The Ever-Growing Role of Coronary Artery Calcium in Primary Prevention
Quick Takes
- Data on coronary artery calcium (CAC) scoring has shown a relationship between CAC scores and subsequent atherosclerotic cardiovascular disease (ASCVD) events.
- Selective use of CAC scoring is now ACC/AHA guideline-endorsed to improve risk assessment to accurately identify both those at high risk and at very low risk.
- CAC=0 confers a low risk for future cardiovascular events and mortality and is one of the strongest negative risk markers of ASCVD events.
Agatston and Janowitz published the first technique for coronary artery calcium (CAC) scoring in 1990.1 Given the lack of data at the time correlating CAC with coronary atherosclerosis burden, their algorithm was remarkable yet unactionable. However, as noted in a recent review by Drs. Khurram Nasir and Miguel Cainzos-Achirica, a plethora of data on CAC has since shown a direct, proportional relationship between CAC scores and subsequent ASCVD events.2 In primary prevention, the CAC score is now the best predictor of absolute risk of events over a 10-year period in intermediate risk adults.
The Data for CAC
Clinical risk estimators like the Pooled Cohort Equation (PCE) lack sufficient accuracy in predicting ASCVD events in asymptomatic individuals.3,4 Considering the potential impact of over- or underestimating ASCVD risk on management decisions, prognosis, and healthcare costs, CAC scoring provides an opportunity to improve risk assessment among patients in whom risk management is unclear. CAC can identify both those at higher risk (high CAC scores) and very low risk (those with CAC=0).
Table 1.1 – Landmark CAC Studies
| Study | Year | Patients | Results |
| Prospective Army Coronary Calcium Project5 | 2005 | 2,000 | CAC was associated with an increase in coronary event risk by a factor of 12 during 3 years of follow-up. |
| Rotterdam Study6 | 2005 | 1,795 | Relative risk of coronary events for CAC 101-400, 401-1000, and >1000 (compared with scores of 0-100) were 3.1, 4.6, and 8.3, respectively over 3 years follow up. |
| Cooper Clinic Cohort7 | 2005 | 10,746 | Age-adjusted rates (per 1,000 person-years) of hard events for no detectable CAC and incremental sex-specific thirds of detectable CAC were 0.4, 1.5, 4.8, and 8.7, respectively over 3.5 years. |
| St. Francis Heart Study8 | 2005 | 4,903 | Subjects with ASCVD events had higher baseline CAC scores than those without events. Relative risk for all ASCVD events of CAC ≥100 was 11.1 compared to CAC <100. |
| MESA9 | 2008 | 6,814 | Adjusted risk of a coronary event increased by 7.73 when CAC 101-300 and 9.67 when CAC >300 regardless of ethnicity. |
| Heinz Nixdorf Recall10 | 2010 | 4,129 | Reclassifying intermediate risk subjects with CAC <100 to the low-risk category and CAC >400 to high-risk yielded a reclassification improvement (NRI) of 21.7% and 30.6% for the FRS, respectively. |
| Jackson Heart Study11 | 2015 | 2,944 | In African Americans, CAC was associated with prevalent CVD. CAC improved the diagnostic accuracy of the FRS by 14%. |
| Framingham Offspring12 | 2016 | 3,486 | CAC was most strongly associated with major coronary heart disease independent of Framingham risk factors and improved discriminatory value beyond risk factors for coronary heart disease. |
| CARDIA13 | 2017 | 3,043 | In adults 32 to 46 years, those with any CAC had a 5-fold increase in CHD events and 3-fold increase in CVD events. |
| CAC Consortium14,15 | 2020 | 66,636 | CAC was the most reliable predictor for long-term mortality. |
The Power of Zero
A CAC score of 0 (CAC=0) confers a low risk for future cardiovascular events and mortality and is one of the strongest negative risk markers of ASCVD events over 10-15 years. Importantly, CAC=0 has been associated with event rates below the 2013 guideline defined threshold for statin benefit in intermediate and low-risk individuals; the so called "power of zero". Consequently, more recent 2018 and 2019 guidelines acknowledge CAC=0 can be used to downgrade estimated risk among individuals at borderline or intermediate risk using the PCE. Recent data indicate that an assessment-guided strategy using CAC=0 is cost-effective as compared to initiating statin therapy in all intermediate risk adults.16
Table 1.2 – Notable CAC=0 Studies
| Study | Patients | Results |
| Heinz Nixdorf Recall Study10 | 4,129 | Cardiovascular event rate of 0.16% per year in subjects with CAC=0. |
| CAC Consortium17,18 | 66,363 | CAC=0 associated with very low rates of mortality. |
| MESA19,20,21 | 6,814 | Events with CAC=0 in asymptomatic individuals very small after 10 years; CAC=0 reclassified 1/2 of candidates as not eligible for statin therapy. |
| Walter Reed Cohort22 | 13,644 | NNT 3,571 with a statin in individuals with CAC=0 to prevent first occurrence of MACE through 10 years versus 12 for CAC >100. |
| Shareghi et al23 | 35,765 | 0.03% annual event rate for individuals with CAC=0. |
| Sarwaret al24 | 64,873 | 0.56% of individuals with CAC=0 had a cardiovascular event over 51 months. |
| Valenti et al25 | 9,715 | Mortality rate similar between diabetic and nondiabetic individuals with CAC=0 for the first 5 years. |
| Valenti et al26 | 4,864 | CAC=0 conferred a 15-year warranty period against mortality in individuals at low to intermediate risk unaffected by age or sex. |
CAC in the Guidelines
The prognostic value of CAC in primary prevention has resulted in a prominent role in current clinical practice guidelines around the world. Current United States (US)27,28,29 and European30 guidelines all recommend selective use of CAC for guiding treatment decisions for primary prevention of ASCVD in individuals at borderline or intermediate risk. US guidelines have seen a growing role for CAC, upgrading the most recent CAC related recommendations to IIa. However, European societies have been slower to adopt CAC, recommending it only as a risk modifier to be used to upgrade risk estimations and strengthen the case for preventive statin therapy.
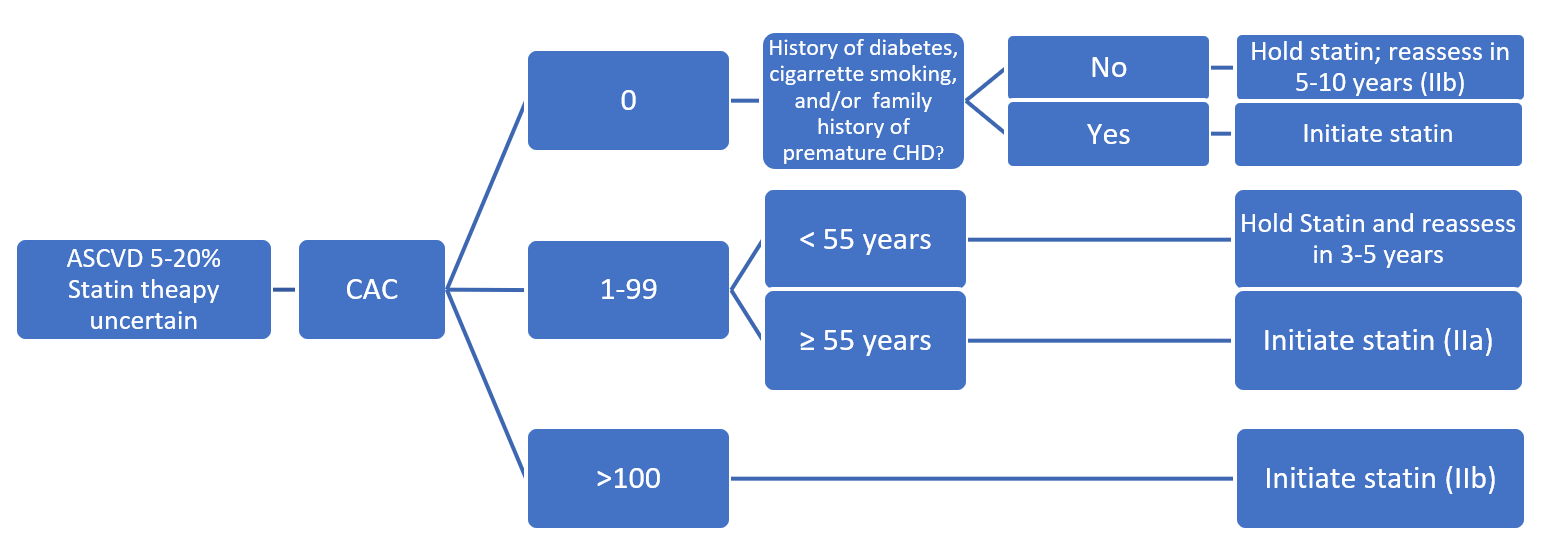
Figure 1.0 – Utilizing CAC According to US Guidelines
Conclusion
As Nasir and Cainzos-Achirica note, the use of CAC in primary prevention is supported by a wealth of data showing that it improves risk prediction when combined with traditional risk factors and scores.
Ongoing studies will continue to elucidate the role of CAC in primary prevention as well as further define the potential role of CAC in allocating of other risk reduction therapies, especially among those with diabetes and patients with severe hypercholesterolemia. As more data become available, CAC will likely become even more incorporated into clinician-patient discussions.
References
- Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827-32.
- Nasir K, Cainzos-Achirica M. Role of coronary artery calcium score in the primary prevention of cardiovascular disease. BMJ 2021;May 04:[Epub ahead of print].
- DeFilippis AP, Young R, Carrubba CJ, et al. An analysis of calibration and discrimination among multiple cardiovascular risk scores in a modern multiethnic cohort. Ann Intern Med 2015;162:266-75.
- Zeitouni M, Nanna MG, Sun JL, Chiswell K, Peterson ED, Navar AM. Performance of guideline recommendations for prevention of myocardial infarction in young adults. J Am Coll Cardiol 2020;76:653-64.
- Taylor AJ, Bindeman J, Feuerstein I, Cao F, Brazaitis M, O'Malley PG. Coronary calcium independently predicts incident premature coronary heart disease over measured cardiovascular risk factors: mean three-year outcomes in the Prospective Army Coronary Calcium (PACC) project. J Am Coll Cardiol 2005;46:807-14.
- Vliegenthart R, Oudkerk M, Hofman A, et al. Coronary calcification improves cardiovascular risk prediction in the elderly. Circulation 2005;112:572-77.
- LaMonte MJ, FitzGerald SJ, Church TS, et al. Coronary artery calcium score and coronary heart disease events in a large cohort of asymptomatic men and women. Am J Epidemiol 2005;162:421-29.
- Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events: the St. Francis Heart Study. J Am Coll Cardiol 2005;46:158-65.
- Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med 2008;358:1336-45.
- Erbel R, Möhlenkamp S, Moebus S, et al. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol 2010;56:1397-406.
- Sung JH, Yeboah J, Lee JE, et al. Diagnostic value of coronary artery calcium score for cardiovascular disease in African Americans: The Jackson Heart Study. Br J Med Med Res 2016;11(2):BJMMR/2016/21449.
- Hoffmann U, Massaro JM, D'Agostino RB Sr, Kathiresan S, Fox CS, O'Donnell CJ. Cardiovascular event prediction and risk reclassification by coronary, aortic, and valvular calcification in the Framingham Heart Study. J Am Heart Assoc 2016;5:e003144.
- Carr JJ, Jacobs DR Jr, Terry JG, et al. Association of coronary artery calcium in adults aged 32 to 46 years with incident coronary heart disease and death. JAMA Cardiol 2017;2:391-99.
- Grandhi GR, Mirbolouk M, Dardari ZA, et al. Interplay of coronary artery calcium and risk factors for predicting CVD/CHD mortality: the CAC Consortium. JACC Cardiovasc Imaging 2020;13:1175-86.
- Adelhoefer S, Uddin SMI, Osei AD, Obisesan OH, Blaha MJ, Dzaye O. Coronary artery calcium scoring: new insights into clinical interpretation -- lessons from the CAC Consortium. Radiol Cardiothorac Imaging 2020;2:e200281.
- Spahillari A, Zhu J, Ferket BS, et al. Cost-effectiveness of contemporary statin use guidelines with or without coronary artery calcium assessment in African American individuals. JAMA Cardiol 2020;5:871-80.
- Blaha M, Budoff MJ, Shaw LJ, et al. Absence of coronary artery calcification and all-cause mortality. JACC Cardiovasc Imaging 2009;2:692-700.
- Blaha MJ, Cainzos-Achirica M, Dardari Z, et al. All-cause and cause-specific mortality in individuals with zero and minimal coronary artery calcium: a long-term, competing risk analysis in the Coronary Artery Calcium Consortium. Atherosclerosis 2020;294:72–79.
- Blaha MJ, Cainzos-Achirica M, Greenland P, et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 2016;133:849-58.
- Sandoval Y, Bielinski SJ, Daniels LB, et al. Atherosclerotic cardiovascular disease risk stratification based on measurements of troponin and coronary artery calcium. J Am Coll Cardiol 2020;76:357-70.
- Nasir K, Bittencourt MS, Blaha MJ, et al. Implications of coronary artery calcium testing among statin candidates according to American College of Cardiology/American Heart Association cholesterol management guidelines: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol 2015;66:1657-68.
- Mitchell JD, Fergestrom N, Gage BF, et al. Impact of statins on cardiovascular outcomes following coronary artery calcium scoring. J Am Coll Cardiol 2018;72:3233-42.
- Shareghi S, Ahmadi N, Young E, Gopal A, Liu ST, Budoff MJ. Prognostic significance of zero coronary calcium scores on cardiac computed tomography. J Cardiovasc Comput Tomogr 2007;1:155-9.
- Sarwar A, Shaw LJ, Shapiro MD, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging 2009;2:675-88.
- Valenti V, Hartaigh BÓ, Cho I, et al. Absence of coronary artery calcium identifies asymptomatic diabetic individuals at low near-term but not long-term risk of mortality: a 15-year follow-up study of 9715 patients. Circ Cardiovasc Imaging 2016;9:e003528.
- Valenti V, Ó Hartaigh B, Heo R, et al. A 15-year warranty period for asymptomatic individuals without coronary artery calcium: a prospective follow-up of 9,715 individuals. JACC Cardiovasc Imaging 2015;8:900-09.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACOM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:3168-3209.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;74:1376-1414.
- Orringer CE, Blaha MJ, Blankstein R, et al. The National Lipid Association scientific statement on coronary artery calcium scoring to guide preventive strategies for ASCVD risk reduction, J Clin Lipidol 2021;15:33-60.
- Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41:111-88.
Clinical Topics: Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Atherosclerotic Disease (CAD/PAD), Homozygous Familial Hypercholesterolemia, Nonstatins, Novel Agents, Statins
Keywords: Dyslipidemias, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Calcium, Prospective Studies, Prognosis, Hypercholesterolemia, Coronary Artery Disease, African Americans, Ethnic Groups, Cost-Benefit Analysis, Follow-Up Studies, Risk Factors, Risk Assessment, Primary Prevention, Diabetes Mellitus, Risk Reduction Behavior, Health Care Costs
< Back to Listings