Radiation Safety in the Practice of Cardiology With an Emphasis on Special Considerations in Women
Quick Takes
- Exposure to radiation has been a notable deterrent for women pursing the field of cardiology as a career.
- With standard radiation safety measures practiced routinely, there is no statistically significant or convincing evidence of an increased risk of pregnancy-related complications for female cardiologists exposed to radiation.
- Radiation safety is a learned skillset that is imperative for the health and safety of all cardiologists; proper training, protective equipment, and effective policies are essential tools for the modern workforce.
Radiation exposure is a known reason why women do not pursue cardiology as a specialty, with surveys consistently citing radiation exposure as a common concern that dissuades women from entering this field. Despite this, training on radiation safety and awareness of safety policies and procedures are globally inconsistent. According to a 2015 work-life survey of female cardiologists conducted by the Women in Cardiology section of the American College of Cardiology, only 34% of women cardiologists in the United States reported that their department had an official policy on radiation exposure during pregnancy, 34% were unaware of a policy, and 32% reported that their departments had no official policy.1 Other studies have consistently shown a similar lack of knowledge or standardization in the practice of radiation safety and lack of routine implementation of radiation protective strategies. For women cardiologists, the added consideration of pregnancy makes knowledge regarding the risks of radiation exposure as well as safety practices an essential aspect of professional career planning. Thus, it is important that all cardiologists receive comprehensive radiation education including pregnancy-related radiation issues during fellowship, at the time of new employment, and during fluoroscopy credentialing and re-credentialing.2
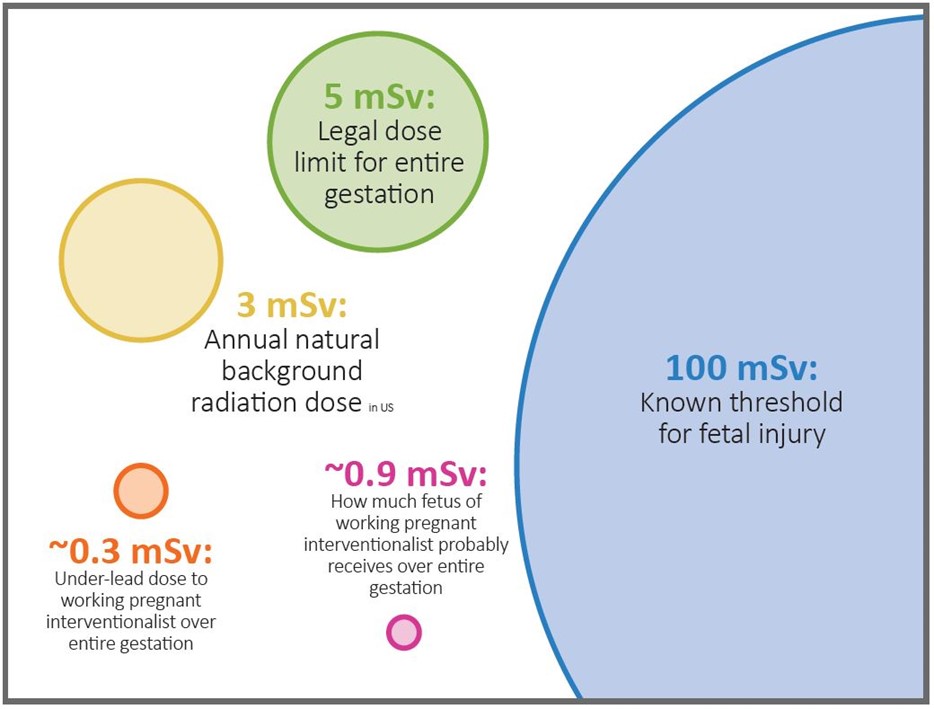
Given frequent and often significant deficits in cardiologists' knowledge of radiation exposure and risk, it is critical for health care workers to understand radiation dosing limitations, particularly related to pregnancy. In the United States, the Nuclear Regulatory Commission sets a regulatory dosing limit of 5 mSv during the entire pregnancy. Internationally, the International Commission on Radiological Protection and European Commission have a limit of 1 mSv during the duration of pregnancy.3 With these limits in mind, it is important to note that there is no evidence that radiation dose to the fetus <100 mSv during pregnancy is associated with an increased incidence of congenital malformation, stillbirth, miscarriage, growth malformation, or mental disability, and there is no statistically significant or convincing evidence of an increased risk of cancer in offspring of female radiation workers (Figure 1).4 The focus for all health care workers exposed to radiation should be on managing occupational exposure, which should include understanding basic radiation physics, understanding correct use of lead garments and protective wear, and understanding positional orientation of oneself and equipment.
Figure 1: Dose Limits
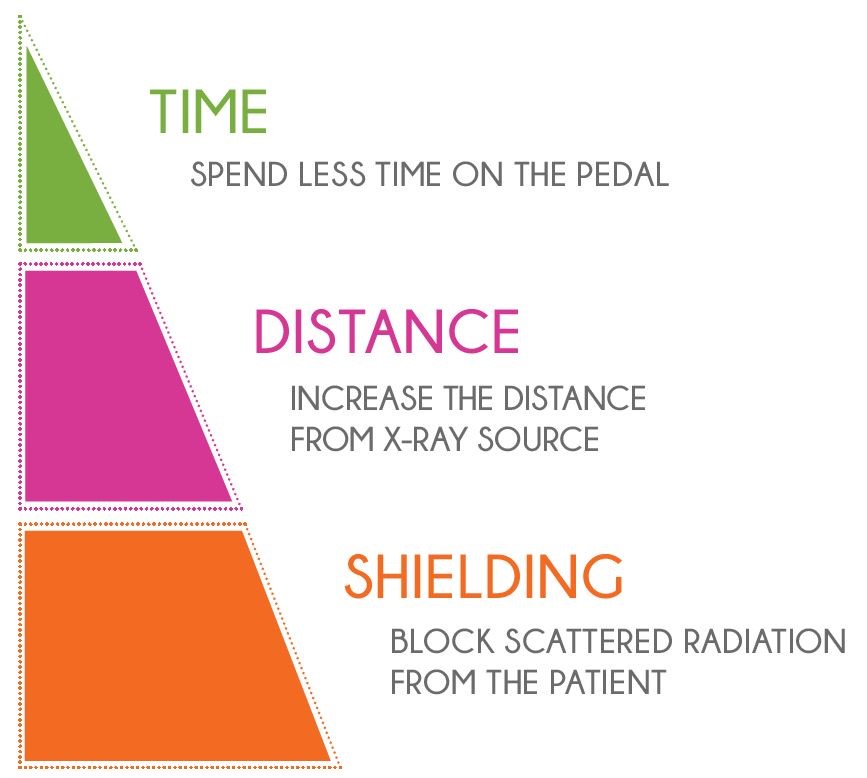
When it comes to managing radiation exposure, it is important to understand and achieve dosage as low as reasonably achievable for radiation exposure while achieving needed imaging. To help achieve dosage as low as reasonably achievable, there are three fundamentals that are key to radiation safety: time, distance, and shielding. Specifically, these principles refer to spending less time on the pedal, increasing distance from the X-ray source, and shielding to block scattered radiation reflected from the patient (Figure 1).5 Making a commitment to these concepts is critical to minimizing radiation exposure.
Figure 2: Three Fundamentals of Radiation Safety
Reducing radiation exposure also requires protective equipment and distancing. Wearing appropriate equipment that includes a leaded apron with shoulder pads for women (to protect radiosensitive breast tissue), leaded glasses, a lead thyroid collar, and optional leg shields. Proper use of a dosimeter radiation badge ensures proper radiation monitoring to limit exposure. Optimal table and image intensifier positions play an important role in reducing radiation exposure. There is an optimal position marked by the distance between the patient's skin surface and the X-ray source. This position is optimal when it is about 70 cm above the source.
Maintaining distance from the image intensifier by increasing the working distance from 40 cm to 80 cm can decrease scattered radiation around one fourth of the original dose. Additionally, when manipulating the C-arm, avoid steep angulations and vary the C-arm angles to avoid repetitive exposure.3 Regarding image acquisitions, choose views that minimize radiation exposure. Anterior-posterior views and right anterior oblique views should be preferred to the left anterior oblique views to reduce radiation dose. Additionally, collimation is an important step in image acquisition that reduces the volume irradiated, which reduces overall patient dose and scatter radiation. Finally, one must remember to press on the fluoroscopy pedals only when viewing the imaging monitor.6
Employing these key radiation management strategies help you reach the goal of limiting radiation exposure and ensuring the safety of all health care workers, particularly pregnant workers. In order to make this critical information easier to understand and more accessible, the nonprofit organization Women as One released the interactive educational slide set "Radiation Safety in the Practice of Cardiology: What all Women Should Know."7 The first-of-its-kind global educational tool is aimed at training all members of the care team on the basics of radiation safety, with a focus on the specific implications for those members who are pregnant, while performing procedures in clinical environments that utilize radiation. Proper training, protective equipment, and effective policies are essential tools for the modern workforce.
References
- Sarma AA, Nkonde-Price C, Gulati M, et al. Cardiovascular Medicine and Society: The Pregnant Cardiologist. J Am Coll Cardiol 2017;69:92-101.
- Morishima Y, Chida K, Katahira Y, Seto H, Chiba H, Tabayashi K. Need for radiation safety education for interventional cardiology staff, especially nurses. Acta Cardiol 2016;71:151-5.
- Bhatt DL. Cardiovascular Intervention: A Companion to Braunwald's Heart Disease. United Kingdom: Elsevier Health Sciences; 2015.
- Dauer LT, Miller DL, Schueler B, et al. Occupational radiation protection of pregnant or potentially pregnant workers in IR: a joint guideline of the Society of Interventional Radiology and the Cardiovascular and Interventional Radiological Society of Europe. J Vasc Interv Radiol 2015;26:171-81.
- Hirshfeld JW Jr, Ferrari VA, Bengel FM, et al. 2018 ACC/HRS/NASCI/SCAI/SCCT Expert Consensus Document on Optimal Use of Ionizing Radiation in Cardiovascular Imaging: Best Practices for Safety and Effectiveness: A Report of the American College of Cardiology Task Force on Expert Consensus Decision Pathways. J Am Coll Cardiol 2018;71:e283-e351.
- Steffenino G, Rossetti V, Ribichini F, et al. Short communication: staff dose reduction during coronary angiography using low framing speed. Br J Radiol 1996;69:860-4.
- Women as One. Radiation Safety in the Practice of Cardiology: What all Women Should Know (WomenAsOne.org). 2020. Available at rad.womenasone.org. Accessed December 19, 2020.
Clinical Topics: Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Interventions and Imaging, Angiography, Nuclear Imaging
Keywords: Coronary Angiography, Radiation, Radiation Protection, Radiation Tolerance, Women, Physicians, Women, Pregnancy, Radiation Monitoring, X-Rays, Abortion, Spontaneous, Thyroid Gland, Occupational Exposure, Health Workforce, Employment, Fluoroscopy, Protective Devices, Reference Standards, Policy, Organizations, Nonprofit, Breast Neoplasms, Diagnostic Imaging
< Back to Listings