New Guidance on Blood Pressure Management in Low-Risk Adults with Stage 1 Hypertension
Quick Takes
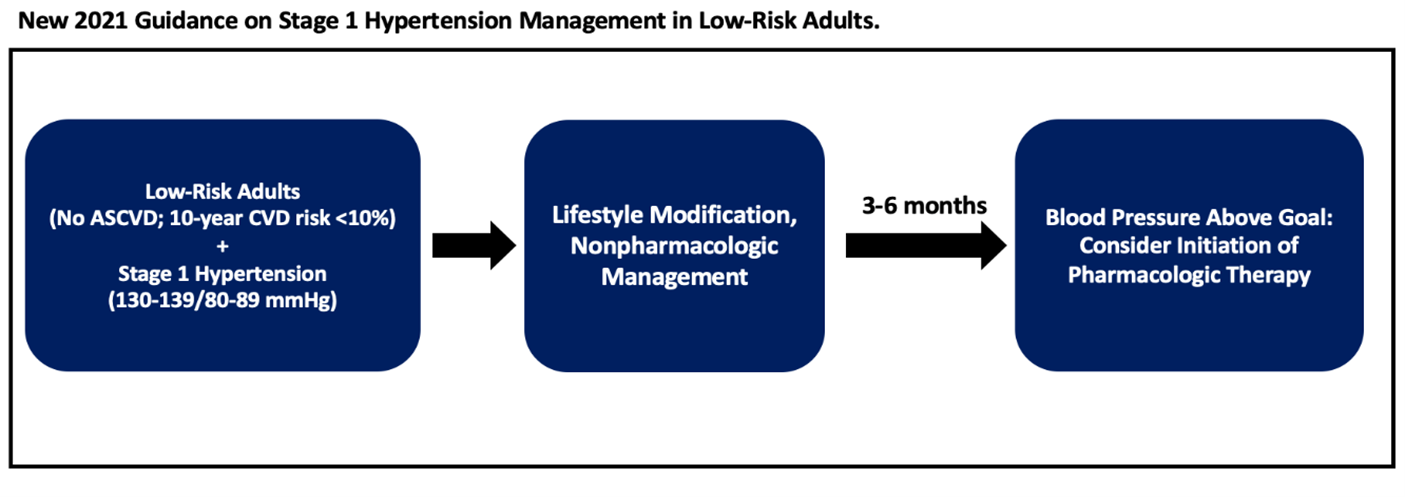
- The AHA/ACC has released a scientific statement in 2021 offering new guidance for management of stage 1 hypertension among patients with low ASCVD risk.
- Among low-risk adults (no ASCVD or 10-year CVD risk <10%) with stage 1 hypertension (blood pressure 130-139/80-89 mmHg), management starts with nonpharmacologic therapy. If blood pressure remains uncontrolled at 3-6 months, consider starting pharmacologic therapy.
More cardiovascular disease (CVD) events are attributable to hypertension (HTN) than any other modifiable CVD risk factor. In recent years, the incidence and prevalence of HTN have increased while rates of HTN control have declined. The American Heart Association (AHA) has recently released a new Scientific Statement regarding management of stage 1 HTN in adults with a low 10-year risk for CVD.1 This is a welcome addition to the guidelines as it fills an important gap in the most recent AHA/American College of Cardiology (ACC) recommendations.
The AHA/ACC started synthesizing evidence and publishing guidelines specifically for HTN in 2014. The last update was in 2017 and the major change at that time was lowering the definition of HTN from ≥140/≥90 mmHg to ≥130/≥80 mmHg.2 It also re-classified "pre-HTN" as elevated blood pressure (120-129/<80 mmHg).
This change was prompted by a growing body of evidence showing a linear relationship between blood pressure and cardiovascular risk, namely that more intensive blood pressure control improves cardiovascular outcomes and survival. The Systolic Blood Pressure Intervention Trial (SPRINT) first published in 2015 (with follow-data published in 2021) randomized 9361 patients with HTN and elevated cardiovascular risk to either an intensive systolic blood pressure (SBP) target (<120 mm Hg) or a standard SBP target (<140 mm Hg).3,4
At 3.3 years of follow-up, they found that the lower SBP target resulted in a significantly lower rate of the composite outcome of myocardial infarction, acute coronary syndrome, stroke, acute decompensated heart failure, or cardiovascular death (1.8% per year vs. 2.4% per year; hazard ratio [HR] 0.73; 95% confidence interval [CI], 0.63 to 0.86). Investigators also found lower all-cause mortality with intensive targets (1.1% per year vs. 1.4% per year; HR 0.75; 95% CI 0.61 to 0.92). Importantly, this landmark study focused on subjects with elevated baseline cardiovascular risk.
There are currently no randomized controlled trial (RCT) data examining the relationship between blood pressure and cardiovascular risk in younger, "low-risk" patients. Because of the number of participants and the extended length of follow-up that would be required in this subgroup to accumulate events and examine risk, the RCTs needed to answer this clinical question would be prohibitively resource-intensive and are unlikely to be performed.
This dearth of RCT data has left a gap in guideline recommendations until now. The 2017 AHA/ACC guidelines recommend lifestyle modification for adults with stage 1 HTN and low 10-year cardiovascular risk. They recommend repeat interval blood pressure measurement every 3 to 6 months, but do not provide guidance for intervention if blood pressure remains above target (<130/<80 mm Hg). The authors of the recent AHA statement seek to address this gap.
The AHA Scientific Statement includes a distinct new recommendation: all patients with stage 1 HTN not meeting blood pressure targets after 6 months of lifestyle modification should be considered for antihypertensive pharmacologic therapy. This applies especially, though not exclusively, to those patients with additional CVD risk factors such as family history of premature CVD, personal history of HTN during pregnancy, or personal history of premature birth.
Figure 1
This new addition to the guidelines reflects the growing appreciation that while short- and intermediate-term risk of HTN and CVD morbidity and mortality may be low, the 20+ year risk can be quite high.5–8 Current tools to estimate 10-year risk do not effectively estimate long-term risk of CVD, especially in younger healthier populations. Even with the presence of stage 1 HTN, younger adults will frequently have low 10-year atherosclerotic cardiovascular disease (ASCVD) risk scores, and even relatively low lifetime risk estimates. However, the cumulative lifetime incidence of HTN (and the associated CVD morbidity and mortality) can be substantial.
In the Coronary Artery Risk Development in Young Adults (CARDIA) study, the incidence of hypertension from ages 18 to 55 years ranged from 40 to 76%. In the Multi-Ethnic Study of Atherosclerosis (MESA), the cumulative incidence of HTN between ages 45 to 85 years ranged from 84 to 93%. Additionally, there are recent observational data showing higher rates of CVD events among patients with untreated stage 1 HTN, even among those younger than 40 years of age.
Whelton et al. examined a cohort of 1457 participants from the MESA study without ASCVD or risk factors and with a mean (standard deviation) age of 58.1 (9.8) years and found higher rates of ASCVD for every 10 mmHg of SBP above 90. The HR for patients with stage 1 hypertension (SBP 120-129 mmHg) was 4.58 (95% CI, 1.47 to 14.27).9
Yano et al. examined CVD risk in 27,081 participants ages 18-49 without coronary disease or antihypertensive therapy at baseline. They followed patients for an average of 31 years. Patients with isolated systolic HTN (SBP ≥ 140 mmHg) had hazard ratios for CVD and coronary mortality risk respectively of 1.23 (95% CI 1.03 to 1.46) and 1.28 (95% CI 1.18 to 2.05) among men and 1.55 (95% CI 1.18 to 2.05) and 2.12 (95% CI 1.49 to 3.01) among women.10
In another study, Yano et al. applied the most recent 2017 ACC/AHA HTN definitions to a cohort of 4851 adults from the CARDIA study with a mean age of 35 and found that compared to those with normal blood pressure, those with elevated blood pressure, stage 1 HTN, and stage 2 HTN had significantly higher rates of CVD events [hazard ratios 1.67 (95% CI, 1.01 to 2.77), 1.75 (95% CI, 1.22 to 2.53), and 3.49 (95% CI, 2.42 to 5.05), respectively].11 The rates of HTN and resultant complications if untreated in younger, lower risk populations as demonstrated in these studies form the basis for the new guideline recommendation.
Table 1: AHA/ACCa Guideline Recommendations by Blood Pressure Category
| BPb Category | Pressure Ranges | Recommendations |
| Normal BP | <120/<80 mmHg | Promote healthy lifestyle; reassess BP annually. |
| Elevated BP | 120-129/<80 mmHg | Start with nonpharmacologic therapy, reassess BP in 3-6 months. |
| Stage1 Hypertension | 130-139/80-89 mmHg | ASCVDc or 10-year CVDd risk ≥10%: Start with both nonpharmacologic and pharmacologic therapy. Reassess BP in 1 month. If at goal, reassess every 3-6 months. If not at goal, assess for adherence and consider intensification of therapy. |
| No ASCVD and 10-year CVD risk <10%: Start with nonpharmacologic therapy, reassess BP in 3-6 months. If not at goal, consider initiation of pharmacologic therapy. |
||
| Stage 2 Hypertension | ≥140/≥90 mmHg | Start with both nonpharmacologic and pharmacologic therapy. Reassess BP in 1 month. If at goal, reassess every 3-6 months. If not at goal, assess for adherence and consider intensification of therapy. |
b: BP, blood pressure.
c: ASCVD, atherosclerotic cardiovascular disease.
d: CVD, cardiovascular disease
While the authors acknowledge that this new recommendation is based upon observational data and intermediate endpoints, the balance of available evidence favors consideration of pharmacologic treatment of stage 1 HTN, even among those traditionally felt to be low risk. The presence of HTN early in life increases risk for progression to more severe hypertension as well as risk for cardiovascular events and mortality across one's lifetime. Earlier intervention among these patients has the potential to blunt the progression of HTN and avert CVD complications. This update to the American guidelines is also consistent with the latest 2018 European Society of Cardiology/European Society of Hypertension guidelines.
Though the perceived benefits would seem to justify pharmacologic intervention in these patients, it will also be important for clinicians to consider the adverse effects of lower blood pressure targets. Documented risks include hypotension, syncope and falls, electrolyte abnormalities, and renal dysfunction. As with many patient care decisions, the question of blood pressure goals and treatment involves both risks and benefits. While the potential benefits are significant, they must be balanced with these risks. Whether or not to treat stage 1 HTN in this population provides a good opportunity for shared clinical decision-making with patients.
References
- Jones DW, Whelton PK, Allen N, et al. Management of stage 1 hypertension in adults with a low 10-year risk for cardiovascular disease: filling a guidance gap: a scientific statement from the American Heart Association. Hypertension 2021;77:e58-e67.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2018;71:e127-e248.
- Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373:2103-16.
- Lewis CE, Fine LJ, Beddhu S, et al. Final report of a trial of intensive versus standard blood-pressure control. N Engl J Med 2021;384:1921-30.
- Berry JD, Dyer A, Cai X, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366:321-29.
- Clark D 3rd, Hall ME, Jones DW. Dilemma of blood pressure management in older and younger adults. Hypertension 2020;75:35-37.
- Wu S, Song Y, Chen S, et al. Blood pressure classification of 2017 associated with cardiovascular disease and mortality in young Chinese adults. Hypertension 2020;76:251-58.
- Son JS, Choi S, Kim K, et al. Association of blood pressure classification in Korean young adults according to the 2017 American College of Cardiology/American Heart Association guidelines with subsequent cardiovascular disease events. JAMA 2018;320:1783.
- Whelton SP, McEvoy JW, Shaw L, et al. Association of normal systolic blood pressure level with cardiovascular disease in the absence of risk factors. JAMA Cardiol 2020;5:1011-18.
- Yano Y, Stamler J, Garside DB, et al. Isolated systolic hypertension in young and middle-aged adults and 31-year risk for cardiovascular mortality: the Chicago Heart Association Detection Project in Industry study. J Am Coll Cardiol 2015;65:327-35.
- Yano Y, Reis JP, Colangelo LA, et al. Association of blood pressure classification in young adults using the 2017 American College of Cardiology/American Heart Association Blood Pressure guideline with cardiovascular events later in life. JAMA 2018;320:1774-82.
Clinical Topics: Acute Coronary Syndromes, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, Acute Heart Failure, Hypertension
Keywords: Dyslipidemias, Cardiovascular Diseases, Antihypertensive Agents, Blood Pressure, American Heart Association, Prevalence, Acute Coronary Syndrome, Confidence Intervals, Premature Birth, Risk Factors, Blood Pressure Determination, Hypertension, Myocardial Infarction, Heart Failure, Stroke, Life Style
< Back to Listings