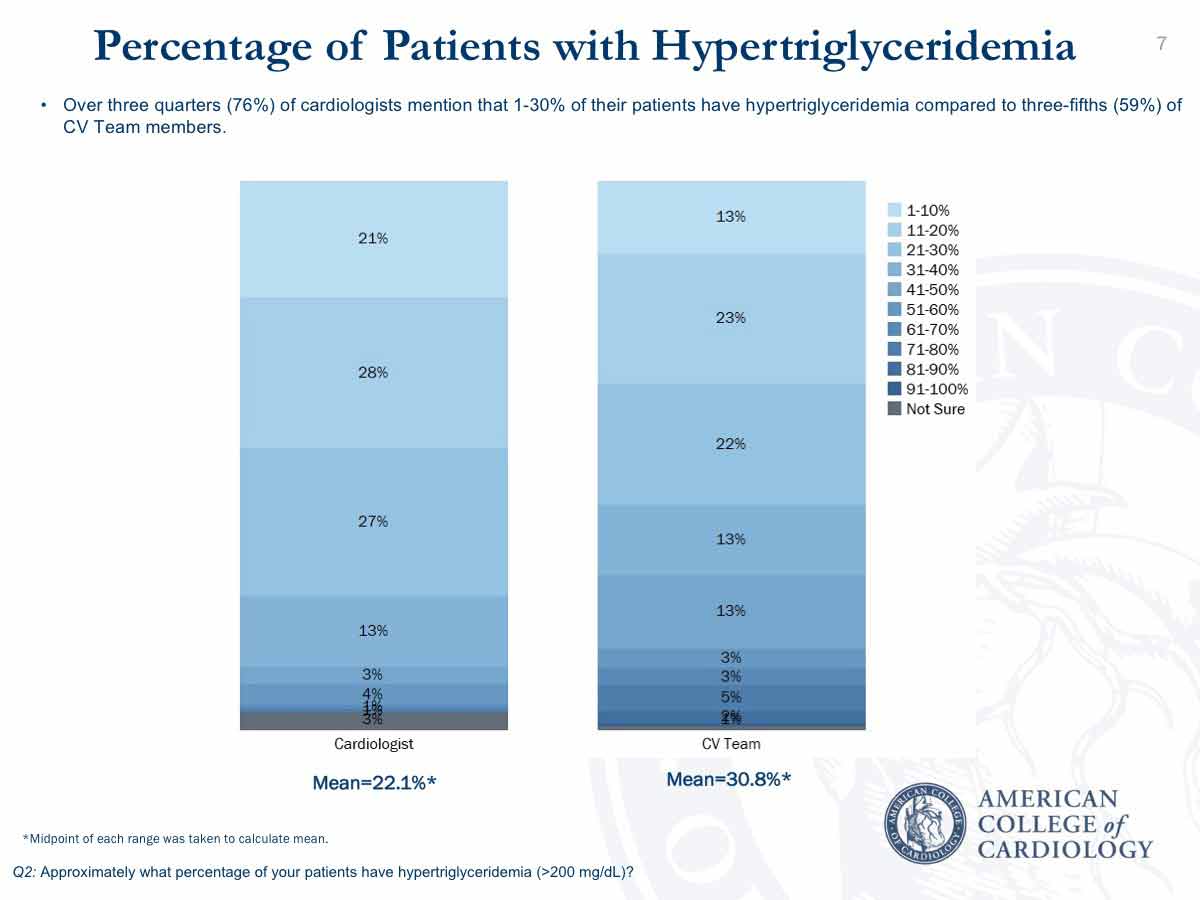
Of the respondents, the cardiologists see a mean of 40 patients with dyslipidemia a week and the CV Team members see a mean of 34 patients. In cardiology practices, a mean 22 percent of patients have a triglyceride level ≥200 mg/dL, compared with 31 percent of patients seen by CV Team members.
What Did the Survey Tell Us?
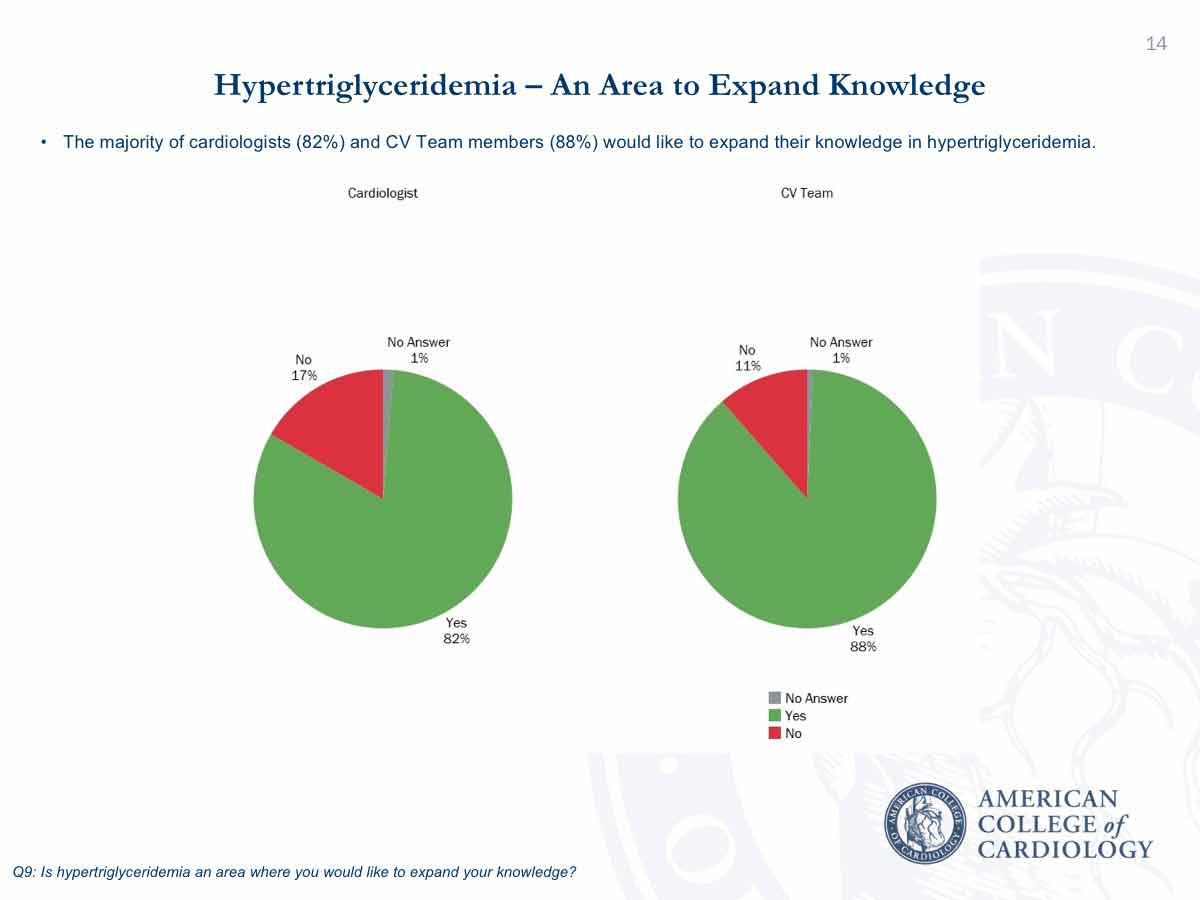
Results showed that 82 percent of the responding cardiologists and 88 percent of the responding CV Team members want more education to expand their knowledge about hypertriglyceridemia.
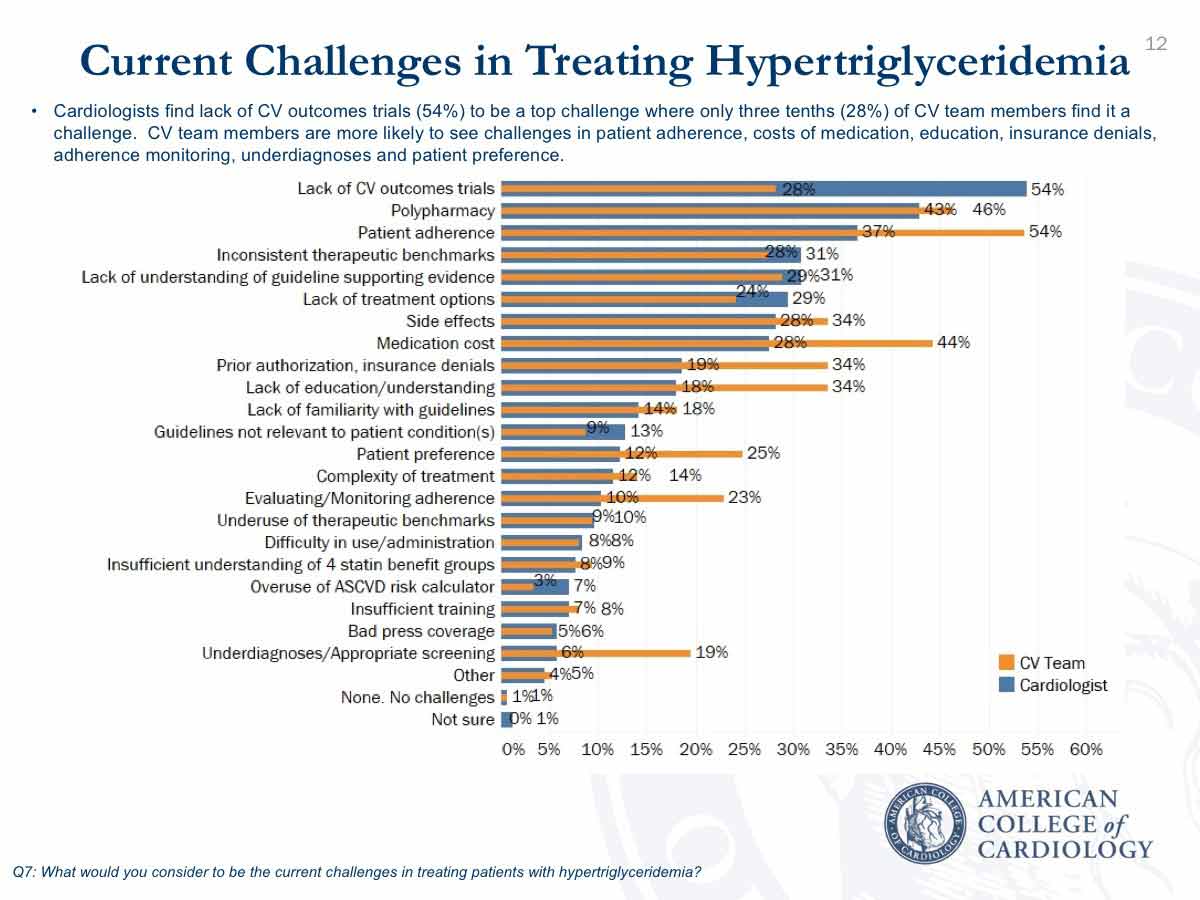
The lack of evidence from outcomes trials was cited as the primary current challenge by 54 percent of cardiologists and 28 percent of the CV Team. Patient adherence to treatment is the top challenge cited by the CV team at 54 percent, compared with 37 percent of cardiologists.
“This difference between CV Team members and cardiologists regarding the lack of clinical trial evidence and the needs for education may be influenced by the fact that some of the CV Team members who responded are not prescribing providers,” notes Sondra M. DePalma, MHS, PA-C, AACC, a certified lipid specialist. “The education, training, scope of practice and patient interactions differ within the CV Team,” she adds. The CV Team includes those who have prescribing privileges (physician assistants and advance practice nurses) and others who do not, including clinical pharmacists, registered nurses, genetic counselors and others.
Related to the need for education, a lack of education and understanding was reported by 18 percent and 34 percent of the cardiologists and CV Team members; lack of familiarity with guidelines by 14 percent and 18 percent; and lack of understanding of guideline-supporting evidence by 29 percent and 31 percent, respectively. Shapiro notes that the current ACC/American Heart Association guidelines do not provide recommendations regarding management of mild-moderate hypertriglyceridemia, because of the current lack of evidence.
“The strong interest in education represents an opportunity for ACC to develop educational products, clinical tools and practice support for members,” says DePalma.
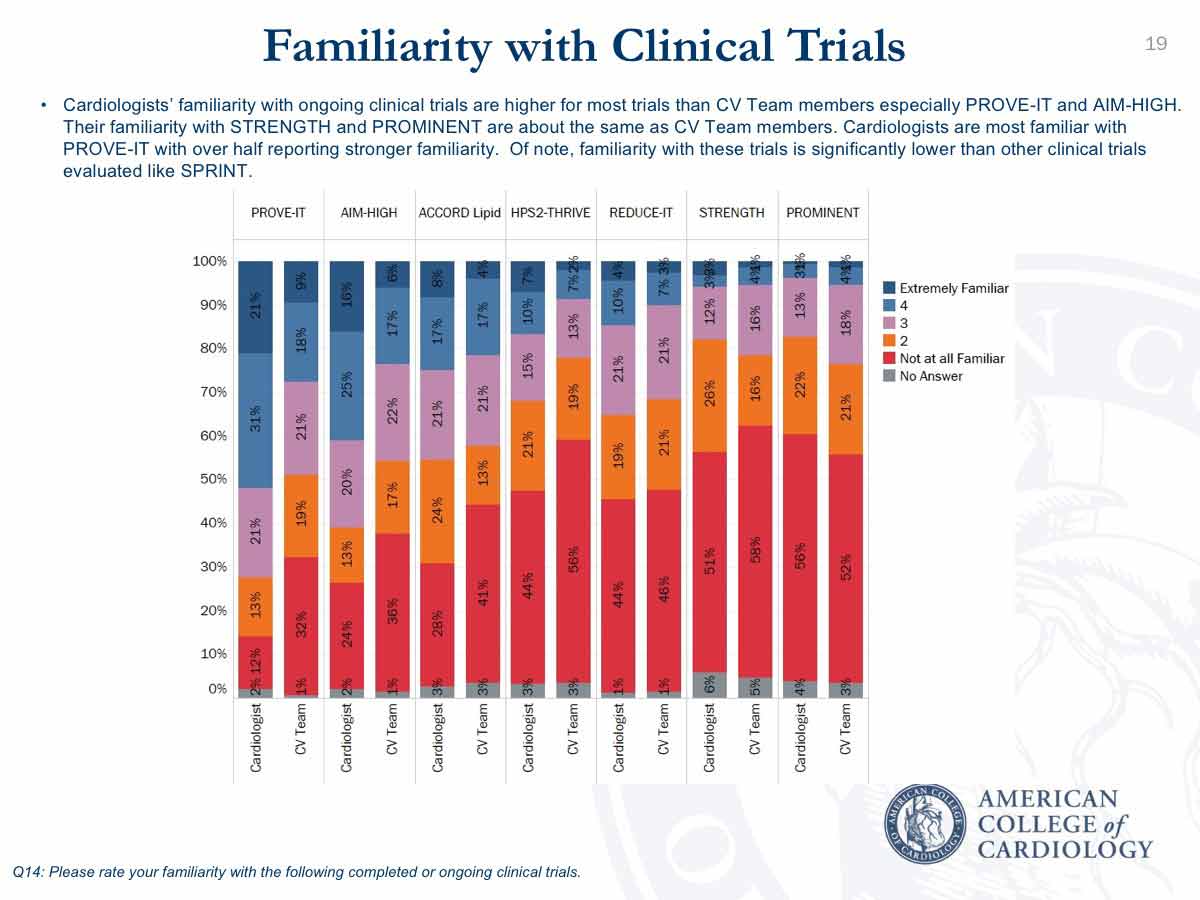
Cardiologists are more familiar with most of the lipid clinical trials than CV Team members, with about half of cardiologists and about a quarter of the CV Team extremely or very familiar with the PROVE-IT and AIM-HIGH trials. However, less than about 10 percent of both groups are familiar with the STRENGTH and PROMINENT studies. Cardiologists have slightly more familiarity with REDUCE IT (14 percent) and 10 percent of CV Team members were familiar. Notably, cardiologists were significantly less familiar with the lipid trials than with non-lipid trials listed in the survey, such as SPRINT.
Among other current challenges for treating hypertriglyceridemia are therapeutic benchmarks that are inconsistent say 31 percent and 28 percent of cardiologists and CV Team members. “Currently there aren’t any therapeutic benchmarks in the guidelines because there’s no randomized controlled clinical trial data to rely on,” says Shapiro.
"This difference between CV Team members and cardiologists regarding the lack of clinical trial evidence and the needs for education may be influenced by the fact that some of the CV Team members who responded are not prescribing providers." — Sondra M. DePalma, MHS, PA-C, AACC
Nearly a third of respondents (29 percent and 24 percent of cardiologists and CV Team members) state the lack of treatment options is a challenge. Medication cost is a challenge according to 28 percent and 44 percent, and prior authorization and insurance denials according to 19 percent and 34 percent of cardiologists and CV Team members. Shapiro notes that some of the current options, such omega-3, are expensive and often denied by insurance, which could contribute to the view that there’s a lack of treatment options.
Of the cardiologists and CV Team members, 43 percent and 46 percent say polypharmacy is a challenge and 28 and 34 percent cite side effects.
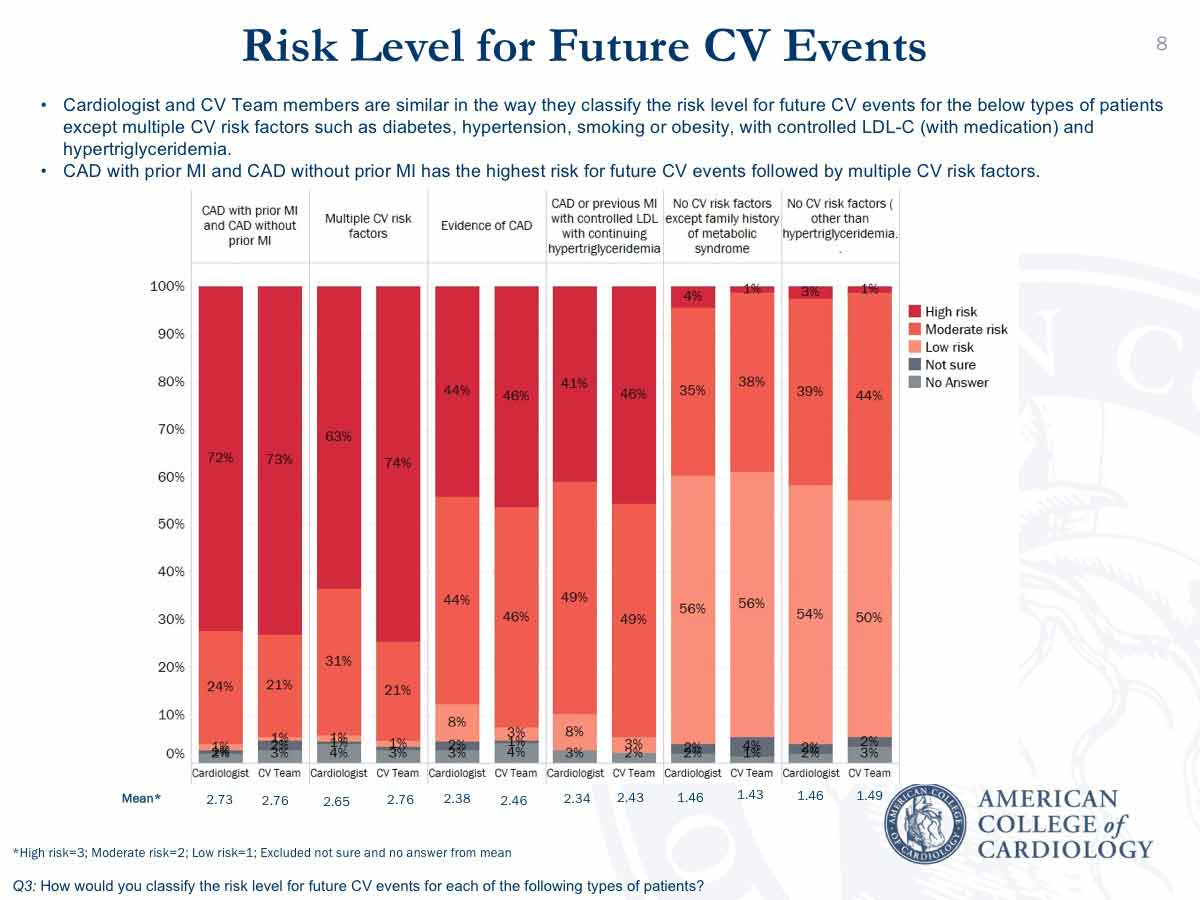
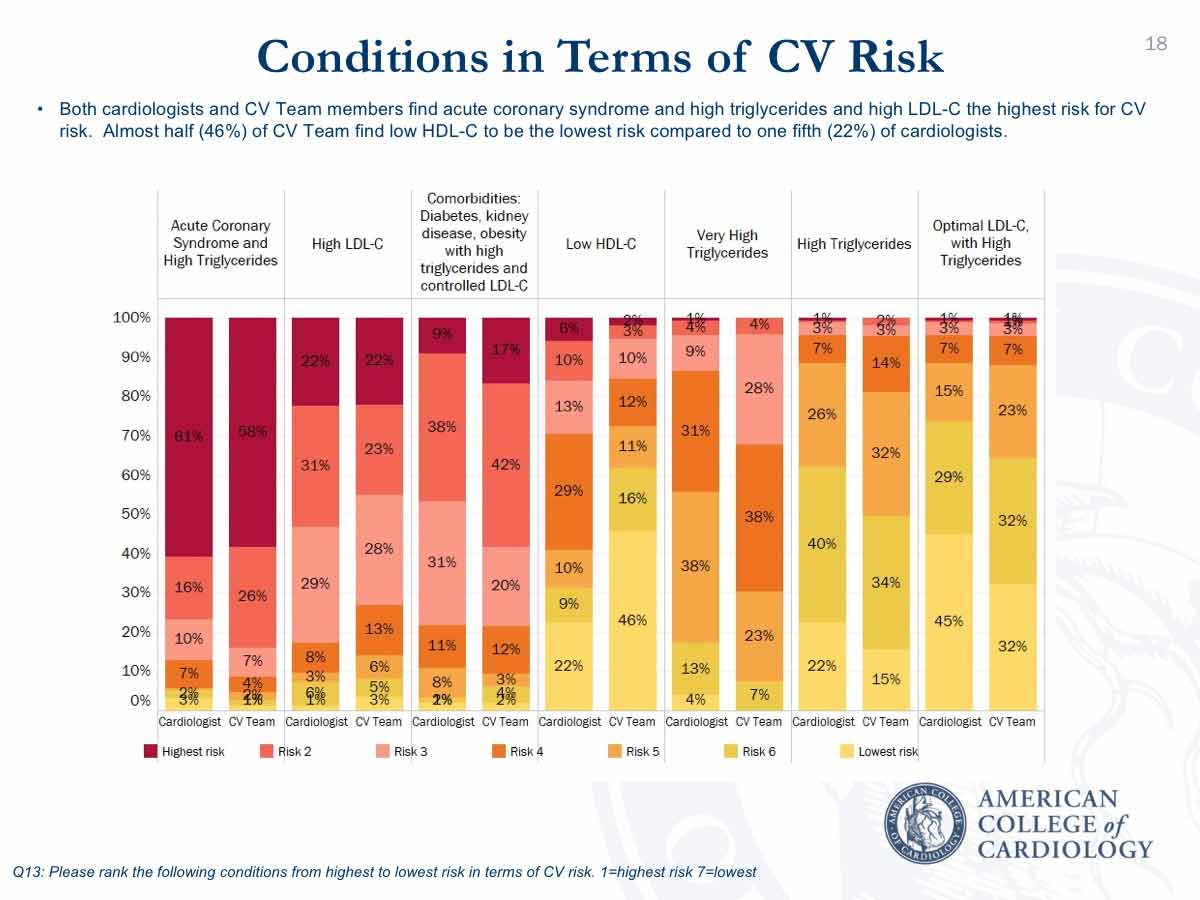
When it comes to risk, both groups share a similar perception of the patients who are at the greatest cardiovascular risk. Patients with an acute coronary syndrome (ACS) plus high triglycerides have the highest risk, say 61 percent and 58 percent of the cardiologist and CV Team respondents respectively. Twenty-two percent of each group say high LDL-C presents the highest risk.
In patients with hypertriglyceridemia and controlled LDL-C, comorbidities (diabetes, kidney disease and obesity) are thought to pose the highest risk for events by 9 percent of cardiologists and 17 percent of CV Team members. Nearly half (46 percent) of CV Team members but 22 percent of cardiologists think a low HDL-C places a patient at the lowest risk.
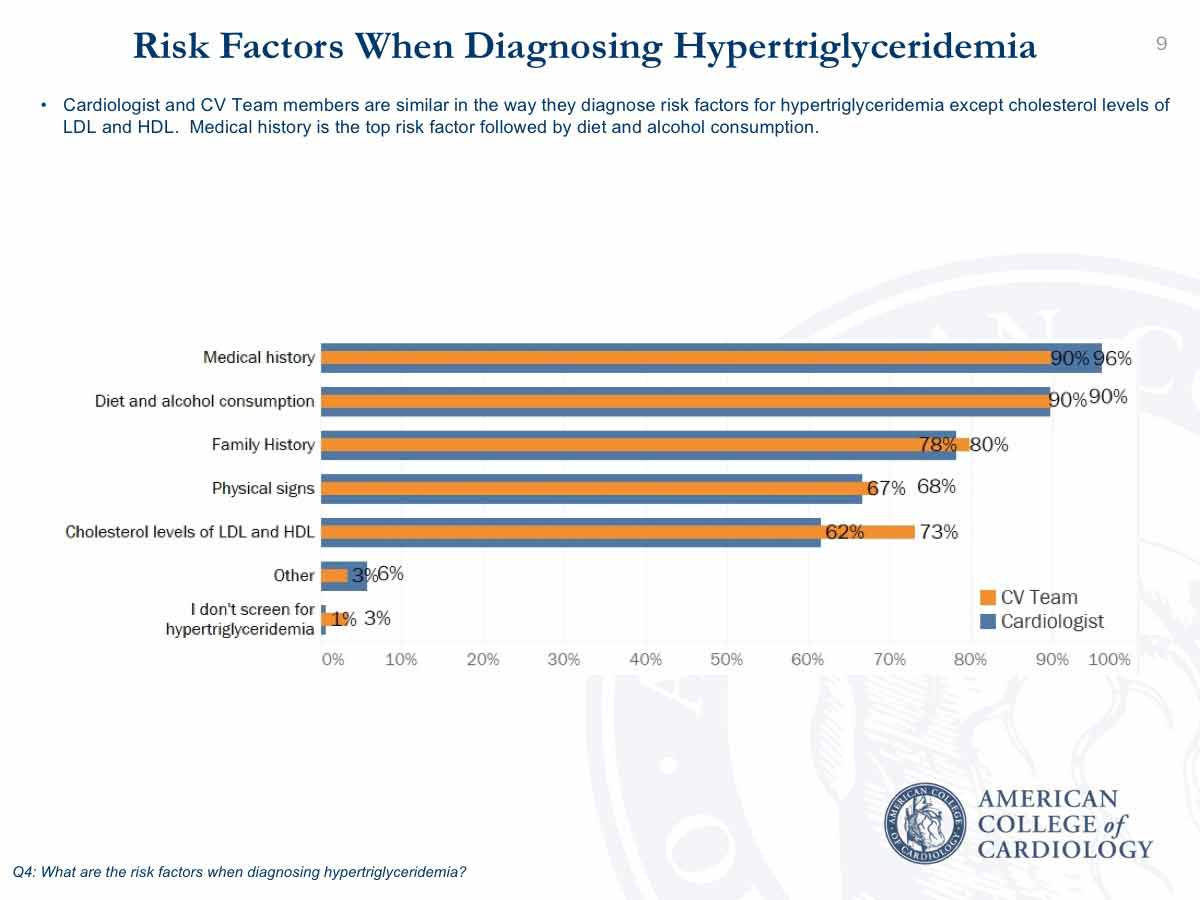
When assessing risk factors for diagnosing hypertriglyceridemia, medical history is most relied upon (by 96 percent of cardiologists and 90 percent of CV Team members) followed by diet and alcohol consumption (90 percent of each group); family history (78 percent and 80 percent); physical signs (67 percent and 68 percent); and LDL-C and HDL-C levels (62 percent and 73 percent).
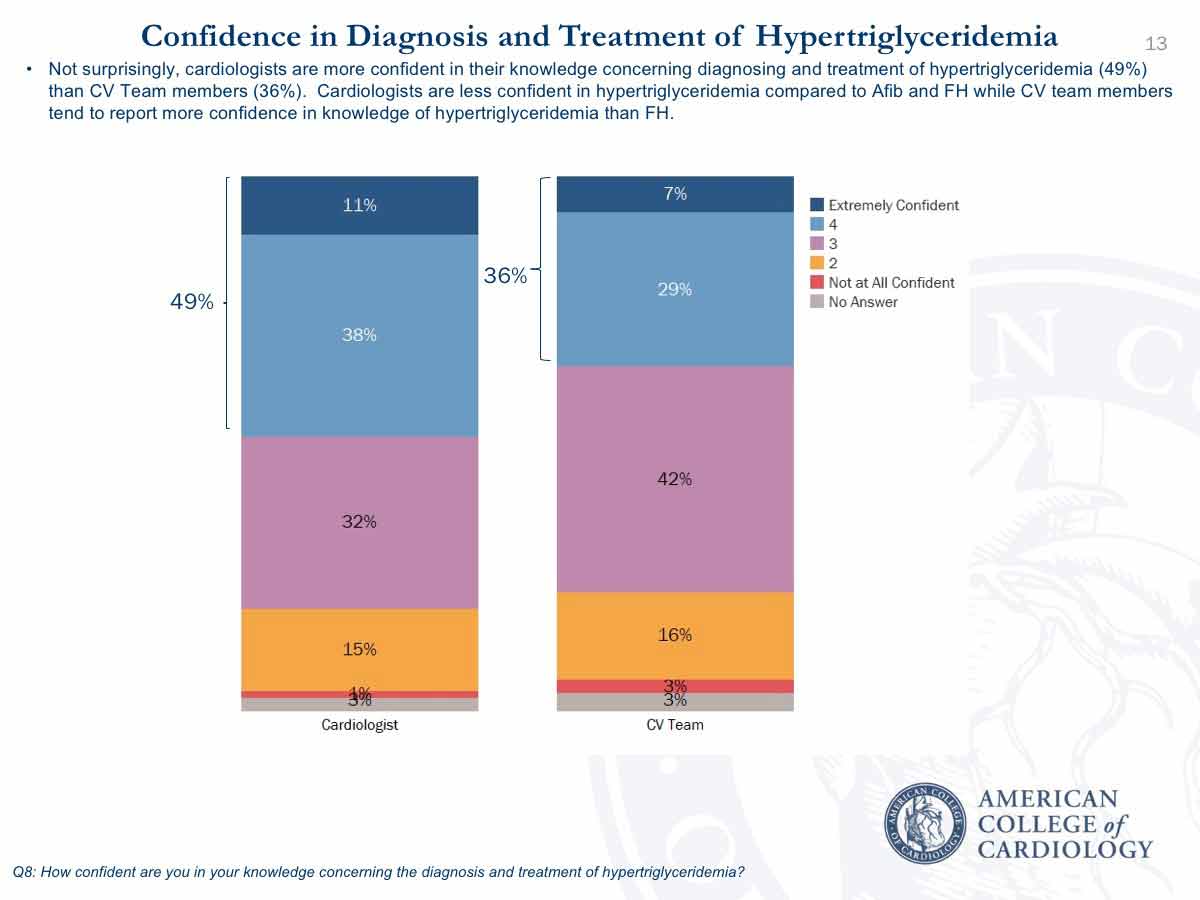
Of note, less than half of cardiologists (49 percent) and CV Team members (36 percent) state they are extremely or very confident about diagnosing and treating hypertriglyceridemia. DePalma suggests this likely reflects the lack of evidence-based treatment options, even though both groups recognize the increased cardiovascular risk for their patients with elevated triglycerides.
Cardiologists are less confident regarding hypertriglyceridemia than atrial fibrillation and familial hypercholesterolemia. CV Team members are more confident in their knowledge of hypertriglyceridemia than familial hypercholesterolemia.
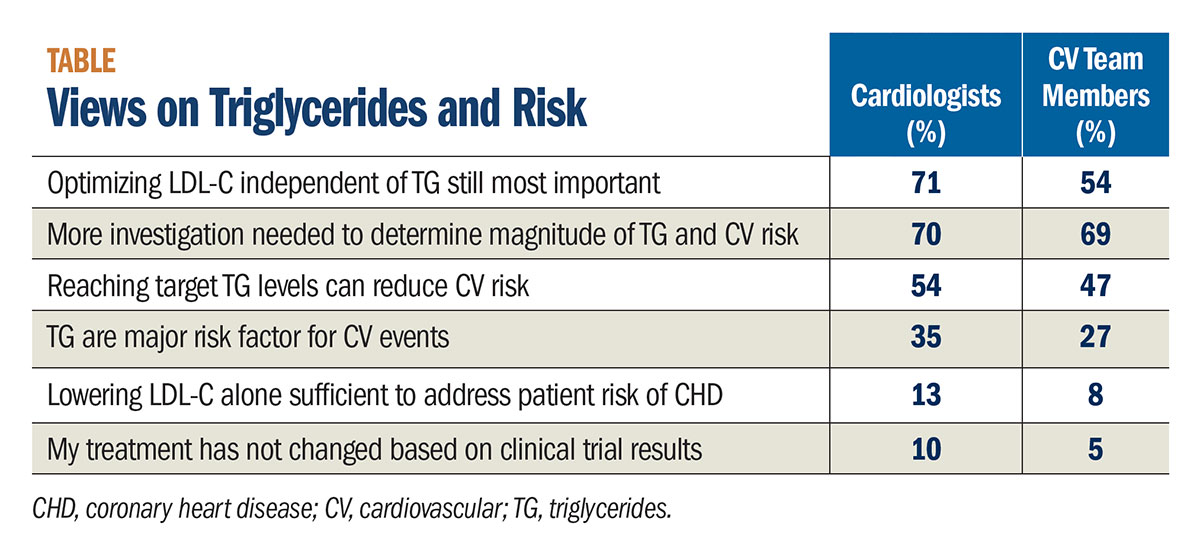
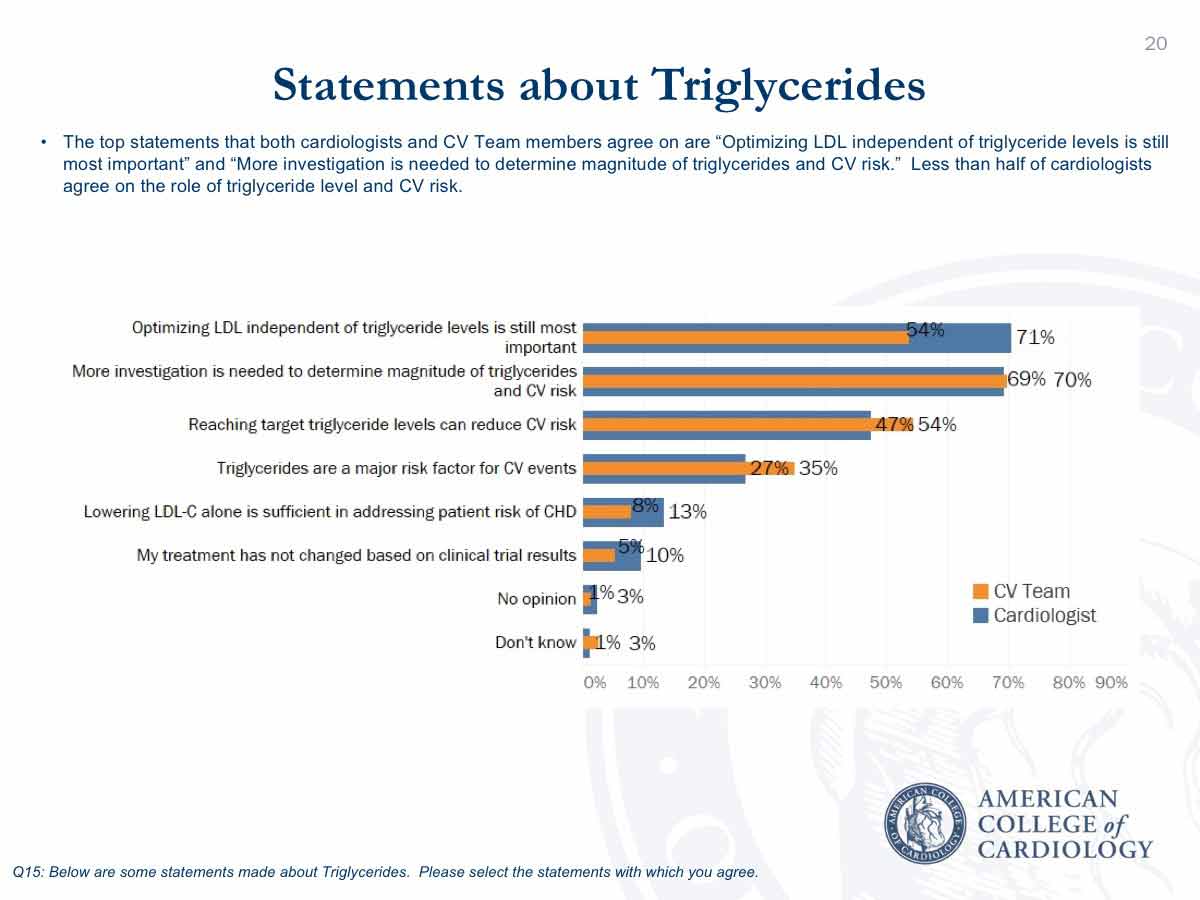
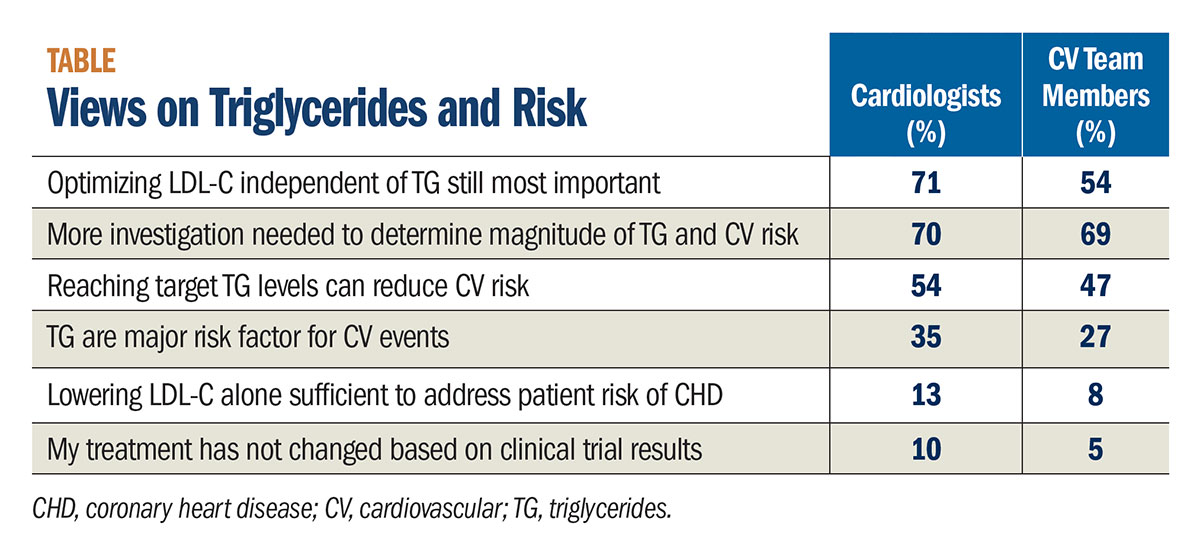
Another common perception among cardiologists and CV Team respondents is that the most important step to reducing risk is to optimize LDL-C levels independent of triglyceride levels (71 percent and 54 percent, respectively). More investigation is needed to determine the magnitude of the risk of triglycerides, according to 70 percent of both groups.
Fifty-four percent of cardiologists and 47 percent of CV Team members say that reaching target triglyceride levels can reduce risk, and 27 percent and 35 percent say that triglycerides are a major risk factor for CV events. Just 13 percent of cardiologists and 8 percent of CV Team members think lowering LDL-C alone is sufficient to address risk.
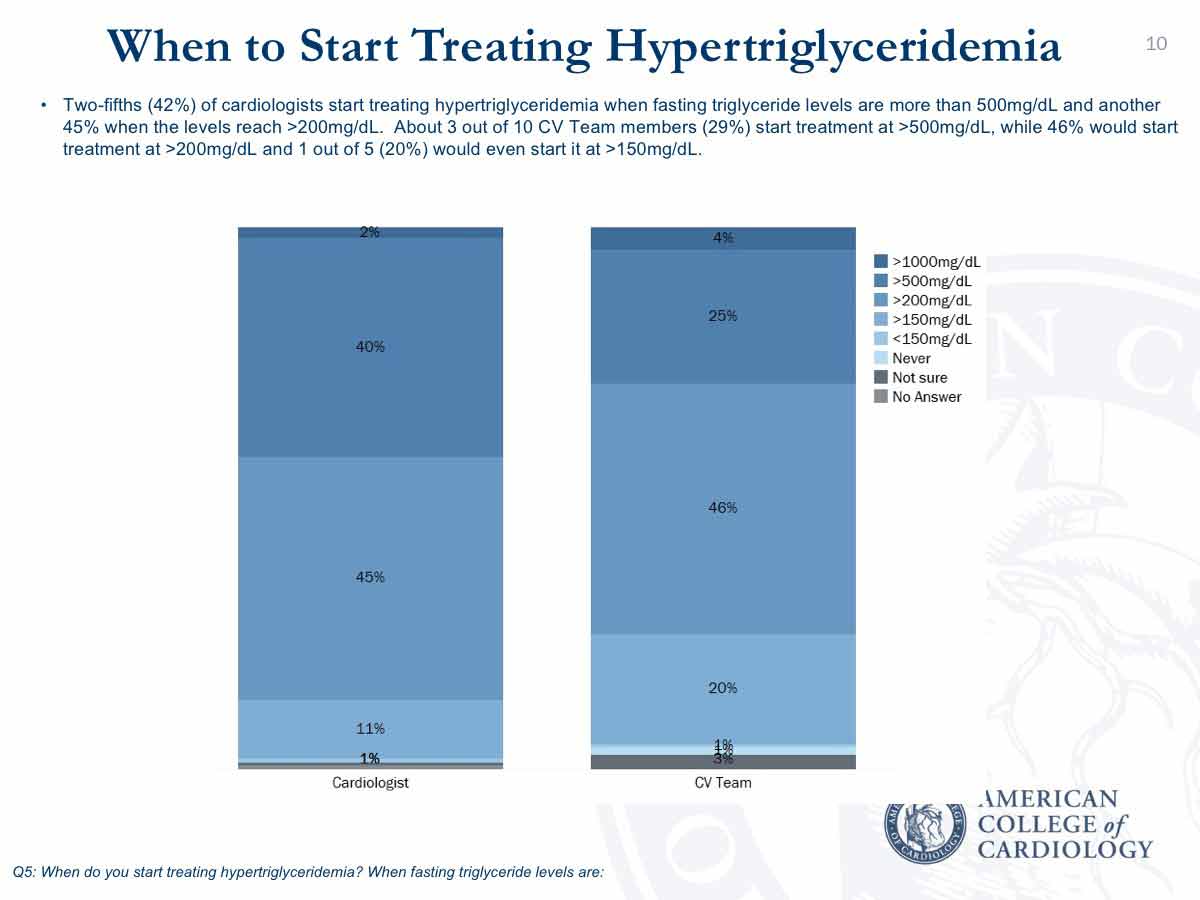
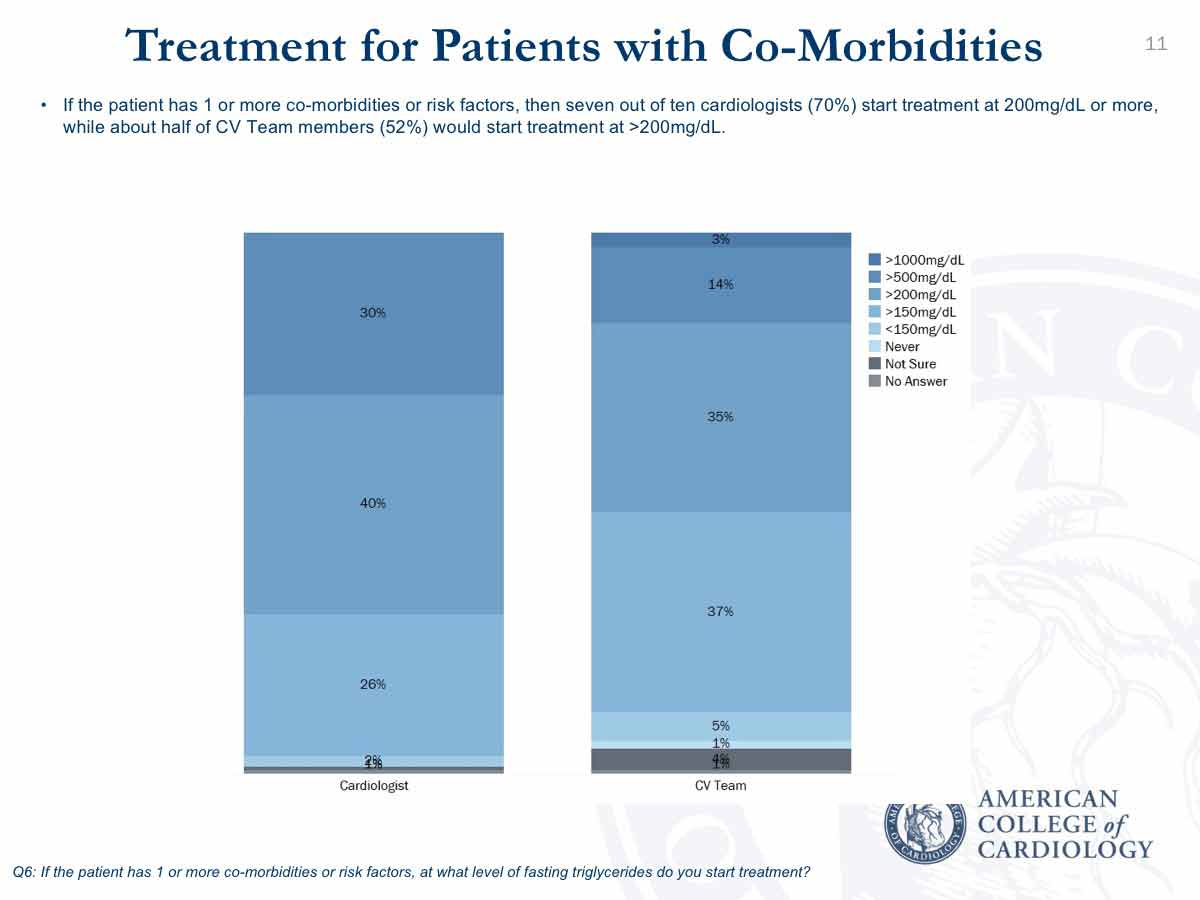
When do they start treatment of hypertriglyceridemia? Among cardiologists, 45 percent start when fasting triglycerides are >200 mg/dL and 42 percent start when the levels are >500 mg/dL. For CV Team members, 20 percent start treatment when fasting triglycerides exceed 150 mg/dL, 46 percent when they are >200 mg/dL and 29 percent start when the levels are >500 mg/dL. The threshold for treatment is lower for both cardiologists and CV Team members when a patient has one or more risk factors or comorbidities, with 70 percent and 52 percent respectively starting treatment when triglycerides exceed 200 mg/dL.
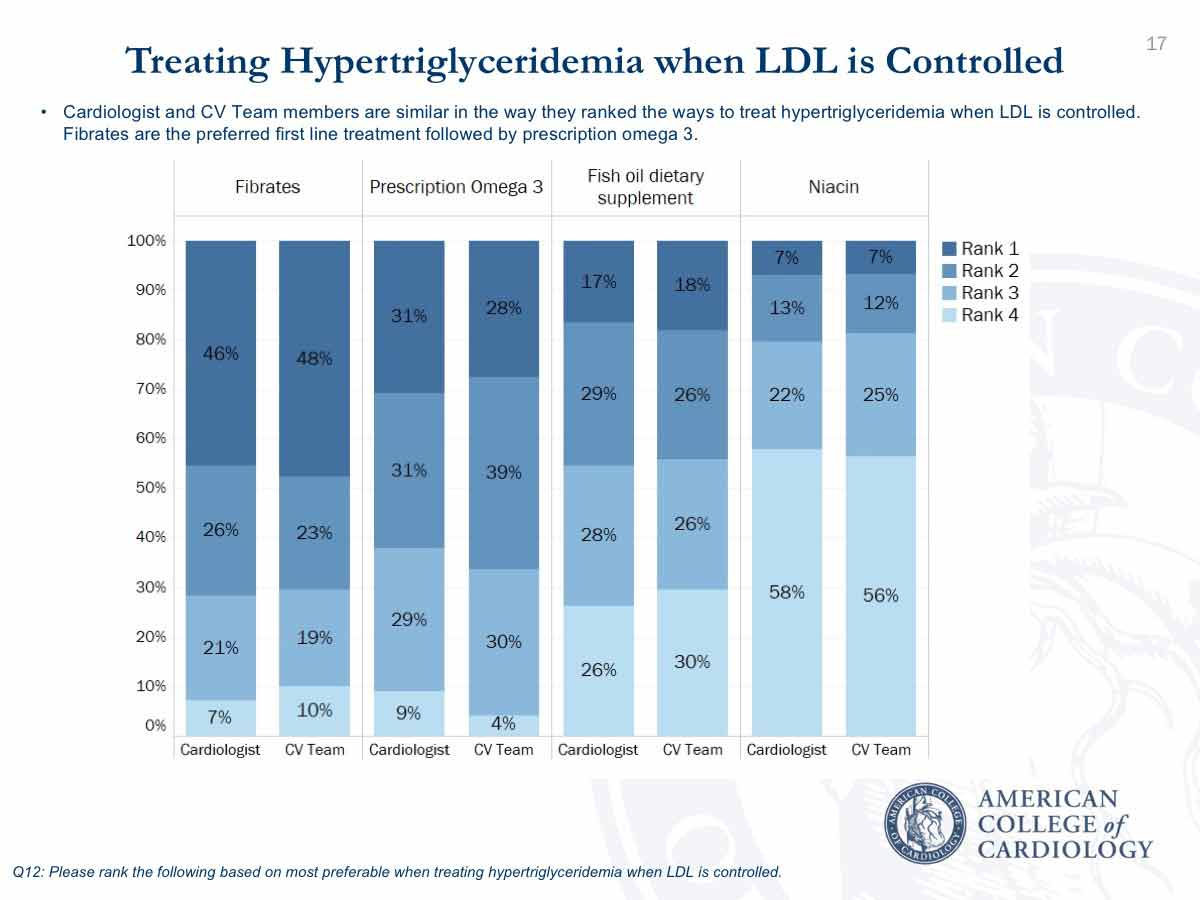
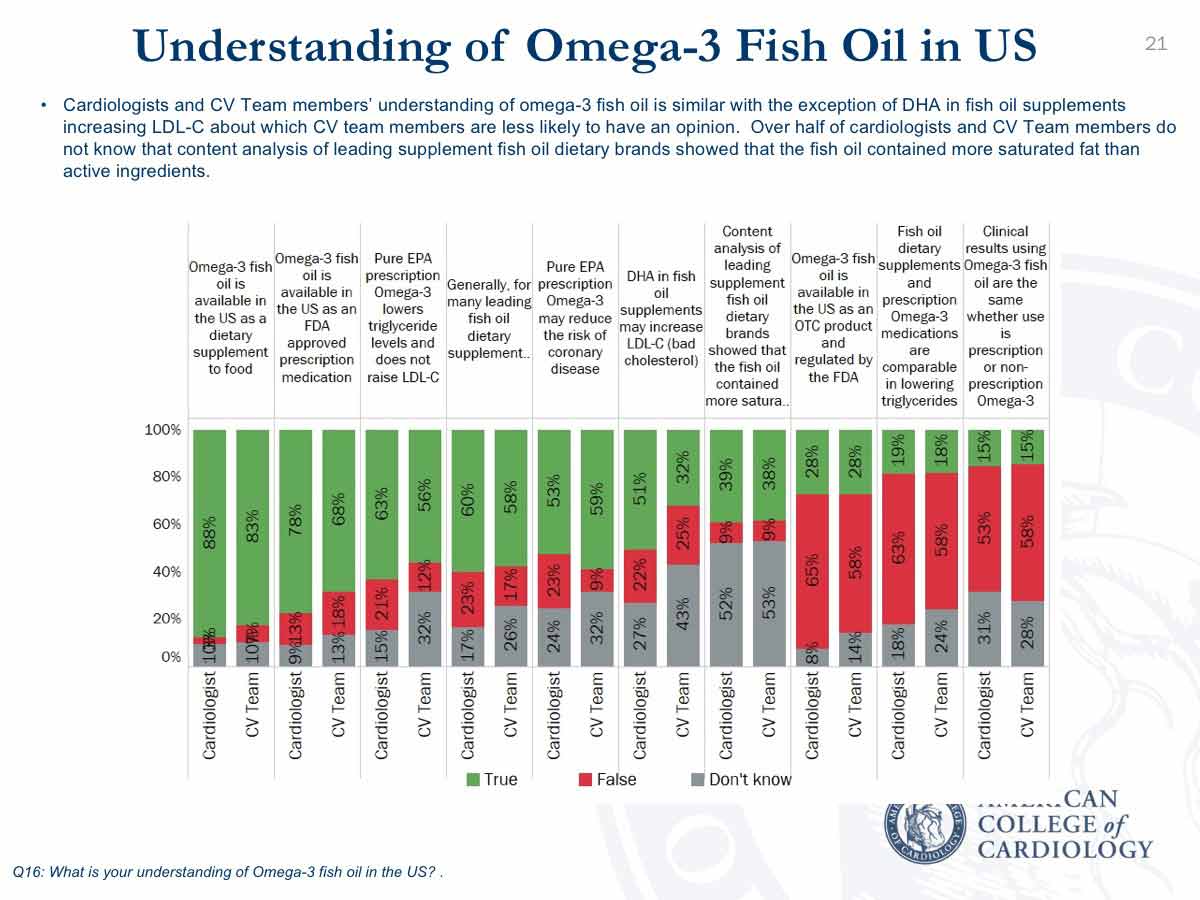
Interestingly, when it comes to treating patients with controlled LDL-C but elevated triglycerides, cardiologists and CV Team members alike first reach for fibrates (46 and 48 percent respectively) and then prescription Omega-3 (31 percent and 28 percent). Only about 17 percent of both ranked fish oil dietary supplement as their first choice and it was niacin for only 7 percent of both groups.
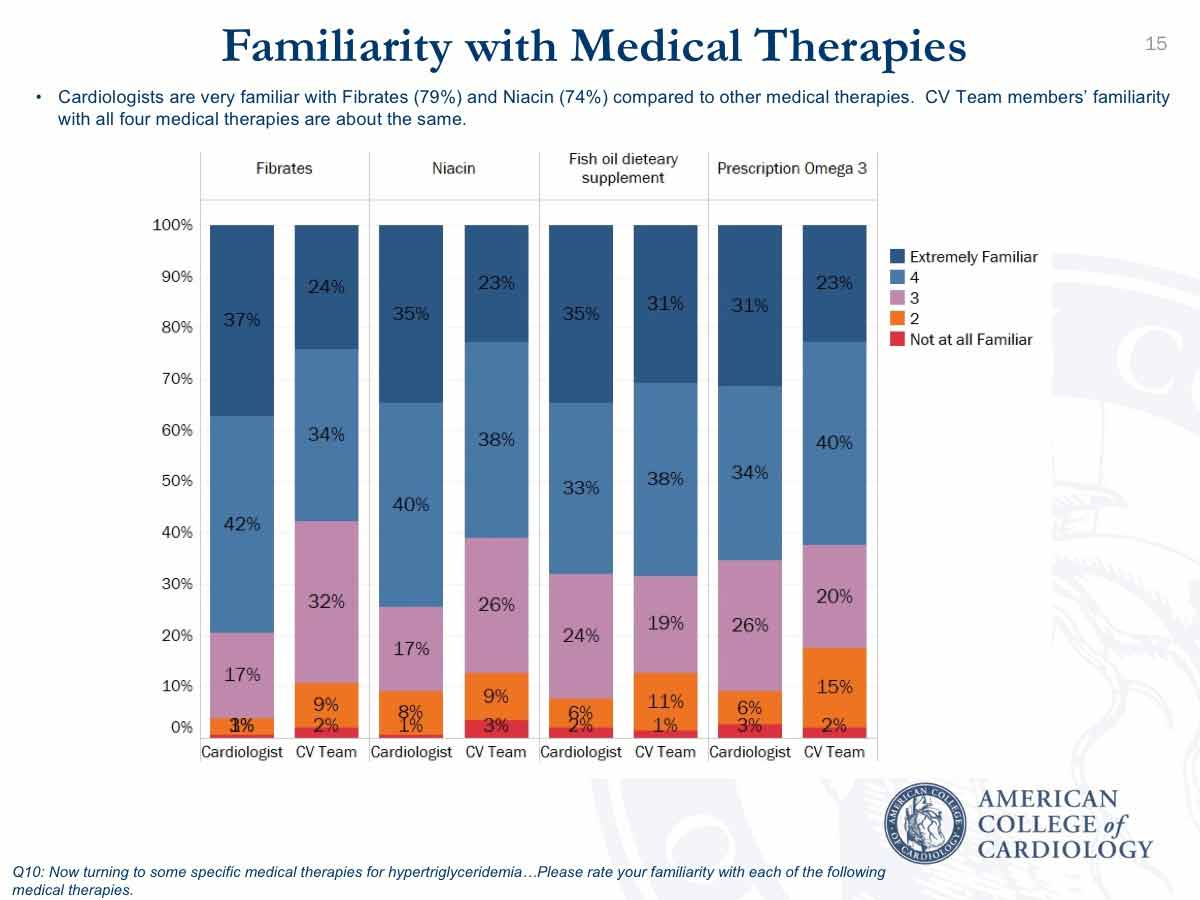
Regarding familiarity with available medical therapies, more cardiologists are extremely or very familiar with fibrates and niacin (79 percent and 74 percent), compared with fish oil dietary supplements and prescription omega-3 (68 percent and 65 percent). About 60 percent of CV Team members were extremely or very familiar with each category.
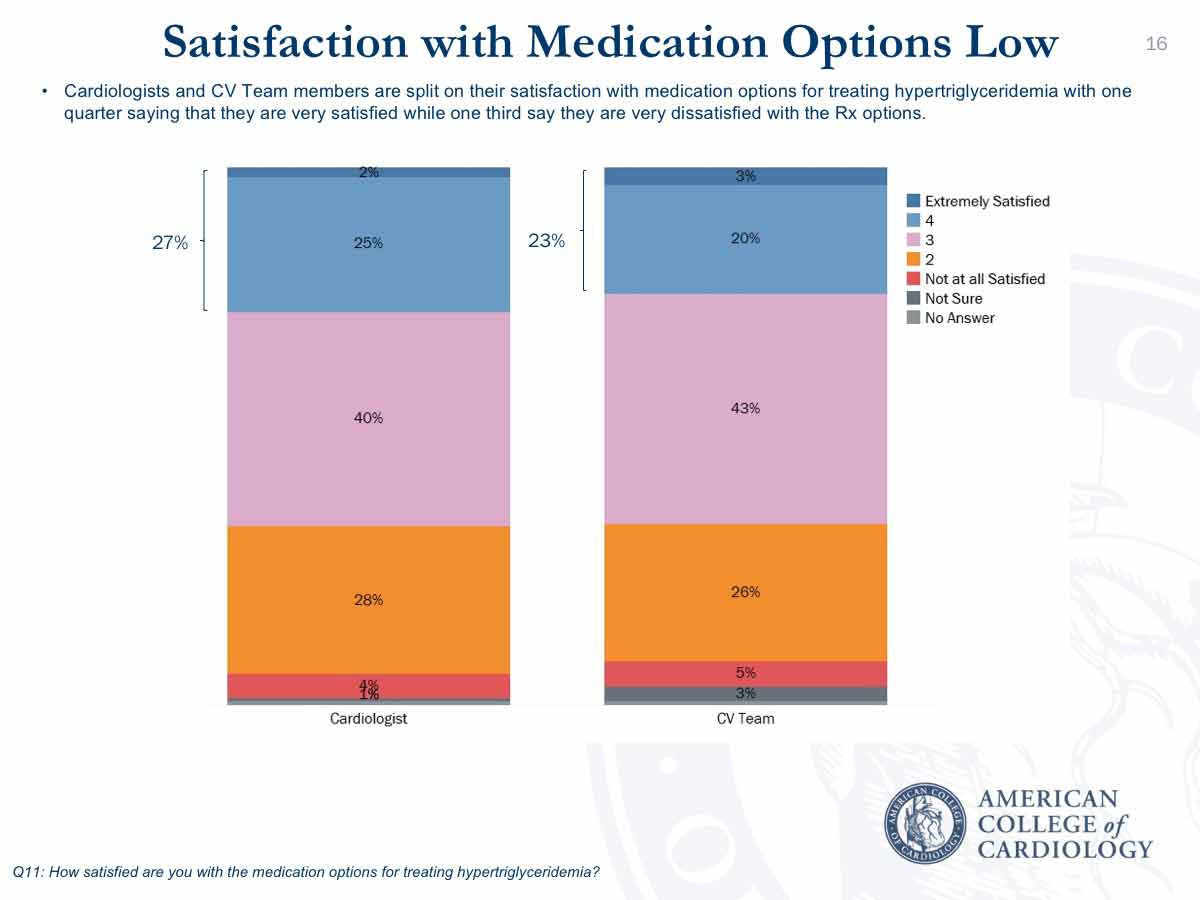
Importantly, there’s low satisfaction with current medication options to treat hypertriglyceridemia. Only 27 percent of cardiologists and 23 percent of CV Team respondents are satisfied – and 32 percent and 31 percent and very dissatisfied. Both Shapiro and DePalma suggest the lack of evidence-based data could be contributing to this dissatisfaction, along with frustration with payer denials for current treatment options.
“Overall, these survey results indicate that clinicians take triglycerides seriously and recognize the impact on cardiovascular risk, particularly in their high-risk patients,” says Shapiro. “Few respondents treated patients with moderately elevated triglycerides (200-500 mg/dL) and REDUCE-IT will help to answer whether moderately elevated triglycerides should be treated in patients with manifest vascular disease who’ve achieved a good LDL-C level.”
This research was sponsored by Amarin.
Clinical Topics: Acute Coronary Syndromes, Arrhythmias and Clinical EP, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Atrial Fibrillation/Supraventricular Arrhythmias, Hypertriglyceridemia, Lipid Metabolism, Nonstatins, Novel Agents, Primary Hyperlipidemia, Statins, Diet
Keywords: ACC Publications, Cardiology Magazine, Acute Coronary Syndrome, Alcohol Drinking, American Heart Association, Angina, Unstable, Atherosclerosis, Atrial Fibrillation, Benchmarking, Carboxylic Acids, Cardiovascular Diseases, Certification, Comorbidity, Counseling, Diabetes Mellitus, Diabetes Mellitus, Type 2, Diet, Dietary Supplements, Eicosapentaenoic Acid, Fasting, Fatty Acids, Omega-3, Fibric Acids, Frustration, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Hyperlipoproteinemia Type II, Hypertriglyceridemia, Kidney Diseases, Lipids, Myocardial Infarction, Niacin, Nurse Practitioners, Obesity, Patient Compliance, Pharmacists, Physician Assistants, Polypharmacy, Risk Factors, Schools, Medical, Specialization, Stroke, Triglycerides, Vascular Diseases, Triglycerides
< Back to Listings