What We Have Learned from Young Patients with ASCVD
Introduction
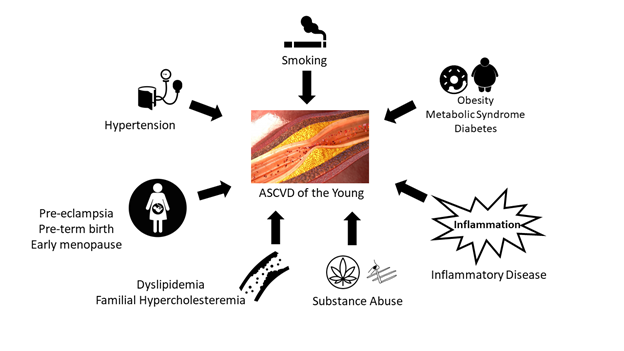
Although the incidence of myocardial infarction (MI) has declined substantially in the United States (US), the incidence among young adults have remained steady for the last ten years.1,2 With increasing rates of cardiovascular (CV) risk factors among the young, including obesity, hypertension, smoking, and diabetes mellitus (DM), atherosclerotic cardiovascular disease (ASCVD) is likely to become more prevalent. In this article, we discuss recent studies that have explored ASCVD among young adults (e.g., age <50 years) and highlight the need for future strategies to optimize preventive care among young adults.
Young Adults with Myocardial Infarction
Recent data has highlighted the increasing burden of MI in the young. The Atherosclerotic Risk in Communities (ARIC) surveillance study found that the annual proportion of acute MI admissions among young adults (age 35-54 years) has increased over time from 27% between 1995 and 1999 to 32% between 2010 and 2014.3 The YOUNG-MI registry is a retrospective cohort study from two large academic medical centers which includes patients who experienced an MI at or before 50 years of age between 2000 and 2016.4 In this registry, the percentage of very young individuals, defined as less than 40 years of age, increased 1.7% per year between the years of 2007-2016.5 Many patients who experienced an MI at a young age have pre-existing CV risk factors, and although 80-90% of such individuals have at least one risk factor prior to their MI, this is often unrecognized and untreated.6,7
Smoking may be a particularly strong predictor of future MI in the young. A recent study that examined smoking among the young observed a nine-fold increased risk in men and 13-fold increased risk of MI in women.8 Furthermore, in a study that examined 280,736 young MI patients (age 18-44), smoking was the most prevalent risk factor at 56.8%.6 Notably, although the prevalence of smoking has decreased in the general population, it has increased among young MI patients. In the YOUNG-MI registry, patients who quit smoking post-MI had a substantially reduced risk of recurrent events, highlighting the importance of smoking cessation counseling in both primary and secondary prevention.9
Similarly, obesity and metabolic syndrome has increased among young adults. In a retrospective study of 2,082 patients with MI who underwent percutaneous coronary intervention, almost half of young patients (<50) with MI had metabolic syndrome and these patients had the highest incidence of a recurrent MI compared with other groups.10 Diabetes is another significant risk factor among the young. In the YOUNG-MI registry, one in five patients had DM at the time of their index hospitalization which was associated with increased CV mortality and all-cause mortality.11
Familial hypercholesterolemia (FH) is a prevalent genetic risk factor among young individuals with ASCVD, which is often underrecognized. In the YOUNG-MI registry, approximately 10% had clinically defined FH, yet only approximately half of such individuals were on high-intensity statin therapy prior to MI and approximately one-third were not discharged on high-intensity statin post-MI.12 In the VITAL registry, a multicenter cross-sectional study that utilized clinical and administrative data from the Veterans Affairs (VA) health care system, patients with ASCVD who had premature (age <55 years for men and age <65 years for women) ASCVD compared to non-premature ASCVD were less likely to be prescribed aspirin or statins and less likely to adhere to statin therapy.13
Substance use is an increasingly recognized risk factor for MI and is particularly prevalent in young adults who experience an MI. Studies have reported rates of cocaine use as high as 25% among the young; in the YOUNG-MI registry, cocaine use was detected in 5% of patients, while marijuana use was found in 6% of patients.14 Importantly, the prevalence of such substance use was even higher among the very young (age <40 years).5,15 Given the recent legalization of marijuana in many US states, its increased use will likely continue.16 Lastly, autoimmune systemic inflammatory conditions are important to recognize as a risk factor for ASCVD in the young. These autoimmune inflammatory conditions often initially manifest in teenage/young adulthood and it is well established that current ASCVD calculators underestimate CV risk in the presence of such conditions.17 A recent study demonstrated that CV risk is especially underestimated in female and younger (age <55) rheumatoid arthritis patients.18 In the YOUNG-MI registry, approximately 2.5% had evidence of systemic inflammatory conditions (psoriasis, rheumatoid arthritis (RA), or systemic lupus erythematosus (SLE)), and these patients experienced higher all-cause mortality, even when compared with patients who had a similar CV risk factor profile.19 Furthermore, in the VITAL registry, patients with RA, SLE, and inflammatory bowel disease had a higher prevalence of premature and extremely premature (<40 years) ACSVD compared with age-matched controls.20,21 Autoimmune conditions have a predilection for women, and sex-related disparities are also important to consider.22
CV Risk Under-Recognition
Even though many young adults with CV risk factors are at risk for developing CVD, many are not treated and are classified as 'low-risk' based on current guidelines. This is due to the fact that age remains a dominant factor in the pooled cohort equation (PCE) to estimate 10-year ASCVD risk.23 The PCE is validated for age >40 and thus risk calculation for age <40 is unclear.23 In the YOUNG-MI registry, only 31% of patients would have met criteria for statin eligibility per the American College of Cardiology/American Heart Association (ACC/AHA) guidelines.7 A study that examined young patients with first MI at Duke University Medical Center found similar results and further described that most young adults with premature MI are not recommended for intensive post-MI lipid management despite having a much longer potential life span for recurrent CV events. Younger individuals with very high-risk criteria (i.e., history of multiple ASCVD events or one major ASCVD event plus high-risk conditions) were also at higher risk of major adverse cardiovascular events.24,25 Thus, there is a clear need for better methods to assess CV risk in younger individuals.
Screening for Atherosclerosis in the Young
One method to identify higher risk young individuals who are at greater risk for cardiovascular events is the use of coronary artery calcium (CAC) testing.26 The presence of any calcified coronary plaque has been shown to improve risk stratification among young adults.27-29 However, the absence of CAC at a very young age does not offer the same negative predictive value as it does in older individuals. Thus, a score of zero at a young age (e.g., age <40, and especially among young women) should not be used as a basis to defer treatments that may otherwise be indicated, such as other risk enhancing factors. In these scenarios, it is reasonable to initiate statin therapy. In selected cases, high risk adults may have a higher burden of non-calcified plaque (i.e., chronic inflammatory disease, HIV) and testing with coronary computerized tomography (CT) angiography may be reasonable in such scenarios.30
Other than imaging testing, evaluation for other underlying risk enhancers (e.g., lipoprotein(a), high sensitivity C-reactive protein [hs-CRP], sex specific risk factors in women) can also be employed to identify higher risk individuals.23 Sex-specific risk factors can occur across the reproductive life course and includes early menarche, pre-eclampsia, pre-term birth, and early natural or surgical menopause.31 Lastly, current ASCVD risk calculators do not include genetic risk factors. Polygenic risk scores (PRS) are emerging as an additional approach to enhance risk prediction. Recently, in a study that examined the addition of PRS to cohorts that span cross-ethnicity and cross-ancestry was shown to enhance risk prediction; however, analysis with larger datasets and further validation studies are needed to understand how these risk scores can be applied routinely in clinical practice.32
A Clinical Framework for the Prevention and Management of ASCVD in the Young
While it is well known that the development of atherosclerosis begins at a young age, most prevention efforts, including clinical trials focusing on various preventive medical treatments, have generally focused on older adults. The challenges with designing clinical trials in young adults is that event rates are generally low, thus necessitating a large sample size or a long follow-up time. A recent NHLBI workshop suggested that CAC testing may enhance patient selection for such a trial,33 in addition, another potential mechanism to assess the efficacy of various preventive therapies is to assess for differences in plaque progression based on coronary CT angiography.34
Until we have prospective CVD prevention trials focused on young adults, it is important to recognize and aggressively treat underlying CV risk factors, as is also advocated for older adults, including blood pressure control, lipid lowering therapies, diabetes, and obesity. In addition, all individuals need to be counseled regarding the importance of tobacco cessation and avoidance of cocaine and marijuana. Lifestyle interventions should be recommended at all ages, including regular aerobic physical activity and a diet which avoids processed food and emphasizes the intake of fruits, vegetables, whole grains, and legumes.23
Conclusion
In summary, recent evidence has established that risk factors play a significant role in the development of ASCVD in the young. While lifestyle interventions should be implemented in all individuals regardless of age, the optimal time for initiating various pharmacological treatments is not well defined. While there is a growing consensus that such treatments should be started at an earlier age, clinical trials focusing on young adults have not been performed. Improved risk assessment — whether by enhanced risk scores, imaging for atherosclerosis, or based on genetic risk scores — may allow the identification of young individuals who may benefit from aggressive pharmacological therapies prior to developing ASCVD events.
Figure 1: Risk factors for ASCVD in Young Adults
References
- Gupta A, Wang Y, Spertus JA, et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. J Am Coll Cardiol 2014;64:337–45.
- Wilmot KA, O'Flaherty M, Capewell S, Ford ES, Vaccarino V. Coronary heart disease mortality declines in the United States From 1979 through 2011: evidence for stagnation in young adults, especially women. Circulation 2015;132:997–1002.
- Arora S, Stouffer GA, Kucharska-Newton AM, et al. Twenty-year trends and sex differences in young adults hospitalized with acute myocardial infarction. Circulation 2019;139:1047–56.
- Singh A, Collins B, Qamar A, et al. Study of young patients with myocardial infarction: design and rationale of the YOUNG-MI Registry. Clin Cardiol 2017;40:955–61.
- Yang J, Biery DW, Singh A, et al. Risk factors and outcomes of very young adults who experience myocardial infarction: the Partners YOUNG-MI Registry. Am J Med 2020;133:605-612.e1.
- Yandrapalli S, Nabors C, Goyal A, Aronow WS, Frishman WH. Modifiable risk factors in young adults with first myocardial infarction. J Am Coll Cardiol 2019;73:573–84.
- Singh A, Collins BL, Gupta A, et al. Cardiovascular risk and statin eligibility of young adults after an MI: Partners YOUNG-MI Registry. J Am Coll Cardiol 2018;71:292–302.
- Palmer J, Lloyd A, Steele L, et al. Differential risk of ST-segment elevation myocardial infarction in male and female smokers. J Am Coll Cardiol 2019;73:3259–66.
- Biery DW, Berman AN, Singh A, et al. Association of smoking cessation and survival among young adults with myocardial infarction in the Partners YOUNG-MI Registry. JAMA Netw Open 2020;3:e209649.
- Kim I, Kim MC, Sim DS, et al. Effect of the metabolic syndrome on outcomes in patients aged <50 years versus >50 years with acute myocardial infarction. Am J Cardiol 2018;122:192–8.
- Divakaran S, Singh A, Biery D, et al. Diabetes is associated with worse long-term outcomes in young adults after myocardial infarction: the Partners YOUNG-MI Registry. Diabetes Care 2020;43:1843-50.
- Singh A, Gupta A, Collins BL, et al. Familial hypercholesterolemia among young adults with myocardial infarction. J Am Coll Cardiol 2019;73:2439–50.
- Mahtta D, Ramsey DJ, Al Rifai M, et al. Evaluation of aspirin and statin therapy use and adherence in patients with premature atherosclerotic cardiovascular disease. JAMA Netw Open 2020;3:e2011051.
- DeFilippis EM, Singh A, Divakaran S, et al. Cocaine and marijuana use among young adults with myocardial infarction. J Am Coll Cardiol 2018;71:2540–51.
- Mahtta D, Ramsey D, Krittanawong C, et al. Recreational substance use among patients with premature atherosclerotic cardiovascular disease. Heart 2021;107:650–6.
- DeFilippis EM, Bajaj NS, Singh A, et al. Marijuana use in patients with cardiovascular disease: JACC Review Topic of the Week. J Am Coll Cardiol 2020;75:320–32.
- Colaco K, Ocampo V, Ayala AP, et al. Predictive utility of cardiovascular risk prediction algorithms in inflammatory rheumatic diseases: a systematic review. J Rheumatol 2020;47:928-38.
- Rohrich DC, van de Wetering EHM, Rennings AJ, et al. Younger age and female gender are determinants of underestimated cardiovascular risk in rheumatoid arthritis patients: a prospective cohort study. Arthritis Res Ther 2021;23:2.
- Weber B, Biery DW, Singh A, et al. Association of inflammatory disease and long-term outcomes among young adults with myocardial infarction: the Mass General Brigham YOUNG-MI Registry. Eur J Prev Cardiol 2021;Mar 30:[Epub ahead of print].
- Mahtta D, Gupta A, Ramsey DJ, et al. Autoimmune rheumatic diseases and premature atherosclerotic cardiovascular disease: an analysis from the VITAL Registry. Am J Med 2020;133:1424-32.e1.
- Lee MT, Mahtta D, Chen L, et al. Premature atherosclerotic cardiovascular disease risk among patients with inflammatory bowel disease. Am J Med 2021:Apr 1:[Epub ahead of print].
- Lee MT, Mahtta D, Ramsey DJ, et al. Sex-related disparities in cardiovascular health care among patients with premature atherosclerotic cardiovascular disease. JAMA Cardiol 2021;Apr 21:[Epub ahead of print].
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;74:e177-e232.
- Zeitouni M, Nanna MG, Sun JL, Chiswell K, Peterson ED, Navar AM. Performance of guideline recommendations for prevention of myocardial infarction in young adults. J Am Coll Cardiol 2020;76:653–64.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: executive summary. J Am Coll Cardiol 2019;73:3168–3209.
- Orringer CE, Blaha MJ, Blankstein R, et al. The National Lipid Association scientific statement on coronary artery calcium scoring to guide preventive strategies for ASCVD risk reduction. J Clin Lipidol 2021;15:33–60.
- Carr JJ, Jacobs DR Jr, Terry JG, et al. Association of coronary artery calcium in adults aged 32 to 46 years with incident coronary heart disease and death. JAMA Cardiol 2017;2:391–99.
- Miedema MD, Nauffal VD, Singh A, Blankstein R. Statin therapy for young adults: a long-term investment worth considering. Trends Cardiovasc Med 2020;30:48–53.
- Miedema MD, Dardari ZA, Nasir K, et al. Association of coronary artery calcium with long-term, cause-specific mortality among young adults. JAMA Netw Open 2019;2:e197440.
- Lerman JB, Joshi AA, Chaturvedi A, et al. Coronary plaque characterization in psoriasis reveals high-risk features that improve after treatment in a prospective observational study. Circulation 2017;136:263–76.
- Freaney PM, Khan SS, Lloyd-Jones DM, Stone NJ. The role of sex-specific risk factors in the risk assessment of atherosclerotic cardiovascular disease for primary prevention in women. Curr Atheroscler Rep 2020;22:46.
- Weale ME, Riveros-Mckay F, Selzam S, et al. Validation of an integrated risk tool, including polygenic risk score, for atherosclerotic cardiovascular disease in multiple ethnicities and ancestries. Am J Cardiol 2021;148:157–64.
- Greenland P, Michos ED, Redmond N, et al. Primary prevention trial designs using coronary imaging: a National Heart, Lung, and Blood Institute workshop. JACC Cardiovasc Imaging 2021;14:1454-65.
- Jaffer FA, Blankstein R. Getting down with diet and exercise for coronary artery disease treatment: insights from the DISCO-CT Study. JACC Cardiovasc Imaging 2021;14:1203-05.
Clinical Topics: Cardiovascular Care Team, Congenital Heart Disease and Pediatric Cardiology, Diabetes and Cardiometabolic Disease, Dyslipidemia, Invasive Cardiovascular Angiography and Intervention, Prevention, CHD and Pediatrics and Arrhythmias, CHD and Pediatrics and Interventions, CHD and Pediatrics and Prevention, CHD and Pediatrics and Quality Improvement, Advanced Lipid Testing, Homozygous Familial Hypercholesterolemia, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Diet, Exercise, Hypertension, Smoking
Keywords: Young Adult, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Retrospective Studies, C-Reactive Protein, Cross-Sectional Studies, Calcium, Smoking Cessation, Marijuana Smoking, Metabolic Syndrome, Lipoprotein(a), American Heart Association, Secondary Prevention, Coronary Vessels, Patient Selection, National Heart, Lung, and Blood Institute (U.S.), Cocaine, Ethnic Groups, Aspirin, Longevity, Fabaceae, Menarche, Pre-Eclampsia, Cardiovascular Diseases, Predictive Value of Tests, Blood Pressure, Hypercholesterolemia, Prospective Studies, Diet, Myocardial Infarction, Atherosclerosis, Smoking, Risk Factors, Risk Assessment, Hospitalization, Life Style, Obesity, Diabetes Mellitus, Registries, Percutaneous Coronary Intervention, Hypertension, Delivery of Health Care, Arthritis, Rheumatoid, Lupus Erythematosus, Systemic, Exercise, Inflammatory Bowel Diseases, Psoriasis, Academic Medical Centers
< Back to Listings