Practical Implications of the REALITY Trial
Introduction
Anemia is common in patients with acute myocardial infarction (AMI) and affects prognosis. Transfusion is often considered because even moderate levels of anemia are associated with increased cardiovascular mortality in these patients. In theory, transfusion should increase oxygen delivery and therefore improve outcomes. However, data suggest that oxygen delivery is not necessarily increased in patients receiving transfusions, due at least in part to red blood cell depletion in nitric oxide and 2,3-diphosphoglyceric acid during storage.1 Conversely, transfusion may have deleterious effects, including but not limited to increased platelet activation and aggregation and vasoconstriction.2 In addition, blood is a scarce resource that should be conserved.
Observational studies regarding transfusion strategies in AMI have provided inconsistent results due to confounding factors.3 Only 2 small pilot randomized trials have compared restrictive with liberal transfusion strategies in patients with AMI and have yielded contradictory results. The CRIT (Conservative Versus Liberal Red Cell Transfusion in Myocardial Infarction Trial) pilot study4 randomized 45 patients with AMI and hematocrit ≤30% to a liberal versus a conservative transfusion strategy and found benefit of a liberal strategy for the primary composite outcome of in-hospital death, recurrent myocardial infarction, and new or worsening heart failure (38% vs. 13%; p = 0.046). Death occurred in 1 patient in the liberal group and 2 patients in the restrictive group. Conversely, the MINT (Myocardial Ischemia and Transfusion Pilot) pilot study5 included 110 patients with acute coronary syndrome or stable angina and hemoglobin <10 g/dL and found a trend for fewer cardiac events in patients treated with a restrictive strategy (with a primary composite outcome of death, myocardial infarction, or unscheduled revascularization occurring in 10.9% vs. 25.5% in the liberal vs. restrictive strategy arms, respectively; p = 0.054). Death occurred in 1.8% of patients in the liberal group versus 13.0% of patients in the restrictive group (p = 0.032).
REALITY Trial Design
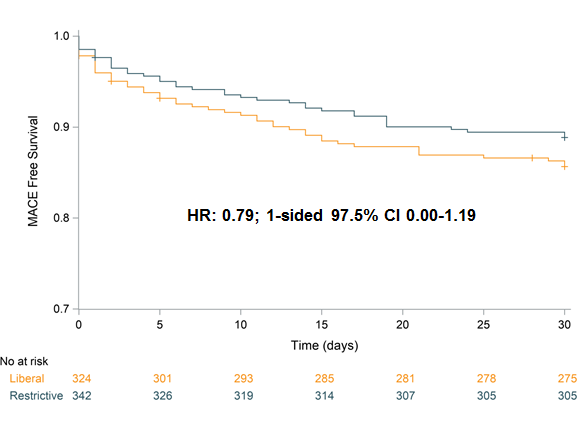
The REALITY (Restrictive and Liberal Transfusion Strategies in Patients With Acute Myocardial Infarction) multicenter randomized trial compared a restrictive (n = 342) with a liberal (n = 324) transfusion strategy (transfusion triggered by hemoglobin ≤8 and ≤10 g/dL, respectively) in patients with AMI and anemia in 35 French and Spanish centers.6 Patients randomly assigned to the restrictive strategy received 55% fewer units of blood. At 30 days, a major adverse cardiovascular event (MACE) had occurred in 36 patients (11.0%; 95% confidence interval [CI], 7.5-14.6) in the restrictive arm and in 45 patients (14.0%; 95% CI, 10.1-18.0) in the liberal arm (relative risk 0.79; upper bound of 95% 2-sided CI, 1.19), meeting the prespecified non-inferiority criterion in both per-protocol and intention-to-treat populations (Figure 1). In addition, patients treated with the restrictive strategy had lower risks of bacterial infection (0% vs. 1.5%; p = 0.03) and acute respiratory distress syndrome (0.3% vs. 2.2%; p = 0.03).7
Figure 1: MACE-Free Survival
From a cost-effectiveness standpoint, the 30-day incremental cost-effectiveness ratio was −€33,065 (i.e., more than $39,000 saved per additional MACE averted with the restrictive vs. liberal strategy). Analysis of the joint distribution of costs and outcomes found that the restrictive strategy had an 84% probability to be dominant (i.e., both cost-saving and MACE-reducing).
Practical Implications
Given uncertainty regarding the clinical effectiveness of transfusion strategies, current international guidelines are somewhat inconsistent and provide weak recommendations.8-10 The REALITY trial is, to date, the largest randomized trial on transfusion in patients with AMI and anemia and therefore constitutes the most robust data available on this topic. The trial established non-inferiority of the restrictive strategy at 30 days in terms of clinical efficacy and saving blood, with excellent safety and a high probability of being dominant from a cost-effectiveness standpoint. Pending the results of the ongoing and larger MINT trial, the results of the REALITY trial support a restrictive strategy in patients with anemia and AMI.
References
- Doyle BJ, Rihal CS, Gastineau DA, Holmes DR Jr. Bleeding, blood transfusion, and increased mortality after percutaneous coronary intervention: implications for contemporary practice. J Am Coll Cardiol 2009;53:2019-27.
- Silvain J, Abtan J, Kerneis M, et al. Impact of red blood cell transfusion on platelet aggregation and inflammatory response in anemic coronary and noncoronary patients: the TRANSFUSION-2 study (impact of transfusion of red blood cell on platelet activation and aggregation studied with flow cytometry use and light transmission aggregometry). J Am Coll Cardiol 2014;63:1289-96.
- Yeh RW, Wimmer NJ. Blood transfusion in myocardial infarction: opening old wounds for comparative-effectiveness research. J Am Coll Cardiol 2014;64:820-2.
- Cooper HA, Rao SV, Greenberg MD, et al. Conservative versus liberal red cell transfusion in acute myocardial infarction (the CRIT Randomized Pilot Study). Am J Cardiol 2011;108:1108-11.
- Carson JL, Brooks MM, Abbott JD, et al. Liberal versus restrictive transfusion thresholds for patients with symptomatic coronary artery disease. Am Heart J 2013;165:964-971.e1.
- Ducrocq G, Calvo G, González-Juanatey JR, et al. Restrictive vs liberal red blood cell transfusion strategies in patients with acute myocardial infarction and anemia: Rationale and design of the REALITY trial. Clin Cardiol 2021;44:143-50.
- Ducrocq G, González-Juanatey JR, Puymirat E, et al. Effect of a Restrictive vs Liberal Blood Transfusion Strategy on Major Cardiovascular Events Among Patients With Acute Myocardial Infarction and Anemia: The REALITY Randomized Clinical Trial. JAMA 2021;325:552-60.
- Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2016;37:267-315.
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J 2018;39:119-77.
- Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;64:e139-e228.
Clinical Topics: Acute Coronary Syndromes, Heart Failure and Cardiomyopathies, Stable Ischemic Heart Disease, Acute Heart Failure, Chronic Angina
Keywords: Nitric Oxide, Hematocrit, Angina, Stable, Acute Coronary Syndrome, Risk, Uncertainty, Confidence Intervals, Vasoconstriction, Cost-Benefit Analysis, Hospital Mortality, Pilot Projects, Cost Savings, Intention to Treat Analysis, Myocardial Infarction, Anemia, Hemoglobins, Treatment Outcome, Stroke, Prognosis, Heart Failure, Erythrocytes, Platelet Activation, Respiratory Distress Syndrome, Bacterial Infections, Oxygen, Mentha
< Back to Listings