South Asian Cardiovascular Health: Lessons Learned from the National Lipid Association Scientific Statement
Quick Takes
- Compared to other ethnic subgroups, SAUS have a disproportionately greater burden of ASCVD, which often occurs earlier in life (<50 years) and is more aggressive.
- Cardiovascular risk among SAUS includes a constellation of traditional risk factors (hypertension, diabetes mellitus, and smoking) superimposed on a milieu of unhealthy modifiable behaviors (e.g. limited physical activity and unhealthy dietary patterns).
- Early recognition and treatment of cardiovascular risk factors and in selected individuals, appropriate imaging should help identify and mitigate the burden of ASCVD events.
Introduction
South Asians in the United States (SAUS) include a heterogeneous group of individuals who trace their ancestry to the Indian subcontinent (India, Pakistan, Bangladesh, Sri Lanka, Maldives, Bhutan, and Nepal). Despite the common origin from the Indian subcontinent, there are considerable difference lifestyle patterns and dietary habits.1
When compared to other ethnic subgroups, SAUS have a disproportionately greater burden of atherosclerotic cardiovascular disease (ASCVD) which often occurs earlier in life (<50 years) and is more aggressive. In this setting, the recent scientific statement from the National Lipid Association provides further guidance on the prevention of ASCVD among SAUS.2
Limitations of Available ASCVD Risk Assessment Specific to SAUS
While risk assessment is a fundamental aid for ASCVD risk reduction counseling, risk prediction, discrimination and calibration in SAUS remains challenging because 1) available risk algorithms have not been derived from or prospectively validated in SA adults living in North America; 2) limited considerations have been given for native versus migrant populations; and 3) there is a limited availability of disaggregated data, masking meaningful ASCVD health differences in SA subgroups.3,4 As such, population-specific risk assessment tools unreliably estimate risk in this group.
For example, when accounting for ethnicity in the United Kingdom (UK), the National Institute for Health & Care Excellence (NICE) guidelines recommended an adjustment factor to the Framingham Risk Score (FRS) for SA (FRS multiplied by 1.4 for SA men; no recommendation for women).5 Of note, the FRS and UK Prospective Diabetes Study underestimates risk in SA when compared to a white European population.6 QRISK2 underestimates risk in SA women.7 The 3rd Joint British Societies' cardiovascular disease (CVD) risk calculator (incorporates QRISK and QRISK2 databases) accounts for SA ethnicity, but also underestimates risk when considering the very small proportion (2% and 0.7%, respectively) of SA adults included in the cohort.8,9 The World Health Organization (WHO) risk charts have been shown to misclassify high-risk SA to low-risk categories.10
The INTERHEART Modifiable Risk-Score has been internally and externally validated for the prediction of future ASCVD risk in SA, however, its application is limited considering case-control data used to develop the risk calculator.11 SA ethnicity is defaulted to "white" race when using the American Heart Association (AHA)/American College of Cardiology (ACC) Pooled Cohort Equations (PCE), resulting in risk underestimation. The 2016 European prevention guidelines and 2018 AHA/ACC multi-society cholesterol guidelines now include SA ethnicity as a risk-enhancer when considering the initiation of statin therapy.12,13
Highly Prevalent Risk Factors
Cardiovascular risk among SAUS includes a constellation of traditional risk factors (hypertension, diabetes mellitus, and smoking) superimposed on a milieu of unhealthy modifiable behaviors (e.g. limited physical activity and unhealthy dietary patterns).
The age-adjusted prevalence of hypertension was estimated around 27% in the New York City Community Health Survey and 43% in men and 35% in women in the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study.14,15 SA adults with a history of hypertension have an increased risk of acute myocardial infarction (odds ratio 2.69, p = 0.001).16,17
Diabetes is a highly prevalent cardiovascular risk factor among SAUS patients. Findings from the MASALA study demonstrate a prevalence of 25% of diabetes and 33% of prediabetes.18 In conjunction with the high prevalence of diabetes, SAUS have a disproportionately elevated burden of metabolic syndrome, which is defined as increased body mass index (BMI) and/or waist circumference, low HDL-C, elevated triglycerides, and insulin resistance.
The predilection to these risk factors is sometimes compounded by less-than-ideal modifiable lifestyle patterns including smoking, sedentary activity, and unhealthy dietary patterns such as increased intake of animal protein, fried foods, snacks that are rick in refined carbohydrates, sweets (i.e. mithai, jalebi, and gulab jamun), and other foods that are high in saturated fats (i.e. ghee, coconut oil, and paneer).2 With respect to biomarkers, SAUS, on average, tend to have higher levels of lipoprotein(a) [Lp(a)], which is independently associated with an increased risk of major adverse cardiovascular events including coronary heart disease (CHD) and stroke.2
Management of Modifiable Cardiovascular Risk Factors
Despite the high burden of disease in these individuals, there is robust potential for intervention to reduce ASCVD risk. First, lifestyle modifications such as increased physical activity and healthy eating should be emphasized. Regular and culturally tailored physical activity (e.g. Bollywood dancing, bhangra, yoga, or brisk walking) at a minimum of 150 minutes per week at moderate intensity is recommended.19 Increasing intake of fresh fruit, vegetables, whole grains, low fat, and lean proteins should be emphasized in conjunction with reducing the intake of tropical oils, fried, salty, sugary or processed foods, and refined carbohydrates.1 Healthy cooking lessons and referrals to culturally tailored dietary therapy may assist in making these changes.
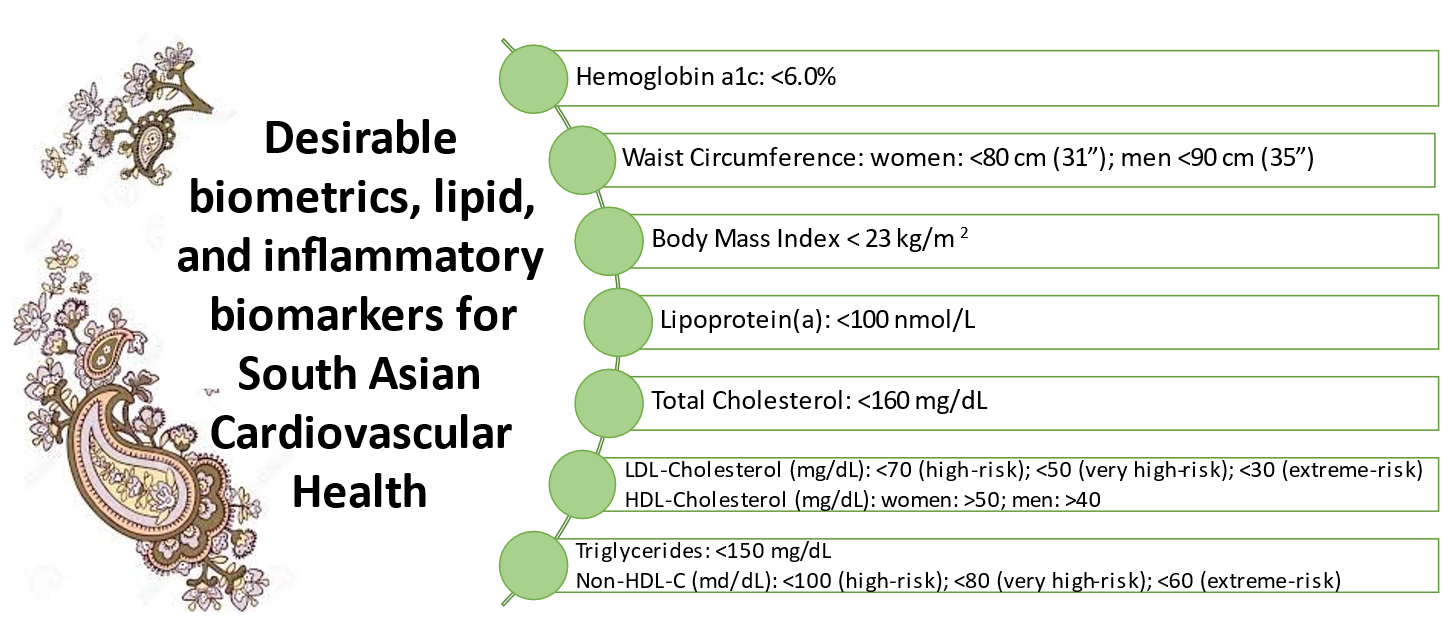
Residual risk for ASCVD conveyed by hypertension, diabetes, and hyperlipidemia should be targeted with guideline-recommended pharmacologic therapy for primary and secondary prevention.2 Table 1 depicts desirable metrics to optimize cardiovascular health in SAUS.2
Figure 1: Desirable Levels of Cardiovascular Disease Risk Factors For South Asian Patients
Further Risk Assessment – Coronary Artery Calcium
In addition to frequent and universal screening for traditional risk factors and metrics, the use of coronary artery calcium (CAC), a highly specific marker of subclinical atherosclerosis, may be a useful test to improve risk stratification in SAUS.20-24 The extent of ASCVD-risk overestimation using the PCE is greater among SA adults considered at low/intermediate risk than among white adults, such that intermediate-risk SA individuals have a 73% higher odds of CAC=0.20 The presence of a family history of CHD is associated with a high burden of CAC (>300).22 With respect to hypertension management, CAC may help identify those SA adults who would best qualify for lifestyle optimization and anti-hypertensive pharmacotherapy.14 When compared to available non-traditional risk markers, CAC scoring should be the preferred noninvasive modality for further risk refinement in SA.2,25
Conclusion
It is critical that appropriate and adequate strategies be developed to screen and manage ASCVD in SAUS. It is apparent that in addition to genetic and established coronary risk factors, the higher prevalence of ASCVD and related cardiovascular events are also related to poor diet choices and unhealthy lifestyle patterns. Structured interventions at a societal level for increasing physical activity and implementing dietary are needed.
In addition to these preventive strategies, earlier recognition, and treatment of cardiovascular risk factors and in selected individuals, appropriate imaging should help identify and mitigate the burden of ASCVD events. Future studies should be geared towards understanding the reason behind the disproportionately higher burden of ASCVD in SAUS and developing appropriate therapeutic strategies in a disaggregated manner. Equally important is the promotion and engagement of existing SA community-level ASCVD programs to further educate, promote health literacy, and provide culturally competent health care (Table 1).
Table 1: South Asian Cardiovascular Health and Prevention Clinics
| Program Name and Physicians | State and City |
| California | |
| South Asian Heart Center | Fremont, Los Gatos, Mountain View |
| Stanford Center for Asian Health Research and Education (CARE)/ Stanford South Asian Translational Heart Initiative (SSATHI) | Portola Valley, Santa Clara, Stanford |
| Mediators of Atherosclerosis in South Asians Living in America (MASALA) (Alka Kanaya MD) |
San Francisco |
| PRevention and AwareNess for South Asians (PRANA) – Sutter Health/Palo Alto Medical Foundation | Los Altos, Los Gatos, Fremont, Palo Alto, San Jose |
| Georgia | |
| NCS Cardiology | Cumming, Johns Creek |
| Emory - Atlanta South Asian Health Alliance (ASHA) | Atlanta |
| Illinois | |
| Advocate Health Care - South Asian Cardiovascular Center (SACC) | Park Ridge |
| South Asian Healthy Lifestyle Initiative (SAHELI) (Namratha Kandula MD) |
Chicago, Evanston |
| Maryland | |
| Ciccarone Center at Greater Baltimore Medical Center and Greenspring Station (Fall 2021) (Roger Blumenthal MD, Michael Blaha MD, Garima Sharma MBBS & Jaideep Patel MD) |
Towson |
| Minnesota | |
| SEWA-AIFW (Asian Indian Family Wellness) | Minneapolis |
| New York | |
| Memorial Sloan Kettering Cancer Center – South Asian Health Initiative (SAHI) | New York |
| New Jersey | |
| Rutgers – Robert Wood Johnson Medical School, South Asian Total Health Initiative (SATHI) | New Brunswick |
| Ohio | |
| The Christ Hospital Outpatient Center – Montgomery, South Asian Comprehensive Cardiovascular Clinic | Cincinnati |
| Cardiovascular Health in Asian Indians (CHAI) (Ankur Kalra MD) |
Cleveland |
| Texas | |
| Baylor Scott & White Heart Hospital Baylor Plano (Anandita Agarwala MD) |
North Dallas/Plano |
| Baylor College of Medicine Cardiometabolic Initiative (Salim Virani MD) |
Houston |
| Canada | |
| South Asian Risk Assessment Clinic | Ontario – Brampton, Toronto |
| Fraser Health – South Asian Health Institute | British Columbia – multiple locations |
| *List is not comprehensive, however we encourage the reader to seek out South Asian related ASCVD resources near them if available. | |
References
- Volgman AS, Palaniappan LS, Aggarwal NT, et al. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation 2018;138:e1-e34.
- Kalra D, Vijayaraghavan K, Sikand G, et al. Prevention of atherosclerotic cardiovascular disease in South Asians in the US: a clinical perspective from the National Lipid Association. J Clin Lipidol 2021;15:402-22.
- Findlay SG, Kasliwal RR, Bansal M, Tarique A, Zaman A. A comparison of cardiovascular risk scores in native and migrant South Asian populations. SSM Popul Health 2020;11:100594.
- Manjunath L, Chung S, Li J, Shah H, Palaniappan L, Yong CM. Heterogeneity of treatment and outcomes among asians with coronary artery disease in the United States. J Am Heart Assoc 2020;9:e014362.
- Cooper A, O'Flynn N, Group GD. Risk assessment and lipid modification for primary and secondary prevention of cardiovascular disease: summary of NICE guidance. BMJ 2008;336:1246-48.
- Bellary S, O'Hare JP, Raymond NT, et al. Premature cardiovascular events and mortality in South Asians with type 2 diabetes in the United Kingdom Asian Diabetes Study - effect of ethnicity on risk. Curr Med Res Opin 2010;26:1873-39.
- Tillin T, Hughes AD, Whincup P, et al. Ethnicity and prediction of cardiovascular disease: performance of QRISK2 and Framingham scores in a U.K. tri-ethnic prospective cohort study (SABRE--Southall And Brent REvisited). Heart 2014;100:60-67.
- Hippisley-Cox J, Coupland C, Vinogradova Y, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ 2008;336:1475-82.
- Hippisley-Cox J, Coupland C, Robson J, Brindle P. Derivation, validation, and evaluation of a new QRISK model to estimate lifetime risk of cardiovascular disease: cohort study using QResearch database. BMJ 2010;341:c6624.
- Bansal M, Kasliwal RR, Trehan N. Comparative accuracy of different risk scores in assessing cardiovascular risk in Indians: a study in patients with first myocardial infarction. Indian Heart J 2014 2014;66:580-86.
- McGorrian C, Yusuf S, Islam S, et al. Estimating modifiable coronary heart disease risk in multiple regions of the world: the INTERHEART Modifiable Risk Score. Eur Heart J 2011;32:581-89.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:e285-e350.
- Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 2016;37:2315-81.
- Yi SS, Thorpe LE, Zanowiak JM, Trinh-Shevrin C, Islam NS. Clinical characteristics and lifestyle behaviors in a population-based sample of Chinese and South Asian immigrants with hypertension. Am J Hypertens 2016;29:941-47.
- Kandula NR, Kanaya AM, Liu K, et al. Association of 10-year and lifetime predicted cardiovascular disease risk with subclinical atherosclerosis in South Asians: findings from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. J Am Heart Assoc 2014;3:e001117.
- Joshi P, Islam S, Pais P, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 2007;297:286-94.
- Pais P, Pogue J, Gerstein H, et al. Risk factors for acute myocardial infarction in Indians: a case-control study. Lancet 1996;348:358-63.
- Shah AD, Vittinghoff E, Kandula NR, Srivastava S, Kanaya AM. Correlates of prediabetes and type II diabetes in US South Asians: findings from the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Ann Epidemiol 2015;25:77-83.
- Piercy KL, Troiano RP. Physical activity guidelines for Americans from the US Department of Health and Human Services. Circ Cardiovasc Qual Outcomes 2018;11:e005263.
- Al Rifai M, Cainzos-Achirica M, Kanaya AM, et al. Discordance between 10-year cardiovascular risk estimates using the ACC/AHA 2013 estimator and coronary artery calcium in individuals from 5 racial/ethnic groups: Comparing MASALA and MESA. Atherosclerosis 2018;279:122-29.
- Mehta A, Patel J, Al Rifai M, et al. Inflammation and coronary artery calcification in South Asians: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) study. Atherosclerosis 2018;270:49-56.
- Patel J, Al Rifai M, Cainzos-Achirica M, et al. Family history of CHD is associated with severe CAC in South Asians: comparing the MASALA and MESA studies. JACC Cardiovasc Imaging 2017;10:958-60.
- Al Rifai M, Kanaya AM, Kandula NR, et al. Distribution of calcium volume, density, number, and type of coronary vessel with calcified plaque in South Asians in the US and other race/ethnic groups: the MASALA and MESA studies. Atherosclerosis 2021;317:16-21.
- Patel J, Mehta A, Mahmoud A, et al. Hypertension guidelines and coronary artery calcification among South Asians: results from MASALA and MESA. Am J Prev Cardiol 2021;6:100158.
- Blaha MJ, Cainzos-Achirica M, Greenland P, et al. Role of coronary artery calcium score of zero and other negative risk markers for cardiovascular disease: The Multi-Ethnic Study of Atherosclerosis (MESA). Circulation 2016;133:849-58.
Clinical Topics: Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Advanced Lipid Testing, Hypertriglyceridemia, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Hypertension
Keywords: Dyslipidemias, Cardiovascular Diseases, Body Mass Index, Antihypertensive Agents, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Lipoprotein(a), Metabolic Syndrome, Ethnic Groups, Waist Circumference, Prediabetic State, Hyperlipidemias, American Heart Association, Public Health, Insulin Resistance, Prospective Studies, Secondary Prevention, Coronary Vessels, Benchmarking, Cost of Illness, Risk Factors, Myocardial Infarction, Atherosclerosis, Coronary Disease, Stroke, Asian Continental Ancestry Group, Risk Assessment, Cardiology, Hypertension, Risk Reduction Behavior, Cholesterol, World Health Organization, Biomarkers, Delivery of Health Care, Triglycerides, Asian Americans, Asia
< Back to Listings