Cover Story | New ACC/AHA Cholesterol Guideline: Personalized, Patient-Centered Care; New Treatment Options
The new 2018 ACC/AHA Guideline on the Management of Blood Cholesterol allows for more personalized care for patients compared with its 2013 predecessor. Among the biggest changes: more detailed risk assessments and new cholesterol-lowering drug options for people at the highest risk for atherosclerotic cardiovascular disease (ASCVD).
"High cholesterol treatment is not one size fits all, and this guideline strongly establishes the importance of personalized care," says ACC President C. Michael Valentine, MD, FACC. "Over the past five years, we've learned even more about new treatment options and which patients may benefit from them. By providing a treatment roadmap for clinicians, we are giving them the tools to help their patients understand and manage their risk and live longer, healthier lives."
Among these tools are risk-enhancing factors that help cardiovascular professionals better determine individualized risk and treatment options, as well as coronary artery calcium scores, a second-line decision tool that has been "more fully integrated into the guidelines," says Michael Shapiro, DO, FACC, chair of the Dyslipidemia and Familial Hypercholesterolemia Work Group of ACC's Prevention of Cardiovascular Disease Section.
For primary prevention of ASCVD, there's a step-wise approach to refining risk estimation in the guideline. The risk categories, based on 10-year risk using the race- and sex-specific Pooled Cohort Equations, are low (<5 percent), borderline (5-7.5 percent), intermediate (>7.5-20 percent) and high (≥20 percent).
"The comprehensive list of risk enhancing factors can guide and refine decision-making and is especially useful in the large group of adults in the U.S. who fall into the newly defined category of intermediate risk," says Shapiro. When the risk decision remains unclear, the coronary artery calcium scores can be a tie-breaker.
Shapiro cautions, however, that the utility of a coronary artery calcium score is less certain in those who are smokers, have diabetes or a strong family history. Among patients with a score of 1-99, he suggests that any degree of coronary calcium may support starting statin therapy, particularly those older than 55 years. Statin therapy is clearly indicated for patients with a calcium score of >100 or >75th percentile for age and gender.
"The decision to use statin therapy should be determined through a discussion between the patient and clinician," says Shapiro. This patient risk discussion, which has a Class I recommendation in the new guideline, should include a review of risk enhancers. As with all shared decision-making conversations, it should also address the patient's values in terms of cost, potential for benefit and adverse effects, and drug-drug interactions.
The new guideline also calls for assessing adherence and percentage response to LDL-C lowering treatment and lifestyle changes with repeat lipid measurements at four to 12 weeks after statin initiation or dose adjustments, repeated every three to 12 months as needed. A maximally tolerated statin dose to lower LDL-C by ≥50 percent is recommended.
Recognizing the cumulative effect of high cholesterol over the full lifespan, identifying and treating it early can help reduce the lifetime risk for cardiovascular disease. The new guideline suggests elective cholesterol screening is appropriate for children as young as two who have a family history of heart disease or high cholesterol.
In most children, an initial screening test can be considered between the ages of nine and 11 and then again between 17 and 21. Because of a lack of sufficient evidence in young adults, there are no specific recommendations for that age group. However, it is essential they adhere to a healthy lifestyle, be aware of the risk of high cholesterol levels and get treatment as appropriate at all ages to reduce the lifetime risk of heart disease and stroke.
"Having high cholesterol at any age increases that risk significantly. That's why it's so important that even at a young age, people follow a heart-heathy lifestyle and understand and maintain healthy cholesterol levels," says AHA President Ivor Benjamin, MD, FACC.
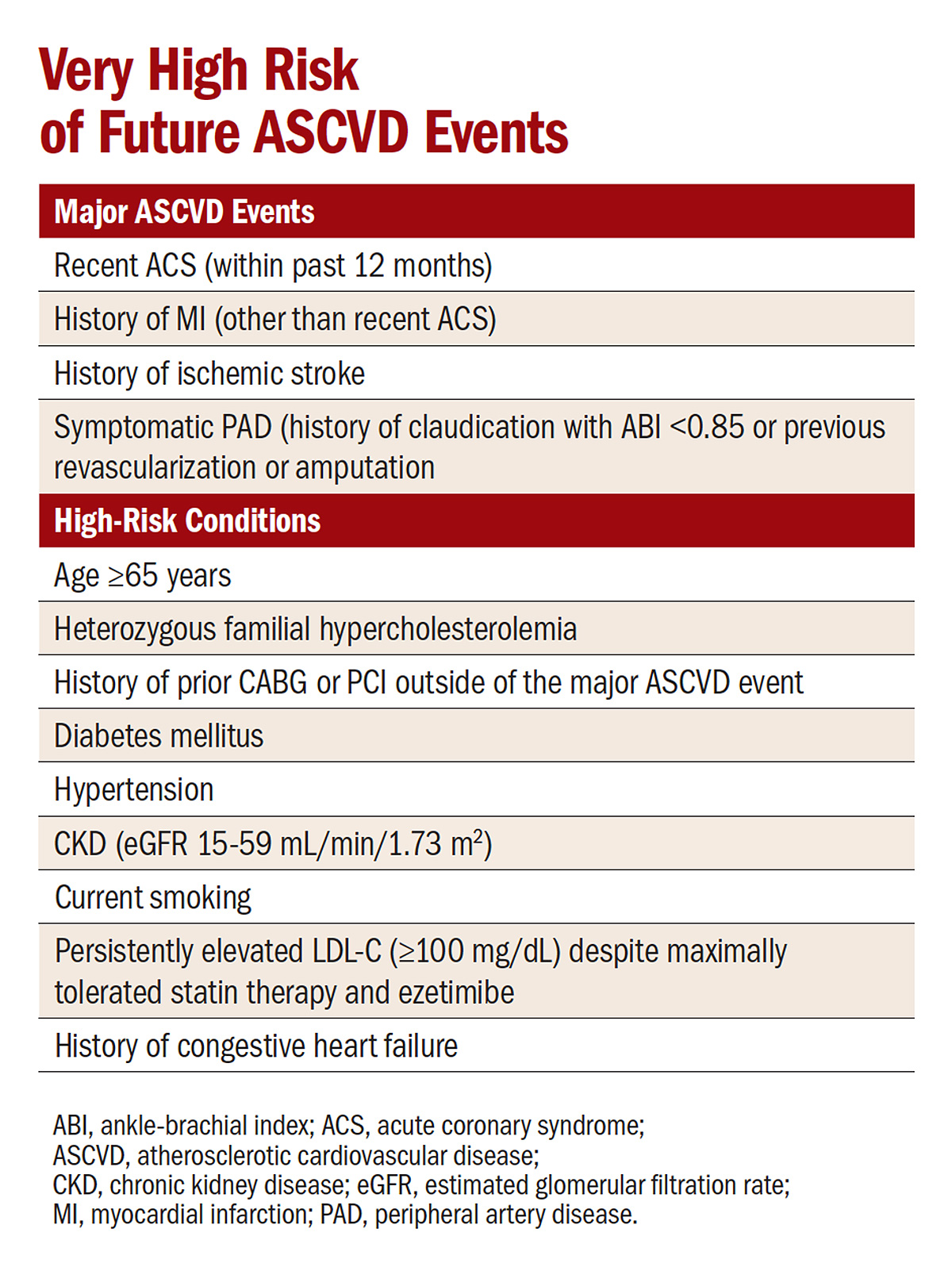
The guideline also sets out very specific recommendations for clinicians to discuss options with patients in the newly defined "very high risk of ASCVD" category who still have LDL-C ≥70 mg/dL after maximizing statin therapy (Table). It recommends considering other nonstatin drugs, including ezetimibe and PCSK9 inhibitors.
Adding ezetimibe is reasonable and recommended before adding a PCSK9 inhibitor. Further, the guideline states that if the patient is on clinically judged maximal LDL-C lowering therapy and LDL-C remains ≥70 mg/dL or non–HDL-C is ≥100 mg/dL it is reasonable to add a PCSK9 inhibitor.
For patients with severe primary hypercholesterolemia (LDL-C ≥190 mg/dL), the guideline recommends starting high-intensity statin therapy without calculating the 10-year ASCVD risk; if LDL-C remains ≥100 mg/dL adding ezetimibe is reasonable. A PCSK9 inhibitor may be considered if the LDL-C remains ≥100 mg/dL on therapy with a statin and ezetimibe if the patient has risk factors for subsequent ASCVD.
For the first time, the new guideline also includes a Value Statement that underscores the need for clinicians and patients to factor in the cost of drugs in determining the most appropriate treatment strategy. Based on pricing through mid-2018, the guideline gives PCSK9 inhibitors a low-cost value (>$150,000 per QALY) for patients at very high risk of ASCVD and uncertain value for patients with familial hypercholesterolemia compared with a good cost value (<$50,000 per QALY).
However, it remains to be seen if recent reductions in pricing by both Amgen and Sanofi-Regeneron as part of broader efforts to improve patient access, as well as results from studies like ODYSSEY OUTCOMES (see sidebar), could alter this value equation down the road.
"ACC is committed to helping physicians with access to care issues, while also bringing together stakeholders, including payer, industry and clinician representatives, to talk about opportunities to move forward together," Valentine adds. "We recognize recent efforts to lower cost and increase transparency for patients. Our goal is to make sure the highest risk patients have access to the care they need."
"The new ACC/AHA clinical practice guideline on management of blood cholesterol provides clinicians with useful guidance regarding up-to-date management of blood lipids. It merges excellent clinical science with logical and precise clinical judgment," says James L. Januzzi, MD, FACC, chair of ACC's Task Force on Expert Consensus Decision Pathways and incoming member of the Board of Trustees.
Looking ahead, with the release of the new guideline for the treatment of blood cholesterol, as well as recent changes in drug pricing and the release of the ODYSSEY OUTCOMES results, the College plans to review its current Expert Consensus Decision Pathway over the next six to 12 months to evaluate the pragmatic translation of these new data points.
While the current pathway remains relevant, especially the regular evaluation of the holistic view of the patient's treatment, the writing group will evaluate other enhancements that could further support translation for individual patients.
Clinical Topics: Acute Coronary Syndromes, Cardiac Surgery, Cardiovascular Care Team, Dyslipidemia, Invasive Cardiovascular Angiography and Intervention, Prevention, Cardiac Surgery and Arrhythmias, Homozygous Familial Hypercholesterolemia, Lipid Metabolism, Nonstatins, Novel Agents, Primary Hyperlipidemia, Interventions and ACS, Smoking
Keywords: ACC Publications, Cardiology Magazine, Acute Coronary Syndrome, Angina, Unstable, Antibodies, Monoclonal, Anticholesteremic Agents, Atherosclerosis, Brain Ischemia, Calcium, Cholesterol, Cohort Studies, Consensus, Coronary Vessels, Cost-Benefit Analysis, Decision Making, Diabetes Mellitus, Diagnosis-Related Groups, Drug Interactions, Follow-Up Studies, Heart Diseases, Hospitalization, Hypercholesterolemia, Hyperlipoproteinemia Type II, Intention to Treat Analysis, Life Style, Lipids, Medicare, Myocardial Infarction, Myocardial Revascularization, Primary Prevention, Quality of Life, Quality-Adjusted Life Years, Risk Assessment, Risk Factors, Smoking, Stroke, Writing
< Back to Listings