Exercise and Elevation
Quick Takes
- The human physiology of altitude reflects acute and chronic human acclimatization to hypobaric hypoxia.
- Athletes and active individuals with cardiovascular disease who are asymptomatic and without functional limitations at sea level do not typically require screening cardiovascular testing prior to altitude ascent.
- Pre-trip planning, adequate hydration, avoidance of rapid ascent profiles, and incremental increases in exercise workload are important for athletes and active individuals with or without cardiovascular disease to minimize the risk of high-altitude illness and adverse cardiovascular events.
"Because it's there." These famous words of George Mallory justified his attempt to climb Mount Everest, the world's tallest peak, standing 8,850m (29,028 ft) above sea level. Ultimately fatal, his legacy of pushing the boundaries of human physiology in extreme altitude environments lives on.1 The effect altitude plays on athletic endeavors is, however, not limited to extreme mountaineering. Many competitive and recreational athletes, with and without cardiovascular disease, pursue altitude to utilize aspects of high-altitude environments for sports such as alpine skiing, or simply because it is the location of their next event. An understanding of the physiology and pathophysiology of altitude exposure, within the context of both healthy active individuals and those with cardiovascular disease, is an essential skill for both the sports cardiologist and all health professionals involved in the care of active populations.
The Altitude Environment
Among the unique environmental features of the altitude environment (including thermal and psychological stress) is the fact that progressive altitude related hypoxia underlies the relevant medical physiology. The composition of air remains constant despite increases in altitude, with oxygen comprising approximately 21%. Barometric pressure, however, decreases with elevation resulting in a reduction in the partial pressure of oxygen in arterial blood (PaO2) and eventual hypoxemia. This hypobaric hypoxia creates a graded physiologic stressor with increasing elevation, one which occurs at rest and is exacerbated by the demands of exercise.2 Acclimatization is the body's normal compensatory physiologic response to the hypoxic environment. For the purposes of clinical care, the degree of altitude can be defined in terms of these physiologic changes and their limits.3 Intermediate altitude (1500-2500m) is where detectable physiological changes begin. High altitude, typically defined as an elevation above 2500m, is the point above which altitude illnesses tend to occur. The equivalent sea level FiO2 at 2500m is approximately 14%.2 Extreme altitude, defined as >5800m, has a sea level equivalent FIO2 <10% and is associated with marked hypoxemia. Despite maximal efforts at acclimatization, this typically results in progressive clinical deterioration.3
Physiological Acclimatization to Altitude
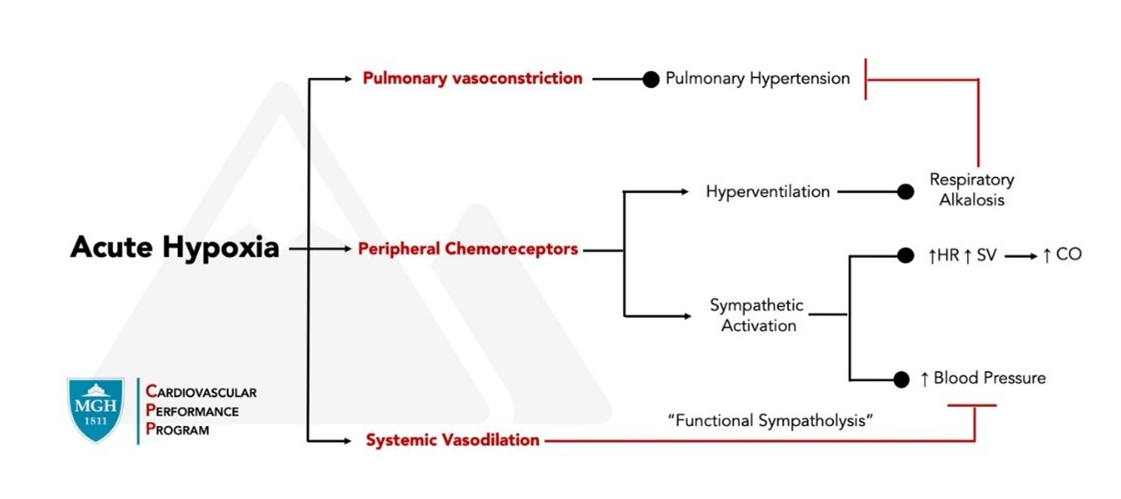
Human acclimatization to acute and chronic hypoxia serves to optimize oxygen delivery to the working muscles and tissues (Figure 1). Acute altitude exposure leads to a drop in PaO2 and the arterial oxygen content (CaO2).4 Oxygen delivery is maintained by an initial compensatory increase in cardiac output (CO) coupled with vasodilation of the systemic vasculature. The increase in CO is driven almost exclusively by an increase in heart rate, without an appreciable change in stroke volume.5 Interestingly, despite elevated sympathetic stimulation, peripheral vasodilation occurs that is driven by local metabolic factors in a phenomenon known as "functional sympatholysis".6
Figure 1
Altitudes approaching and exceeding high altitude (above 2200-2500m) result in a PaO2 less than 65mmHg and trigger physiologic responses to enhance oxygen carrying capacity.7 Acute hypoxia stimulates hyperventilation with an initial respiratory alkalosis and a subsequent increase in red blood cell mass.8 Reductions in plasma volume from increased urinary output, water loss from hyperventilation, and hypoxia-induced adipsia all serve to increase hemoglobin concentration and thereby enhance oxygen carrying capacity.9
As oxygen carrying capacity increases from prolonged hypoxic exposure, the work of the cardiovascular system subsides, with reductions in heart rate, muscle blood flow, and reduced oxygen extraction. Cardiac work, however, remains elevated above sea level values, as evidenced by persistent elevations in resting and submaximal exercise heart rates (HR).10 An increase in myocardial blood flow due to relative coronary vasodilation at both rest and exercise is observed in healthy individuals.11 Peak HR is reduced with prolonged exposure. Vascular tone as measured by systemic vascular resistance and mean arterial pressure both rise with prolonged hypoxic exposure after the initial vasodilatory effect of acute hypoxia. Pulmonary vascular resistance and pulmonary arterial pressure also increase due to hypoxic pulmonary vasoconstriction.10
Exercise Performance at Altitude
A near universal experience among all who sojourn to high altitude is a decline in exercise and functional capacity. Altitude's effect on exercise performance depends on the degree of altitude, duration of hypoxic exposure, and the type and intensity of exercise. Shorter duration anaerobic exercise may experience a beneficial performance effect as the favorable effects of reduced wind resistance outweigh the detrimental effects of reduced cardiovascular performance.12 Longer duration endurance activities, however, rely on a well-conditioned cardiovascular system. Hypoxic stress increases workload and reduces performance. The effect on aerobic performance is a function of both event duration and elevation. Performance decrements start at 1600m for events 2-5 minutes in duration but occur at elevations as low as 700m for events lasting 20 minutes or longer.13 This performance decrement is directly related to reductions in maximal oxygen consumption (V̇O2max). Maximal oxygen consumption (V̇O2max) is reduced in smaller increments starting at 580m followed by an approximate 1% reduction for every 100m above 1500m.13 Acclimatization alone does not result in appreciable increases in V̇O2max, particularly at higher altitudes. Submaximal exercise occurring at a given absolute workload is therefore performed at a higher percentage of V̇O2max. Accordingly, the lactate threshold, the physiologic parameter that determines the intensity of sustainable exercise, occurs at heart rates comparable to sea level but at lower intensities of external work.14 Submaximal exercise capacity, in contrast to maximal exercise capacity, does tend to improve with sustained hypoxia exposure owing to improvements over time in oxygen carrying capacity and CaO2.15
Athletes and High-Altitude Illness
Exposure to the hypoxic altitude environment may result in three main illnesses. These are acute mountain sickness (AMS), high altitude cerebral edema (HACE), and high-altitude pulmonary edema (HAPE).16 AMS is the least severe form and occurs in approximately 10-25% of unacclimatized persons at altitudes >2500m. The risk of HACE or HAPE typically occurs at elevations >3000m. Important to the care of athletes is that a high level of aerobic fitness is not protective against development. Furthermore, exercise can exacerbate symptoms of AMS and any degree of high-altitude illness will almost certainly affect athletic performance.10,16 Athletes travelling to high altitude should be made aware of this risk and educated regarding potential signs and symptoms of illness development. The hallmark symptom of AMS is headache, other symptoms include nausea, vomiting, dizziness, fatigue and insomnia. The development of severe symptoms, coupled with an altered level of consciousness or other neurological signs, suggest the development of HACE. HAPE, a form of non-cardiogenic pulmonary edema, may present as inappropriate dyspnea, with pink frothy sputum, or a worse than expected degree of hypoxemia for a given altitude.16 Prevention by gradual exposure to high altitude (>2500m) prior to undertaking athletic endeavors is recommended. Ideally, this should occur in the form of an ascent of no more than 300-500m per day with rest days every 3-4 days. As this is not always practical, arrival at altitude several days prior to planned exercise may help to reduce AMS symptoms.10 Ensuring adequate hydration is paramount as hypovolemia secondary to hypoxia-mediated diuresis may aggravate AMS symptoms and negatively influence performance. Several medications have demonstrated efficacy in prevention of AMS onset and reduction in symptom severity. These include acetylsalicylic acid, ibuprofen, acetazolamide, and dexamethasone.16 The latter two are banned substances and their use is therefore limited to non-competitive athletes.17 In those with a history of HAPE recurrence, risk can be reduced by prophylaxis with nifedipine, tadalafil (phosphodiesterase-5 inhibitor), or dexamethasone. The mainstay of treatment for more severe illness remains rapid descent from altitude and supplemental oxygen.16
Athletes with Cardiovascular Disease
Despite the stress imposed on the cardiovascular system from high altitude exposure, the attributable risk of adverse cardiovascular events remains unclear.2 In those with atherosclerotic coronary artery disease (CAD), it is principally sympathetically driven altitude related increases in myocardial oxygen demand coupled with the propensity for paradoxical coronary vasoconstriction that invite the potential for ischemia at altitude.2,18 After trauma, sudden cardiac death (SCD) is the predominant cause of death at altitude and observational data suggest that the risk factors for SCD track with the epidemiology of CAD—namely, age, sex, and prior history of myocardial infarction.19 Hypovolemia and early vigorous exertion appear to be risk enhancing features with most events occurring on the first day of exposure.20 Nevertheless, the limited available data indicate that high-altitude travel is generally well tolerated by individuals with stable CAD. However, in order to minimize risk, exercise at altitude merits a careful and individualized assessment prior to ascent.
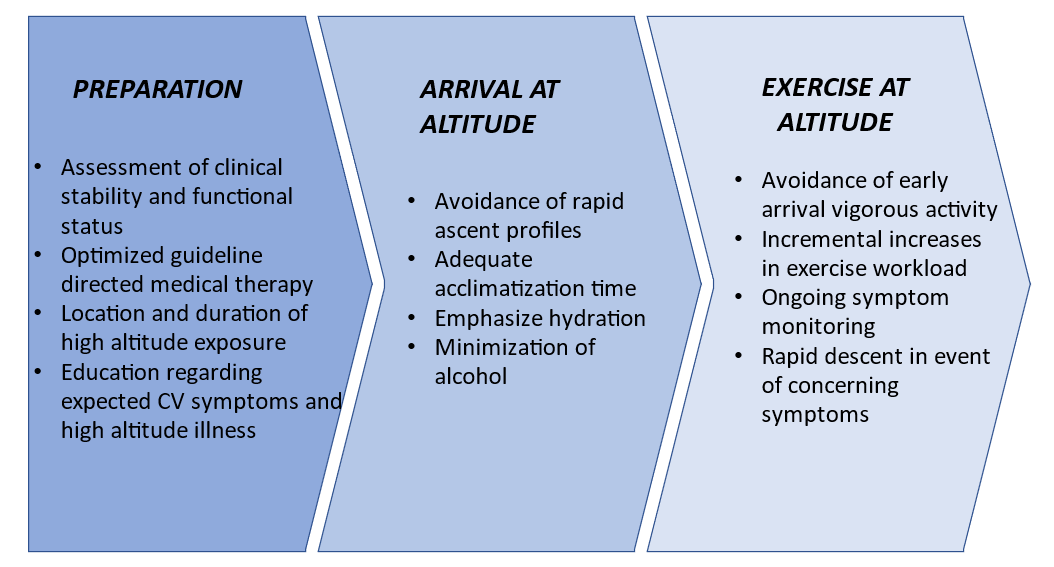
Limited data exist to guide the management of patients with established CAD during and prior to high-altitude travel and thus practice recommendations rely on expert experience and an understanding of relevant physiology. In those with stable ischemic heart disease, therapeutic hallmarks include counseling hydration, avoidance of rapid ascent profiles, and incremental increases in exercise workload to critically allow for risk reducing acclimatization (Figure 2). Guideline directed use of CAD medications should be emphasized and driven by sea level indications. Those with angina should be counseled to expect angina to occur earlier and at lower workloads. Moreover, those with CAD who are older, have had a prior myocardial infarction, have low functional status or have residual ischemia may contemplate additional risk mitigation strategies. These include counseling increasingly conservative ascent profiles, the use of supplemental oxygen, and exercise restriction. Ultimately, in those at high-risk, modification of travel plans may be considered and a plan for rapid descent from altitude should be in place in the event of concerning symptoms.
Figure 2
Active individuals with cardiovascular disease who are without symptoms and without functional limitations at sea level do not typically require screening cardiovascular testing prior to altitude ascent.10 Exercise testing, particularly in the form of cardiopulmonary exercise testing (CPET), may provide valuable insight into functional status and offer information regarding a patient's cardiovascular response to exercise across the full spectrum of exercise intensity. Normobaric hypoxic exercise testing may hold promise, but data are limited on its predictive capacity to drive clinical recommendations.21 At present, very limited data exist on the safety of altitudes above 3500-4200m for stable, asymptomatic, or minimally symptomatic patients with cardiovascular disease. Contemporary guidelines advise restriction below these altitudes and exertion should be limited to light-to-moderate intensity for those with any degree of ischemic heart disease.2 Specific recommendations pertaining to high altitude exposure in athletes with cardiovascular disease are not addressed by sports cardiology guidelines.22,23 A shared-decision making process may therefore be most appropriate in areas of clinical equipoise to adequately engage athletes with cardiovascular disease to determine the appropriateness of new or continued exercise at altitude.24
Conclusion
In summary, the hypoxic altitude environment places a unique and graded physiologic stress on those wishing to exercise within it. For the sports cardiologist, understanding the processes of physiologic acclimatization and its interaction with the diseased cardiovascular system are paramount to appropriately advise athletes, highly active persons, and those with cardiovascular disease about the cardiovascular risks and performance effects associated with exercise at high altitude.
References
- Madhok R, Lemery J, Rodway GW. Because it's there… The education of George Mallory. Wilderness Environ Med 2011;22:352-4.
- Parati G, Agostoni P, Basnyat B, et al. Clinical recommendations for high altitude exposure of individuals with pre-existing cardiovascular conditions: a joint statement by the European Society of Cardiology, the Council on Hypertension of the European Society of Cardiology, the European Society of Hypertension, the International Society of Mountain Medicine, the Italian Society of Hypertension and the Italian Society of Mountain Medicine. Eur Heart J 2018;39:1546-54.
- Imray C, Booth A, Wright A, Bradwell A. Acute altitude illnesses. BMJ 2011;343:d4943.
- Higgins JP, Tuttle T, Higgins JA. Altitude and the heart: is going high safe for your cardiac patient? Am Heart J 2010;159:25-32.
- Pagé M, Sauvé C, Serri K, Pagé P, Yin Y, Schampaert E. Echocardiographic assessment of cardiac performance in response to high altitude and development of subclinical pulmonary edema in healthy climbers. Can J Cardiol 2013;29:1277-84.
- Baggish AL, Wolfel EE, Levine BD. "Cardiovascular System: Heart and Systemic Circulation". In: Swenson ER, Bartsch P, eds. High Altitude: Human Adaptation to Hypoxia. New York, Heidelberg, Dordrecht, London: Springer; 2014:103-139.
- Levine BD, Stray-Gundersen J. A practical approach to altitude training: where to live and train for optimal performance enhancement. Int J Sports Med 1992;13 Suppl 1:S209-12.
- Weil JV, Jamieson G, Brown DW, Grover RF. The red cell mass--arterial oxygen relationship in normal man. Application to patients with chronic obstructive airway disease. J Clin Invest 1968;47:1627-39.
- Honig A. Peripheral arterial chemoreceptors and reflex control of sodium and water homeostasis. Am J Physiol 1989;257:R1282-302.
- Wolfel EE. "Exercise at High Altitude" In: Thompson PD, Fernandez AB, eds. Exercise and Sports Cardiology. London, Singapore, Hackensack World Scientific Publishing Europe Ltd.; 2017:197-232.
- Wyss CA, Koepfli P, Fretz G, Seebauer M, Schirlo C, Kaufmann PA. Influence of altitude exposure on coronary flow reserve. Circulation 2003;108:1202-7.
- Péronnet F, Thibault G, Cousineau DL. A theoretical analysis of the effect of altitude on running performance. J Appl Physiol (1985) 1991;70:399-404.
- Fulco CS, Rock PB, Cymerman A. Maximal and submaximal exercise performance at altitude. Aviat Space Environ Med 1998;69:793-801.
- Erdmann J, Sun KT, Masar P, Niederhauser H. Effects of exposure to altitude on men with coronary artery disease and impaired left ventricular function. Am J Cardiol 1998;81:266-70.
- Wolfel EE, Groves BM, Brooks GA, et al. Oxygen transport during steady-state submaximal exercise in chronic hypoxia. J Appl Physiol (1985) 1991;70:1129-36.
- Bärtsch P, Swenson ER. Clinical practice: acute high-altitude illnesses. N Engl J Med 2013;368:2294-302.
- 2020 List of Prohibited Substances and Methods (World Anti-doping Agency website). 2020. Available at: https://www.wada-ama.org/en/resources/science-medicine/prohibited-list-documents. Accessed 01/15/2021.
- Arbab-Zadeh A, Levine BD, Trost JC, et al. The effect of acute hypoxemia on coronary arterial dimensions in patients with coronary artery disease. Cardiology 2009;113:149-54.
- Burtscher M, Ponchia A. The risk of cardiovascular events during leisure time activities at altitude. Prog Cardiovasc Dis 2010;52:507-11.
- Burtscher M. Risk and protective factors for sudden cardiac death during leisure activities in the mountains: an update. Heart Lung Circ 2017;26:757-62.
- Canoui-Poitrine F, Veerabudun K, Larmignat P, Letournel M, Bastuji-Garin S, Richalet JP. Risk prediction score for severe high altitude illness: a cohort study. PLoS One 2014;9:e100642.
- Maron BJ, Zipes DP, Kovacs RJ. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: preamble, principles, and general considerations: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2015;66:2343-49.
- Pelliccia A, Sharma S, Gati S, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J 2020;42:17-96.
- Baggish AL, Ackerman MJ, Putukian M, Lampert R. Shared decision making for athletes with cardiovascular disease: practical considerations. Curr Sports Med Rep 2019;18:76-81.
- Bartsch P, Gibbs JSR. Effect of altitude on the heart and the lungs. Circulation 2007;116:2191-202.
Clinical Topics: Arrhythmias and Clinical EP, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Prevention, Sports and Exercise Cardiology, Atherosclerotic Disease (CAD/PAD), SCD/Ventricular Arrhythmias, Acute Heart Failure, Exercise
Keywords: Sports, Athletes, Exercise, Altitude, Heart Rate, Arterial Pressure, Acetazolamide, Phosphodiesterase 5 Inhibitors, Nifedipine, Ibuprofen, Altitude Sickness, Mountaineering, Pulmonary Circulation, Oxygen, Hyperventilation, Partial Pressure, Pulmonary Edema, Plasma Volume, Stroke Volume, Alkalosis, Respiratory, Cardiovascular Diseases, Coronary Artery Disease, Vasoconstriction, Vasodilation, Hypovolemia, Lactic Acid, Sleep Initiation and Maintenance Disorders, Aspirin, Brain Edema, Conservation of Natural Resources, Anaerobiosis, Cause of Death, Exercise Tolerance, Physical Exertion, Oxygen Consumption, Cell Hypoxia, Athletic Performance, Acclimatization, Risk Factors, Myocardial Infarction, Dyspnea, Fatigue, Nausea, Headache, Death, Sudden, Cardiac, Ischemia, Diuresis, Erythrocytes, Dexamethasone, Hemoglobins
< Back to Listings