Mitigating ASCVD Risk Among Those Previously Infected with COVID-19
The cardiovascular effects of the SARS-CoV2 (COVID-19) virus are variable and can range from no appreciable symptoms to cardiogenic or vasodilatory shock mediated by such direct mechanisms as myocarditis and direct myocardial viral infiltration, to less direct mechanisms such as inflammatory endothelial dysfunction and increased incidence of thromboembolic disease.1,2 Although the case fatality of this illness is concerning, estimated as 1.8% in the United States (US) since pandemic onset, the majority of patients afflicted with COVID-19 recover fully, though some are afflicted with chronic symptoms i.e., 'Long-COVID'.3,4 From a cardiovascular standpoint, 'Long-COVID' patients may demonstrate reduced 6-minute walk testing capacity, myocardial inflammation, myocarditis, postural orthostatic tachycardia syndrome (dysautonomia), and increased arrhythmia burden.4,5
COVID-19 express its pathogenicity, at least in part, as a vascular disease. By way of the ACE2 receptor on the coronary and systemic vascular endothelium, COVID-19 induces disruption of local inflammatory regulation, induces local thrombogenicity, and causes dysregulation of the renin-angiotensin-aldosterone system (RAAS) system.6,7 As such, moderate or severe COVID-19 infection may directly cause plaque progression and destabilization and increase the macro- and microvascular intracoronary thrombotic burden leading to disruption in coronary blood flow.7 Although the long-term consequences remain to be determined, available evidence suggests that focal arterial vascular inflammation and atherosclerosis correlates well with coronary artery calcium (a strong marker of future atherosclerotic cardiovascular disease [ASCVD] risk).8,9 In the absence of available guidance, the use of statins to modify plaque composition and aid inflammation and/or immunomodulation, respectively, can only be postulated among those who have previously been infected with COVID-19. During acute COVID-19 infection, antecedent statin use was significantly associated with lower mortality at 30 and 60 days follow up compared to non-statin use at the time of hospital admission, respectively.10,11
The presence of chronic cardiovascular comorbidities dramatically affects morbidity and mortality among patients with COVID-19. Notably, those infected with COVID-19 have a higher burden of traditional risk factors such as diabetes, portending an increased risk of mortality.12 The prognosis for individuals with hypertension is markedly worse in the presence of COVID-19 infection, compared to those without.13 Cumulative prior exposure to cigarette smoke is an independent risk factor for hospital admission and death from COVID-19.14 Obesity has also been shown to play a profound role with respect to mechanical ventilatory support and death from COVID-19 in adults.15,16 Notably, COVID-19 has disproportionately affected racial and ethnic minority communities (namely African American and Hispanic), likely stemming from increased presence of traditional risk factors (diabetes, hypertension, obesity), socioeconomic factors, and disparities in access to healthcare.17
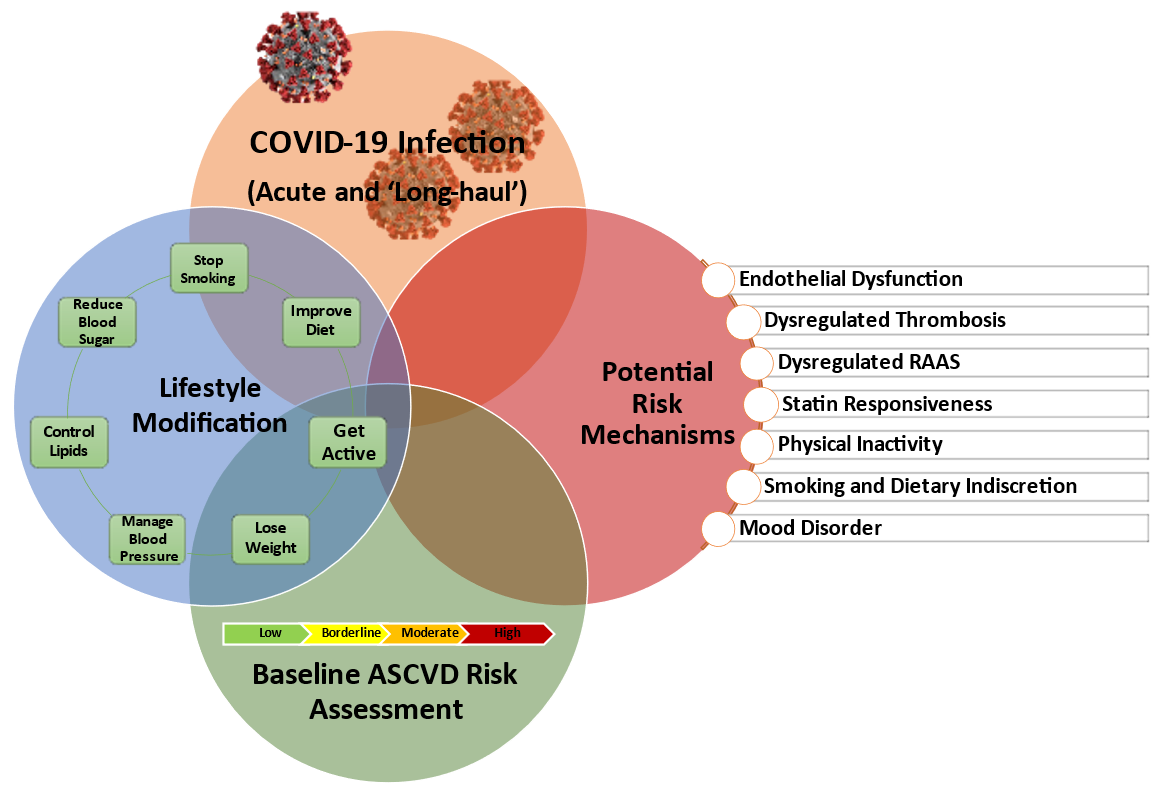
In this context, it is unresolved whether COVID-19 infection in patients with or without previously identified cardiovascular comorbidities is a marker of increased future ASCVD risk (Figure 1). Multiple cardiovascular risk factors including obesity, diabetes mellitus, hypertension, dyslipidemia, hyperuricemia, smoking, physical inactivity and aging can promote damage to the vascular endothelial barrier making viral entry and inflammatory endothelial dysfunction more likely, potentially leading to a more severe COVID-19 infection course.18 Premorbid endothelial dysfunction also may cause a suboptimal initial innate immune response to COVID-19 leading to a delayed and ineffective adaptive immune response.19
Figure 1
Despite wide-spread social disruption and its associated challenges, ASCVD risk reduction strategies should follow guideline proven interventions aimed at optimizing cardiovascular health, such as Life's Simple 7®'s (Figure 1).20,21 With respect to physical activity, the COVID-19 lockdown may have led to increases in population-level interest in and engagement with physical activity; alternatively this has been balanced with a rise in increased screen time and a sedentary lifestyle.22 However, the imperative to promote physical activity should continue and there are myriad opportunities to integrate exercise routines at home.22 COVID-19 has also disrupted routine preventive care, with a decrease in cholesterol testing which may have resulted in suboptimal lipid control.23 Maintaining healthy eating habits during times of stress can trigger unhealthy dietary patterns.24 However, the COVID-19 pandemic provides an opportunity for more thoughtful meal planning. Indeed, eating home cooked meals has been associated with greater adherence to Dietary Approaches to Stop Hypertension (DASH) (low sodium intake) and Mediterranean diets, greater fruit and vegetable intake, and overall declines in adiposity.25 Overcoming nicotine addiction is challenging, made no easier by the pandemic, which may serve as a trigger for smoking relapse and continued smoking behaviors.26 For example, there has been 1% increase in cigarette sales in the first 10 months of 2020 compared to a 4-5% steady annual decline in cigarette sales since 2015.27 However, an opportunity exists to encourage and support quitting tobacco use by offering online cessation services including access to free or low-cost pharmacotherapy (i.e., cessation medications and nicotine replacement therapies), and behavioral counselling.28 Six-month outcome data from Chinese4,29 and American cohorts30 among COVID-19 survivors demonstrated an increased risk of neurological and psychiatric sequelae, namely depression and anxiety. Although necessary to mitigate the spread of COVID-19, mask wearing, physical distancing and reducing physical contact can manifest in psychological strain.31 Social isolation, depression, and anxiety are associated with increased cardiovascular risk.32 Strategies to reduce depression such as engagement in physical activity and maintaining contact with friends/family via telephone or video conferencing, for example, are suggested. Any debilitating symptoms should be addressed with a health care provider.21
Considering other respiratory diseases, a temporal association between influenza infection and acute coronary events is well established.33 Specifically, influenza increases inflammatory activity within coronary plaque leading to destabilization and risk of rupture. Systemic inflammation also potentiates a pro-thrombotic milieu, further promoting plaque thrombosis of ruptured plaque.34 Given the significant reduction in major adverse cardiovascular events (MACE) among those vaccinated against influenza, available ACC/AHA guidelines recommend annual influenza vaccination among individuals with ASCVD (class I, level B) for secondary prevention.35 Notably, the COVID-19 pandemic and corresponding mitigation measures (e.g., face masking, social distancing, hand hygiene), has caused a sharp decline in rates of circulating influenza to global historical lows.36 It remains to be determined if vaccination against COVID-19 will reduce the risk of future adverse cardiac events.37
Summary
COVID-19 disease may increase ASCVD risk directly via vascular endothelial, immune, and thrombotic alterations, while pre-existing ASCVD comorbidities influence morbidity and mortality in infected patients. Clinicians may mitigate future ASCVD risk by engaging patients in guideline recommended risk assessment using the Pooled Cohort Equations and lifestyle modification (Life's Simple 7®) such as increasing physical activity, managing blood pressure, reducing blood sugar, controlling cholesterol (including adherence to lipid lowering therapy), weight loss, smoking cessation, and optimizing nutrition. Although the potential impact of COVID-19 and its vaccination on future ASCVD risk remains to be determined, there are practical strategies available for those previously infected to mitigate preventable cardiovascular disease events as noted above. In particular the ACC COVID-19 Hub provides resources for clinicians directed at managing 'Long-COVID', navigating patient mental health, and the use of telehealth to manage ASCVD conditions during the pandemic.38
References
- Chang WT, Toh HS, Liao CT, Yu WL. Cardiac involvement of COVID-19: a comprehensive review. Am J Med Sci 2021;361:14-22.
- Del Rio C, Collins LF, Malani P. Long-term health consequences of COVID-19. JAMA 2020;324:1723-24.
- COVID Data Tracker (CDC website). 2021. Available at: https://covid.cdc.gov/covid-data-tracker/#trends_dailytrendscases . Accessed 05/04/2021.
- Logue JK, Franko NM, McCulloch DJ, et al. Sequelae in adults at 6 months after COVID-19 infection. JAMA Netw Open 2021;4:e210830.
- Johansson M, Ståhlberg M, Runold M, et al. Long-haul post-COVID-19 symptoms presenting as a variant of postural orthostatic tachycardia syndrome: the Swedish experience. JACC Case Rep 2021;3:573-80.
- Siddiqi HK, Libby P, Ridker PM. COVID-19 - a vascular disease. Trends Cardiovasc Med 2021;31:1-5.
- Bonaventura A, Vecchié A, Dagna L, et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19.Nat Rev Immunol 2021;21:319-29.
- Shapiro MD, Fazio S. From lipids to inflammation: new approaches to reducing atherosclerotic risk. Circ Res 2016;118:732-49.
- Abdelbaky A, Corsini E, Figueroa AL, et al. Focal arterial inflammation precedes subsequent calcification in the same location: a longitudinal FDG-PET/CT study. Circ Cardiovasc Imaging 2013;6:747-54.
- Lee HY, Ahn J, Park J, et al. Beneficial effect of statins in COVID-19-related outcomes-brief report: a national population-based cohort study. Arterioscler Thromb Vasc Biol 2021;41:e175-e182.
- Gupta A, Madhavan MV, Poterucha TJ, et al. Association between antecedent statin use and decreased mortality in hospitalized patients with COVID-19. Nat Commun 2021;12:1325.
- Apicella M, Campopiano MC, Mantuano M, Mazoni L, Coppelli A, Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol 2020;8:782-92.
- Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 2020;5:811-18.
- Lowe KE, Zein J, Hatipoglu U, Attaway A. Association of smoking and cumulative pack-year exposure with COVID-19 outcomes in the Cleveland Clinic COVID-19 Registry. JAMA Intern Med 2021;181:709-11.
- O'Hearn M, Liu J, Cudhea F, Micha R, Mozaffarian D. Coronavirus Disease 2019 hospitalizations attributable to cardiometabolic conditions in the United States: a comparative risk assessment analysis. J Am Heart Assoc 2021;10:e019259.
- Kompaniyets L, Goodman AB, Belay B, et al. Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March-December 2020. MMWR Morb Mortal Wkly Rep 2021;70:355-61.
- Tai DBG, Shah A, Doubeni CA, Sia IG, Wieland ML. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin Infect Dis 2021;72:703-06.
- Yamaoka-Tojo M. Vascular endothelial glycocalyx damage in COVID-19. Int J Mol Sci 2020;21:9712.
- Quinaglia T, Shabani M, Breder I, Silber HA, Lima JAC, Sposito AC. Coronavirus disease-19: the multi-level, multi-faceted vasculopathy. Atherosclerosis 2021;322:39-50.
- Enserro DM, Ramachandran SV, Xanthakis V. Twenty‐year trends in the American Heart Association Cardiovascular Health Score and impact on subclinical and clinical cardiovascular disease: the Framingham Offspring Study. J Am Heart Assoc 2018;7:e008741.
- Khera A, Baum SJ, Gluckman TJ, et al. Continuity of care and outpatient management for patients with and at high risk for cardiovascular disease during the COVID-19 pandemic: a scientific statement from the American Society for Preventive Cardiology. Am J Prev Cardiol 2020;1:100009.
- Ding D, Del Pozo Cruz B, Green MA, Bauman AE. Is the COVID-19 lockdown nudging people to be more active: a big data analysis. Br J Sports Med 2020;54:1183-84.
- Gumuser ED, Haidermota S, Finneran P, Natarajan P, Honigberg MC. Trends in cholesterol testing during the COVID-19 pandemic: COVID-19 and cholesterol testing. Am J Prev Cardiol 2021;6:100152.
- Yau YHC, Potenza MN. Stress and eating behaviors. Minerva Endocrinol 2013;38:255-67.
- Mills S, Brown H, Wrieden W, White M, Adams J. Frequency of eating home cooked meals and potential benefits for diet and health: cross-sectional analysis of a population-based cohort study. Int J Behav Nutr Phys Act 2017;14:109.
- Patanavanich R, Glantz SA. Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine Tob Res 2020;22:1653-56.
- Report on the Impact of the COVID-19 Pandemic on Smoking Cessation (naquitline.org) 2021. Available at: https://cdn.ymaws.com/www.naquitline.org/resource/resmgr/reports-naqc/report_impact__of_covid-19_p.pdf. Accessed 05/06/2021.
- Ahluwalia IB, Myers M, Cohen JE. COVID-19 pandemic: an opportunity for tobacco use cessation. Lancet Public Health 2020;5:e577.
- Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet 2021;397:220-32.
- Taquet M, Geddes JR, Husain M, et al. 6-month neurological and psychiatric outcomes in 236 379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet 2021;397:220-32.
- Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 Coronavirus Disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020;17:1729.
- Hakulinen C, Pulkki-Råback L, Virtanen M, Jokela M, Kivimaki M, Elovainio M. Social isolation and loneliness as risk factors for myocardial infarction, stroke and mortality: UK Biobank cohort study of 479,054 men and women. Heart 2018;104:1536-42.
- Kwong JC, Schwartz KL, Campitelli MA, et al. Acute myocardial infarction after laboratory-confirmed influenza infection. N Engl J Med 2018;378:345-53.
- Musher DM, Abers MS, Corrales-Medina VF. Acute infection and myocardial infarction. N Engl J Med 2019;380:171-76.
- Davis MM, Taubert K, Benin AL, et al. Influenza vaccination as secondary prevention for cardiovascular disease: a science advisory from the American Heart Association/American College of Cardiology. J Am Coll Cardiol 2006;48:1498-1502.
- Olsen SJ, Azziz-Baumgartner E, Budd AP, et al. Decreased influenza activity during the COVID-19 pandemic-United States, Australia, Chile, and South Africa, 2020. Am J Transplant 2020;20:3681-85.
- Heart disease and stroke medical experts urge public to get COVID-19 vaccinations (heart.org). 2021. Available at: https://newsroom.heart.org/news/heart-disease-and-stroke-medical-experts-urge-public-to-get-covid-19-vaccinations?preview=92fe . Accessed 04/10/2021.
- Post-COVID-19 clinics help survivors recover (aamc.org) 2020. Available at: https://www.aamc.org/news-insights/post-covid-19-clinics-help-survivors-recover . Accessed 05/06/2021.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, COVID-19 Hub, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, Implantable Devices, SCD/Ventricular Arrhythmias, Atrial Fibrillation/Supraventricular Arrhythmias, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Diet, Exercise, Hypertension, Smoking
Keywords: Primary Prevention, COVID-19, SARS-CoV-2, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Sedentary Behavior, Smoking Cessation, Renin-Angiotensin System, Calcium, Cardiovascular Diseases, Blood Glucose, Peptidyl-Dipeptidase A, Tobacco Use Disorder, Diet, Mediterranean, Pandemics, Ethnic Groups, Secondary Prevention, Hyperuricemia, Endothelium, Vascular, Adiposity, Influenza, Human, Coronary Vessels, African Americans, Myocarditis, Mental Health, Social Isolation, Postural Orthostatic Tachycardia Syndrome, Virulence, Virus Internalization, Blood Pressure, Depression, Severe Acute Respiratory Syndrome, severe acute respiratory syndrome coronavirus 2, Risk Factors, Minority Groups, Exercise, Immunity, Innate, Atherosclerosis, Smoking, Thrombosis, Dyslipidemias, Diabetes Mellitus, Telemedicine, Delivery of Health Care, Integrated, Delivery of Health Care, Inflammation, Tobacco Use, Risk Assessment, Risk Reduction Behavior, Hypertension, Obesity, Socioeconomic Factors, Arrhythmias, Cardiac, Adaptive Immunity, Hispanic Americans, Vaccination, Anxiety, Lipids, Health Personnel, Immunomodulation, Sodium, Dietary, Hospitals
< Back to Listings