Exercise Before, During, and After Cancer Therapy
Introduction
Early detection of cancer and its effective management have considerably improved the 5-year disease-survival rates of common malignancies. However, cancer and its treatment have physical, psycho-physical, and psychological adverse effects. These can be acute or short-duration symptoms that develop before or during cancer therapy, chronic symptoms that persist for months or years during cancer treatment, and late symptoms that develop months or years after treatment. These symptoms (Table 1) adversely affect the quality of lives of patients with cancer.1-3
Table 1: Symptoms of Cancer and Cancer Therapy1-3
| Symptom Type With Examples | Acute | Chronic | Late |
| Physical: Bone loss and metastases, changes in body composition (metabolic syndrome, weight gain), loss of appetite, cachexia, cardiovascular disease (CVD), lymphedema, peripheral neuropathy, nausea/vomiting, diarrhea, dyspnea, constipation, hair loss, sore mouth, and sweating | Nausea, vomiting, skin rashes, peripheral neuropathy, hair loss, decline in physical function | Lymphedema, peripheral neuropathy, infertility, changes in body composition, pre-mature menopause, cardio-vascular complications | Osteoporosis, osteopenia, cardiovascular complications (arrhythmias, arterial hypertension, coronary artery disease (CAD), diastolic dysfunction, heart failure, interstitial myocardial fibrosis, myocardial dysfunction, peripheral vascular disease, pulmonary hypertension, thromboembolism, stroke, and valvular disease) |
| Psycho-physical: Pain, fatigue, decreased muscle strength, inactivity, drowsiness, and insomnia (sleep disturbance) | Pain, fatigue | Fatigue | Fatigue |
| Psychological: Depression, anxiety, quality of life (QOL), and self-esteem | Anxiety, depression, changes in self-esteem and body image, decline in emotional function | Depression |
Several reviews, meta-analyses, and studies have shown that non-pharmacological interventions such as healthy diet, yoga, and exercise are positively associated with improved survival and QOL and reduction in some cancer-associated symptoms (fatigue, pain, constipation, dyspnea, and weight and sleep problems) and cardiovascular outcomes in patients with cancer.1,3-14 Therefore, oncologists should incorporate these non-pharmacological interventions into the treatment paradigm of their patients with cancer. Exercise can be prescribed right at the time of diagnosis of cancer and through the treatment and post-treatment as well. Oncologists should therefore be aware of the different exercise types, their benefits, and their timing in the patient's journey. They should, however, know that there is no evidence showing that exercise has beneficial effect on symptoms like nausea/vomiting, diarrhea, or loss of appetite.2
Also, cancer and CVD have several common risk factors such as smoking, diabetes, obesity, hypertension, and metabolic syndrome.15 Additionally, anti-cancer anthracycline-based chemotherapies, monoclonal antibodies such as trastuzumab, and radiation therapies that oncologists regularly prescribe are known to have cardiac toxicities.16 Cardiologists form an integral part of the cardio-oncology team to preempt, diagnose, and treat cardiovascular side effects of oncologic treatments.17 Cardiologists are well-versed with cardiac rehabilitation non-pharmacological intervention models such as prescribed exercise, education, counseling, and lifestyle modifications. They can work with oncologists to incorporate these models in the cancer setting as well.8 Oncologists should collaborate with cardiologists, physiotherapists, dieticians, psychologists, and others to form a multidisciplinary team that looks at the exercise and diet aspects of patients with cancer. The physiotherapist in the cardio-oncology team should also be able to recognize when the prescribed exercise starts exhausting their patient and to change its type and intensity without majorly affecting its benefits, where possible. This review is an attempt to educate the cardio-oncology team about the types of exercises that can be prescribed to patients with cancer, when the exercises can be prescribed, exercise intensity, and the benefits provided by these exercises in alleviating the side effects of cancer and its treatment and in improving the cardiovascular fitness of the patients with cancer and survivors of cancer.
Benefits of Exercise in Patients With Cancer
Exercise helps in alleviating cancer-related adverse effects, has a beneficial effect on the whole body and cardiovascular health, and seems to slows cancer progression through probably direct action on tumor-intrinsic factors and by possibly improving the efficacy of the anti-cancer treatment.18 Additionally, a review of 100 studies showed that patients who exercise post cancer diagnosis had fewer cancer-related adverse effects and a lower risk of cancer recurrence and mortality compared with patients who either did not exercise or exercised minimally.19 Segal et al. reviewed 2 guidelines, 18 systematic reviews, and 29 randomized controlled trials studying the effect of exercise during active cancer treatment and after it to conclude that exercise is safe in patients with cancer and provides muscular and aerobic fitness and improves QOL.20
Clinicians should be aware that exercise has added benefit in reducing cardiovascular risk in patients with cancer who exercise regularly versus those who do not exercise if other cardiovascular health metrics (like body mass index, blood pressure, total cholesterol, and fasting blood glucose) are under control (Table 2).8,21
Table 2: Clinical and Cardiovascular Benefits of Exercise in Patients With Cancer in Neo-Adjuvant and Adjuvant Setting8
| Setting and Cancer Type | Beneficial Outcomes of Exercise |
| Adjuvant Setting | |
| Breast | Decreased CVD events and CAD mortality; cardio-respiratory fitness may remain the same, improve, or decrease depending on patient's condition and breast cancer stage; decreased left ventricular ejection fraction |
| Prostate and Colorectal Cancer | Improves cardio-respiratory fitness |
| Post-Adjuvant Setting | |
| Breast | Decreased CVD events and all-cause mortality; cardio-respiratory fitness may improve or remain the same; vascular function improves |
| Prostate | Vascular function and cardio-respiratory fitness improves |
| Adult Survivors of Childhood Cancers | Decreased CVD events and all-cause mortality |
| Testicular | Vascular function and cardio-respiratory fitness improves; improved Framingham risk score |
| Colorectal Cancer | Decrease in all-cause mortality; cardio-respiratory fitness may remain the same, improve, or decrease |
| Leukemia and Lymphoma | Improved cardio-respiratory fitness |
Exercise Prescription in Patients With Cancer By Type of Exercise
Clinicians should understand that exercise and physical activity are two distinct entities. Physical activity is any movement by the musculoskeletal system resulting in energy expenditure. Exercise is a planned, structured, and repetitive physical activity that has a purpose and calculated and planned energy expenditure. Exercise can be prescribed during the pre-habilitation phase (time period between cancer diagnosis and initiation of its treatment), habilitation (during treatment), and rehabilitation phase (after therapy in survivors).
How to Decide Which Exercise Will Benefit the Patient
There are various types of exercises (aerobic, resistance, strength, weight and impact, balance, and flexibility and relaxation) that can be prescribed in various combinations depending on the symptoms.
The cardio-oncology team can decide which exercise type will benefit the concerned patient with cancer depending on the patient's physical, psycho-physical, and psychological symptoms (Table 3).1,3 Restorative exercise along with yoga helps significantly improve fatigue, pain, dyspnea, insomnia, constipation, risk for lymphedema, feeling of overall wellbeing, and cognitive and social functioning (p < 0.05).3,14
Table 3: Types of Exercises and Their Effect on Cancer Symptoms and Adverse Effects of Cancer Therapy1
| Aerobic Exercise | Resistance Exercise | Strength Exercise | Weight and Impact Exercise | Balance Exercise | Flexibility and Relaxation Exercise | |
| Physical Aspects | ||||||
| Bone Loss and Disease | X | X | ||||
| Muscle and Fat Mass Imbalance | X | X | ||||
| Cachexia | X | X | ||||
| Peripheral Neuropathy | X | X | ||||
| Lymphedema | X | |||||
| Psycho-Physical Aspects | ||||||
| Pain | X | |||||
| Fatigue | X | X | X | X | ||
| Sleep Disorders | X | X | ||||
| Psychological Aspects | ||||||
| Depression, Anxiety | X | |||||
| QOL | X | X | X | X | ||
| Self-Esteem | X | |||||
How to Write an Exercise Prescription and Assess Intensity of Exercise
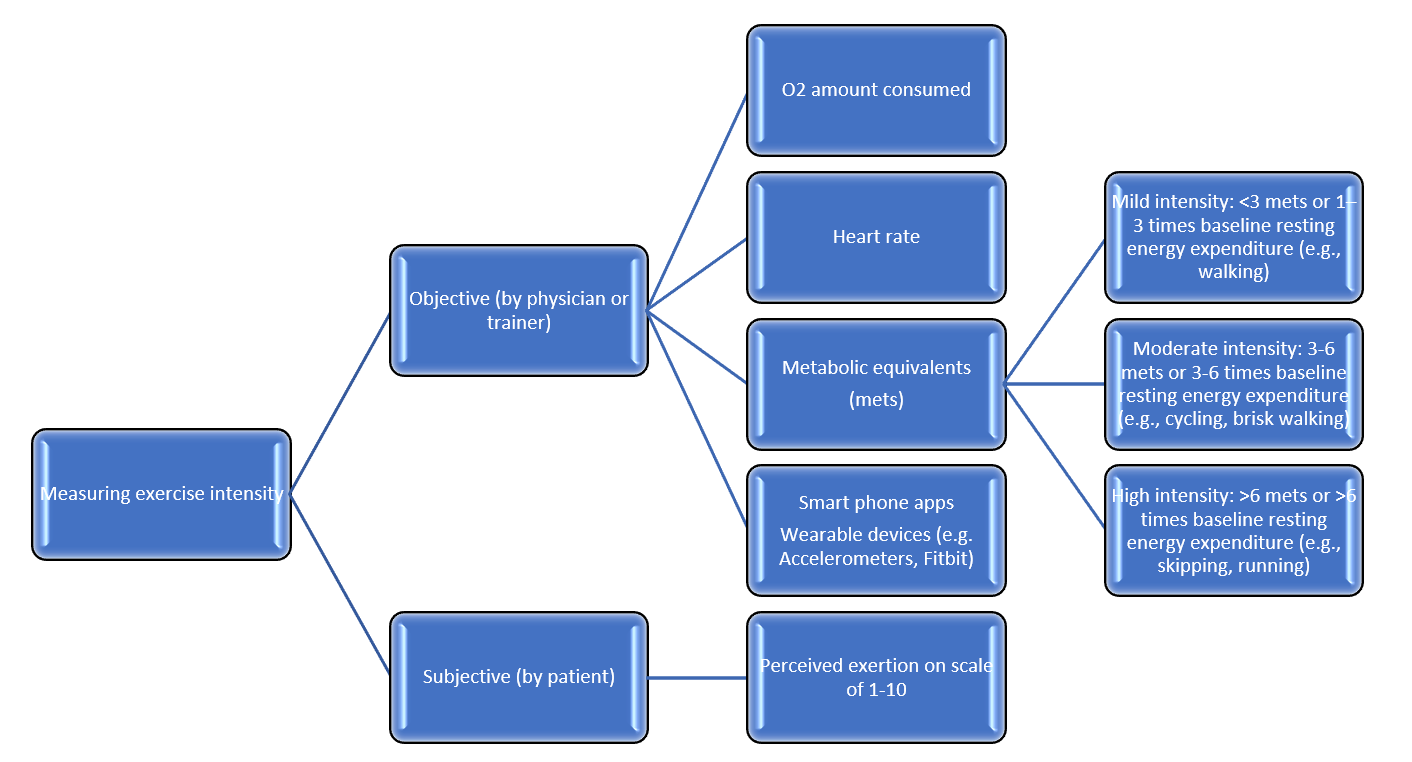
Each exercise prescription should follow the FITT principle and clearly state frequency (the number of times the exercise will be performed per week), intensity, time or duration, and type of exercise.22,23 Intensity of exercise can be measured subjectively by the patient and objectively by the physician or trainer (Figure 1).22,24-26 At each stage, patients should be monitored carefully and the exercise regimen modified based on the patient's physical condition, endurance, and fatigue level along with cardiovascular fitness and presence of cardiovascular risk factors.8,21,23
Figure 1: Measuring Exercise Intensity22,24-26
Exercise Prescription in Patients With Cancer By Exercise Intensity
Usually, patients with cancer can safely perform moderate intensity exercise during and after treatment, and this helps improve their aerobic and muscular fitness and QOL.22 Simple exercises like walking 3-4 days a week can improve functional ability of patients with cancer.3 Compared with high-intensity exercises, moderate-intensity exercise can be sustained over a longer period of time and provide the required protective benefits, including cardiovascular protection.3,8,21,22
Several American and Canadian societies recommend 150 minutes of moderate intensity exercise over 3-5 days and at least 2 days devoted to resistance exercise every week. Each exercise session should include a warm-up and a cool-down. The resistance exercise session should involve 2 sets of 8-10 major muscle groups repeated 8-10 times.3,22 Flexibility exercises should also include all major muscle groups, and balance exercise should be included for all elderly patients and for those who have balance issues.3
Exercising in a Supervised Setting
Patients with cancer who are severely debilitated and have other comorbidities or cardiovascular risk factors or have experienced or are at risk of experiencing cardiovascular side effects due to cancer therapy should initially be exercised in a supervised setting by a trained physical therapist. Community-based programs will benefit cancer survivors with least debility.21,27 Exercise programs in a supervised or group setting have multiple benefits and are found to be superior in improving QOL, fatigue, and muscular strength than an individual exercising alone. These programs provide the right motivation, exercise technique, and a safe environment to exercise.20,28
Pre-Exercise Assessment for Patients With Cancer
The next important thing for the cardio-oncology team is to assess the patient's condition to chalk out an exercise regimen that would be beneficial for the patient. The pre-exercise assessment should include the patient's general condition and special considerations (e.g., lymphedema, peripheral neuropathy, cardiovascular risk, musculoskeletal morbidities, cardiac issues, and special situations such as central lines, ostomies, or breast reconstruction) (Table 4).3,8,22
Table 4: Pre-Exercise Assessment of Patients With Cancer8
| Normal Testing |
| Cardiopulmonary Exercise Testing (CPET) |
| Resting blood pressure (BP) ≤160/90 mmHg (If elevated, recheck after 5 minutes. If still elevated, then reschedule CPET after patient is seen by provider to adjust BP medications.) |
| Normal BP response to exercise |
| No inducible ischemia |
| No atrial or ventricular arrhythmias |
| Maintain normal O2 saturations |
| No symptoms (Symptoms such as dyspnea, chest pain, or dizziness or other cardiac symptoms during exercise deemed abnormal by supervising physician.) |
| 6-Minute Walk Test |
| Resting BP ≤160/90 mmHg (If elevated, recheck after 5 minutes. If still elevated, then reschedule CPET after patient is seen by provider to adjust BP medications.) |
| Maintain normal O2 saturations |
| Laboratory Studies |
| Absence of severe anemia (<8.0 g/dL) |
| Absolute neutrophil count >500 mm3 |
| Platelet count >50 000/mcL |
| No Baseline Symptoms |
| Acute nausea during exercise |
| Vomiting within 24 hours |
| Disorientation |
| Blurred vision |
| Ongoing Cancer Complications |
| Acute infection |
| Acute metabolic disease (Examples include abnormal thyroid function, uncontrolled diabetes mellitus, and electrolyte abnormalities.) |
| New-onset lymphedema |
| Mental or physical impairment to exercise |
| Initial wound healing after surgery |
| Bone or brain metastasis (For patients with bone or brain metastases, a plan needs to include a consultation with oncology rehabilitation to establish a patient-specific safe exercise plan.) |
| Displays Exercise Knowledge |
| Understands functions of aerobic and resistance equipment |
| Demonstrates correct form on equipment |
| Understands perceived exertion and heart rate goals; performs exercise accordingly |
Barriers to Exercise During Cancer Therapy and Predictors of Adherence
Clinicians should be aware of the challenges and barriers that prevent patients with cancer from adhering to their exercise programs. Exercising can be a challenge in patients with cancer because physical activity decreases during course of disease, resulting in de-conditioning or reduced exercise capacity. Additionally, cancer cells release substances such as circulating cytokines, proteolysis-inducing factor, and lipid-mobilizing factor that impair energy metabolism. Cancer and its treatment can cause anorexia, nausea, vomiting, dehydration, systemic inflammation, oxidative stress, mitochondrial death, and skeletal muscle atrophy, all of which reduce the exercise capacity. Cardiovascular complications of cancer treatment also make exercising difficult.21,29
Apart from this, several oncology care settings lack proper exercise screening, implementation, and referral programs. Oncologists and patients both lack proper guidance and knowledge about exercising, and the multidisciplinary team often does not have a trained physical therapist to guide the exercise sessions.30 Similarly, the multitude of surgical procedures, treatment options and their side effects, types of cancer, and variance in metastatic spread makes it impossible to develop a single exercise protocol/regimen that can be universally followed.23
Positive exercise history, high motivation level, fewer exercise limitations, and availability of an exercise center close to home are independent predictors of adherence to exercise during cancer treatment. In cancer survivors, adherence to exercise during cancer treatment, high motivation levels, decreased alcohol consumption, availability of physical trainers and training centers, less extensive surgery, family support, and the right patient education predict higher adherence to exercise.31
Strategies to Make Exercise a More Accessible Therapy
A single-center program offering exercise counseling consultation along with cardio-oncology care is beneficial in improving self-reported QOL and physical and psychosocial symptoms in patients with cancer.28 The benefits multiply with each exercise counseling session, stressing the need to integrate exercise counseling into the treatment paradigm of patients with cancer.28
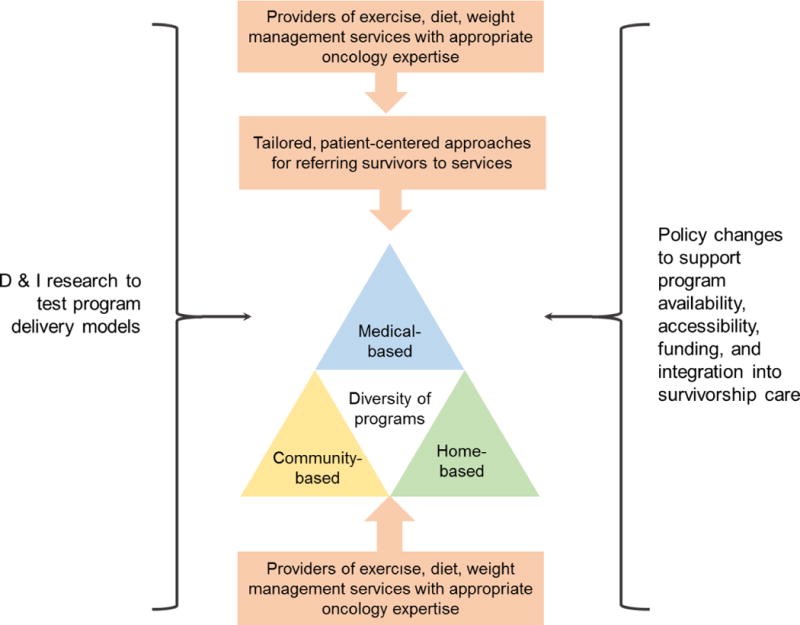
Strategies to improve exercise adherence would need to be constantly researched and various care models developed and tested to see what model works best. Easy access to diverse community-, center-, or home-based exercise programs is required. These programs should be either low cost or fully reimbursed by insurance (Figure 2). To make this possible, there is a need to spread awareness about these programs and their benefits and necessity among patients, oncologists, and policy makers.32
Figure 2: Action Steps to Increase the Availability and Uptake of Multimodal Interventions Including Exercise for Patients With Cancer and Survivors32
Conclusion
This review highlights the importance of exercise as a safe and effective strategy to improve physical, muscular, and cardiovascular fitness in adult patients with cancer and improve their QOL. Multimodal regimens incorporating exercise with nutrition and psychological support need to be tested to find a model that can be universally applied with scope for suitable alterations. Exercise does seem to have some cognitive benefit, and this should continue to be studied in detail. There is still not much clarity on the timing, type, intensity, and frequency of exercise that gives maximum cognitive benefit.33,34 Further research in this area will empower the cardio-oncology team to better adjust exercise in their oncology prescriptions, improve their cardio-respiratory fitness, and reduce associated cardiovascular risk.
References
- Ferioli M, Zauli G, Martelli AM, et al. Impact of physical exercise in cancer survivors during and after antineoplastic treatments. Oncotarget 2018;9:14005-34.
- Nakano J, Hashizume K, Fukushima T, et al. Effects of Aerobic and Resistance Exercises on Physical Symptoms in Cancer Patients: A Meta-analysis. Integr Cancer Ther 2018;17:1048-58.
- Schwartz A, de Heer HD, Bea JW. Initiating Exercise Interventions to Promote Wellness in Cancer Patients and Survivors. Oncology (Williston Park) 2017;31:711-7.
- Bourke L, Boorjian SA, Briganti A, et al. Survivorship and improving quality of life in men with prostate cancer. Eur Urol 2015;68:374-83.
- Chiu HY, Huang HC, Chen PY, Hou WH, Tsai PS. Walking improves sleep in individuals with cancer: a meta-analysis of randomized, controlled trials. Oncol Nurs Forum 2015;42:E54-62.
- Duncan M, Moschopoulou E, Herrington E, et al. Review of systematic reviews of non-pharmacological interventions to improve quality of life in cancer survivors. BMJ Open 2017;7:e015860.
- Gerritsen JK, Vincent AJ. Exercise improves quality of life in patients with cancer: a systematic review and meta-analysis of randomised controlled trials. Br J Sports Med 2016;50:796-803.
- Gilchrist SC, Barac A, Ades PA, et al. Cardio-Oncology Rehabilitation to Manage Cardiovascular Outcomes in Cancer Patients and Survivors: A Scientific Statement From the American Heart Association. Circulation 2019;139:e997-e1012.
- Ligibel JA, Basen-Engquist K, Bea JW. Weight Management and Physical Activity for Breast Cancer Prevention and Control. Am Soc Clin Oncol Educ Book 2019;39:e22-e33.
- Oruç Z, Kaplan MA. Effect of exercise on colorectal cancer prevention and treatment. World J Gastrointest Oncol 2019;11:348-66.
- Paulo TRS, Rossi FE, Viezel J, et al. The impact of an exercise program on quality of life in older breast cancer survivors undergoing aromatase inhibitor therapy: a randomized controlled trial. Health Qual Life Outcomes 2019;17:17.
- Smits A, Lopes A, Das N, Bekkers R, Massuger L, Galaal K. The effect of lifestyle interventions on the quality of life of gynaecological cancer survivors: A systematic review and meta-analysis. Gynecol Oncol 2015;139:546-52.
- Stacey FG, James EL, Chapman K, Courneya KS, Lubans DR. A systematic review and meta-analysis of social cognitive theory-based physical activity and/or nutrition behavior change interventions for cancer survivors. J Cancer Surviv 2015;9:305-38.
- Vardar Yağlı N, Şener G, Arıkan H, et al. Do yoga and aerobic exercise training have impact on functional capacity, fatigue, peripheral muscle strength, and quality of life in breast cancer survivors? Integr Cancer Ther 2015;14:125-32.
- Koene RJ, Prizment AE, Blaes A, Konety SH. Shared Risk Factors in Cardiovascular Disease and Cancer. Circulation 2016;133:1104-14.
- Lenneman CG, Sawyer DB. Cardio-Oncology: An Update on Cardiotoxicity of Cancer-Related Treatment. Circ Res 2016;118:1008-20.
- Barros-Gomes S, Herrmann J, Mulvagh SL, Lerman A, Lin G, Villarraga HR. Rationale for setting up a cardio-oncology unit: our experience at Mayo Clinic. Cardiooncology 2016;2:5.
- Hojman P, Gehl J, Christensen JF, Pedersen BK. Molecular Mechanisms Linking Exercise to Cancer Prevention and Treatment. Cell Metab 2018;27:10-21.
- Cormie P, Zopf EM, Zhang X, Schmitz KH. The Impact of Exercise on Cancer Mortality, Recurrence, and Treatment-Related Adverse Effects. Epidemiol Rev 2017;39:71-92.
- Segal R, Zwaal C, Green E, et al. Exercise for people with cancer: a systematic review. Curr Oncol 2017;24:e290-e315.
- Squires RW, Shultz AM, Herrmann J. Exercise Training and Cardiovascular Health in Cancer Patients. Curr Oncol Rep 2018;20:27.
- Segal R, Zwaal C, Green E, et al. Exercise for people with cancer: a clinical practice guideline. Curr Oncol 2017;24:40-6.
- Scheede-Bergdahl C, Minnella EM, Carli F. Multi-modal prehabilitation: addressing the why, when, what, how, who and where next? Anaesthesia 2019;74:20-6.
- Douma JAJ, Verheul HMW, Buffart LM. Feasibility, validity and reliability of objective smartphone measurements of physical activity and fitness in patients with cancer. BMC Cancer 2018;18:1052.
- Melisko ME, Hadeler EK, Nelson SH, et al. Objective assessment of physical activity during chemotherapy for breast cancer. J Clin Oncol 2017;35:TPS6626.
- Schrack JA, Gresham G, Wanigatunga AA. Understanding physical activity in cancer patients and survivors: new methodology, new challenges, and new opportunities. Cold Spring Harb Mol Case Stud 2017;3:a001933.
- Heston AH, Schwartz AL, Justice-Gardiner H, Hohman KH. Addressing physical activity needs of survivors by developing a community-based exercise program: LIVESTRONG® at the YMCA. Clin J Oncol Nurs 2015;19:213-7.
- Lopez G, Eddy C, Liu W, et al. Physical Therapist-Led Exercise Assessment and Counseling in Integrative Cancer Care: Effects on Patient Self-reported Symptoms and Quality of Life. Integr Cancer Ther 2019;18: 1534735419832360.
- Loughney L, Grocott MP. Exercise and Nutrition Prehabilitation for the Evaluation of Risk and Therapeutic Potential in Cancer Patients: A Review. Int Anesthesiol Clin 2016;54:e47-e61.
- Lyons KD, Padgett LS, Marshall TF, et al. Follow the trail: Using insights from the growth of palliative care to propose a roadmap for cancer rehabilitation. CA Cancer J Clin 2019;69:113-26.
- Ormel HL, van der Schoot GGF, Sluiter WJ, Jalving M, Gietema JA, Walenkamp AME. Predictors of adherence to exercise interventions during and after cancer treatment: A systematic review. Psychooncology 2018;27:713-24.
- Basen-Engquist K, Alfano CM, Maitin-Shepard M, et al. Agenda for Translating Physical Activity, Nutrition, and Weight Management Interventions for Cancer Survivors into Clinical and Community Practice. Obesity (Silver Spring) 2017;25:S9-S22.
- Myers JS, Erickson KI, Sereika SM, Bender CM. Exercise as an Intervention to Mitigate Decreased Cognitive Function From Cancer and Cancer Treatment: An Integrative Review. Cancer Nurs 2018;41:327-43.
- Witlox L, Schagen SB, de Ruiter MB, et al. Effect of physical exercise on cognitive function and brain measures after chemotherapy in patients with breast cancer (PAM study): protocol of a randomised controlled trial. BMJ Open 2019;9:e028117.
Clinical Topics: Arrhythmias and Clinical EP, Cardio-Oncology, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, Pulmonary Hypertension and Venous Thromboembolism, Sports and Exercise Cardiology, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Lipid Metabolism, Nonstatins, Novel Agents, Acute Heart Failure, Pulmonary Hypertension, Diet, Exercise, Hypertension, Smoking, Stress, Sleep Apnea, Sports and Exercise and ECG and Stress Testing
Keywords: Cardiotoxicity, Cardiotoxins, Alopecia, Anorexia, Anthracyclines, Arrhythmias, Cardiac, Atrophy, Anxiety, Appetite, Blood Glucose, Blood Pressure, Body Composition, Body Image, Body Mass Index, Bone Diseases, Metabolic, Breast Neoplasms, Brain Neoplasms, Calcium Carbonate, Cachexia, Cardiac Rehabilitation, Cardiovascular Diseases, Cholesterol, Cognition, Chest Pain, Colorectal Neoplasms, Comorbidity, Constipation, Coronary Artery Disease, Counseling, Cytokines, Diabetes Mellitus, Depression, Dehydration, Dizziness, Diarrhea, Early Detection of Cancer, Dyspnea, Electrolytes, Energy Metabolism, Exercise Test, Exercise, Exercise Therapy, Fasting, Hypertension, Hypertension, Pulmonary, Heart Failure, Infertility, Inflammation, Intrinsic Factor, Leukemia, Lymphedema, Lymphoma, Mammaplasty, Menopause, Metabolic Syndrome, Midazolam, Muscle Strength, Muscle, Skeletal, Motivation, Musculoskeletal System, Nausea, Neoadjuvant Therapy, Nutritionists, Obesity, Osteoporosis, Ostomy, Oxidative Stress, Pain, Patient Care Team, Patient Safety, Peripheral Nervous System Diseases, Peptides, Peripheral Vascular Diseases, Physical Endurance, Physical Therapists, Prostate, Proteolysis, Referral and Consultation, Risk Factors, Quality of Life, Self Report, Sleep Initiation and Maintenance Disorders, Sleep Stages, Smoking, Stroke, Stroke Volume, Survival Rate, Sweating, Thromboembolism, Thyroid Gland, Vomiting, Weight Gain
< Back to Listings