PCI for Multivessel Disease in STEMI
Quick Takes
- Complete revascularization is recommended in patients presenting with an acute ST-segment elevation myocardial infarction (STEMI) without shock.
- In individuals who present in cardiogenic shock during an acute STEMI, revascularization of the culprit vessel only is recommended.
- Fractional flow reserve (FFR) or optical coherence tomography (OCT) evaluation of non-culprit vessels can guide the revascularization strategy.
Introduction
Based on the current body of evidence, recent guidelines recommend complete revascularization for patients presenting with a STEMI who are not in cardiogenic shock.1 However, there are caveats that are discussed in this review. Furthermore, in patients who present in cardiogenic shock during an acute STEMI, revascularization of the culprit vessel only is recommended.
Review of the Literature
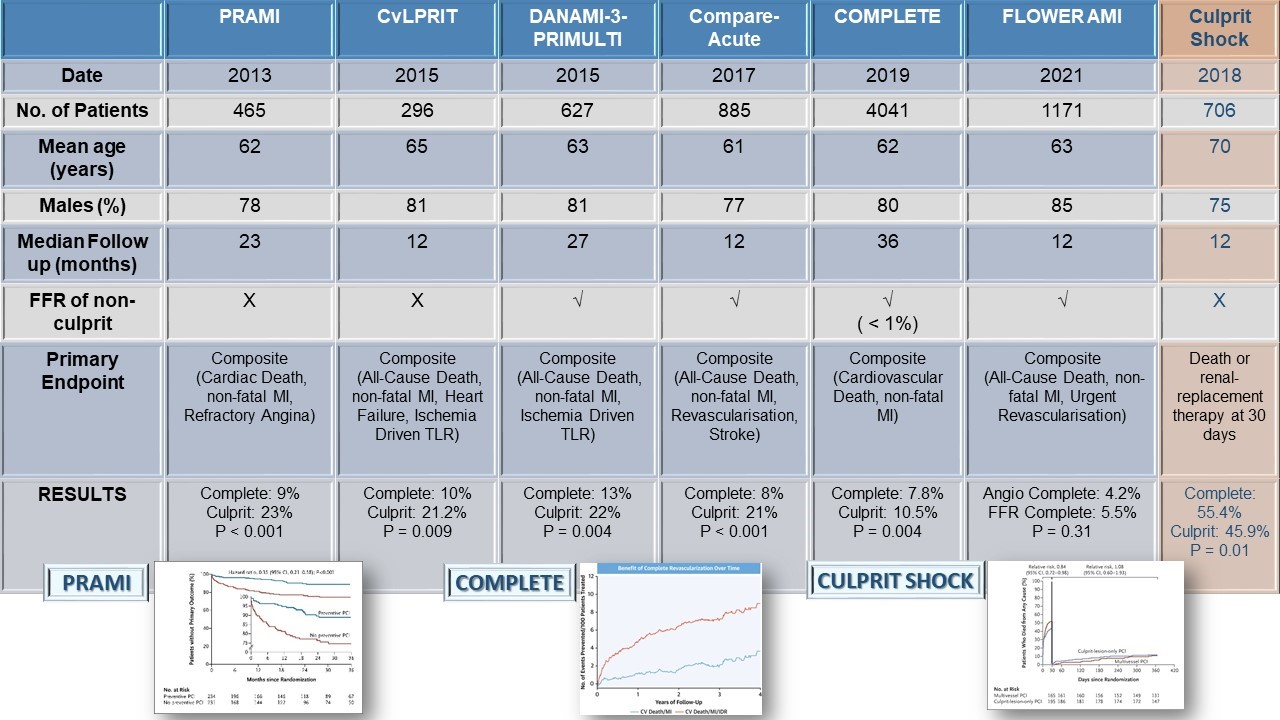
Table 1 summarizes the most relevant randomized clinical trials of culprit-only versus complete revascularization in STEMI. These trials enrolled between 300 to 900 patients. The COMPLETE (Complete Versus Culprit-Only Revascularization Strategies to Treat Multivessel Disease After Early PCI for STEMI) trial is considered the largest of these randomized trials with 4,041 patients. The patient population in these trials was relatively young, with a mean age range of 60-65 years, and a mean follow-up period ranging from 12 to 27 months. However, the COMPLETE trial had an extended follow-up of 36 months. Overall, these trials reported a reduction in the composite endpoint of cardiovascular death, myocardial infarction (MI), or ischemia-driven revascularization (refractory angina).2-6
Table 1: Data From Relevant Randomized Clinical Trials
The argument for complete revascularization could be supported by the OCT substudy of the COMPLETE trial. This substudy demonstrated that obstructive, non-culprit vessel lesions were more frequently characterized by thin cap fibroatheroma and therefore more prone to future events.7
COMPLETE Trial
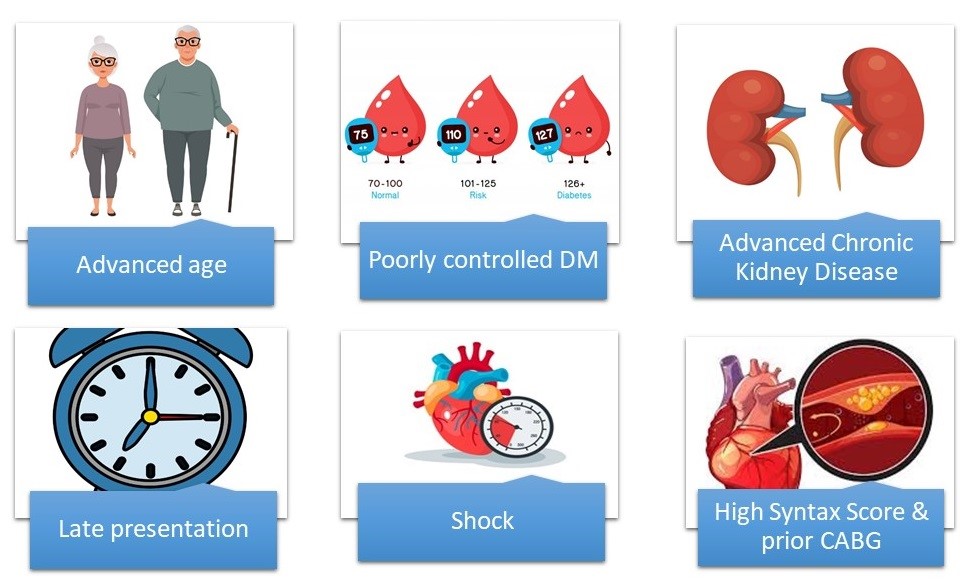
Because the COMPLETE trial is the most contemporary study with the largest enrollment and longest follow-up, it is critical to examine it closely. The patients were relatively young and mostly male (80%) with a low SYNTAX score of 16 who presented early after symptom onset (<6 hours). Those with prior coronary artery bypass grafting (CABG) were excluded. Only 19% of patients had diabetes (mean hemoglobin A1c was 6), and only 2% had significant renal dysfunction. As such, we should be cautious when applying the results to more complex disease (higher SYNTAX score or post-CABG) or higher-risk categories, including patients with advanced chronic kidney disease, elderly patient populations, and patients with poorly controlled diabetes. Despite being a low-risk population with non-complex coronary disease and a normal renal function, there was a trend toward higher incidence of acute kidney injury that did not reach statistical significance (7 in the complete group and 0 in the culprit-only group).6
Of the total patients enrolled in this trial, 303 (3%) underwent a pharmacoinvasive strategy. Dehghani et al. examined this subgroup. This was a prespecified analysis that reported a reduction in major cardiovascular events in patients undergoing an initial pharmacoinvasive strategy similar to those who underwent primary percutaneous coronary revascularization (PCI).8
CULPRIT SHOCK Trial
The 1-year results of the CULPRIT SHOCK (Culprit Lesion Only PCI Versus Multivessel PCI in Cardiogenic Shock) trial were published in 2018.9 A total of 706 patients presenting with STEMI and shock was randomized to culprit lesion only with possible staged revascularization or immediate multivessel revascularization. Of the 301 patients randomized to the culprit-only arm, 43 had immediate multivessel PCI, 13 underwent urgent PCI, 60 underwent staged PCI, and 1 underwent staged CABG. Compared with multivessel PCI, culprit-only PCI was associated with a reduction in all-cause death or renal replacement therapy at 30 days (primary endpoint). This was at the cost of a numerically higher rate of heart failure hospitalizations and more frequent repeat revascularization at 1 year. The rate of the composite of death, recurrent infarction, or rehospitalization for heart failure did not differ significantly between the 2 arms. This persisted to 12 months of follow-up. The mortality benefit noted at 30 days was attenuated over the course of the 1 year.
FFR-Guided Complete Revascularization Trials
Most of the studies evaluating complete revascularization in STEMI were based on angiographic interpretation of lesion severity. Only the Compare-Acute (Fractional Flow Reserve-Guided Multivessel Angioplasty in Myocardial Infarction) trial (n = 885) and DANAMI-3-PRIMULTI (The Third Danish Study of Optimal Acute Treatment of Patients With STEMI: Primary PCI in Multivessel Disease) (n = 627) employed FFR to guide the revascularization strategy. The Compare-Acute trial demonstrated that an FFR-guided strategy reduced the composite primary endpoint of death from any cause, nonfatal MI, revascularization, and cerebrovascular events at 12 months. This was primarily driven by a reduction in revascularization.4 DANAMI-3-PRIMULTI reached the same conclusion.5 As such, an FFR-guided strategy does not necessarily impact hard endpoints such as death and MI but can reduce repeat revascularizations. This may have implications for quality of life and cost.
Contrary to these trials, the more recent FLOWER MI (Flow Evaluation to Guide Revascularization in Multivessel ST-Elevation Myocardial Infarction) trial failed to demonstrate the superiority of an FFR-guided complete revascularization strategy compared with an angiography-guided strategy with respect to repeat revascularization. Consistent with the previously described studies, the primary outcome of all deaths, MI, or unplanned hospitalization leading to urgent revascularization at 12 months was not significantly different between the arms. The power analysis assumed an even rate of 9.5% in the FFR-guided arm and 15% in the angiography-guided arm. The observed event rate in both arms was less than 5%, making the study underpowered to detect a significant difference for the primary endpoint and resulting in a very wide confidence interval.10
With such inconclusive results on the role of physiological assessment of non-culprit vessels in the setting of STEMI, several other studies are underway. The FULL REVASC (FFR-Guidance for Complete Non-Culprit Revascularization) trial is a multicenter, international, registry-based randomized clinical trial designed to evaluate whether a strategy of FFR-guided complete revascularization reduces the combined primary endpoint of total mortality, non-fatal MI, and unplanned revascularization compared to a culprit-only PCI. A total of 1,545 patients was randomized, and enrollment was completed in September 2019. Follow-up is planned for 2.75 years. The results are still pending.11 Other trials addressing the role of instantaneous wave-free ratio (iFR) and OCT in STEMI include the iMODERN (iFR Guided Multi-Vessel Revascularization During Percutaneous Coronary Intervention for Acute Myocardial Infarction) and OCT CONTACT (OCT Guided vs Complete PCI in Patients With ST Segment Elevation Myocardial Infarction and Multivessel Disease) trials, which are ongoing.12-13 The iMODERN trial aims to compare an instantaneous wave-free ratio-guided PCI of non-culprit vessel strategy during the acute intervention with a deferred stress perfusion cardiac magnetic resonance-guided strategy during outpatient follow-up. The follow-up is planned for 6 months, 12 months, 3 years, and 5 years. The OCT CONTACT trial is enrolling patients with STEMI who underwent successful culprit-lesion PCI. Patients will be randomized in a 1:1 fashion to complete angiography-guided PCI versus OCT-guided revascularization of lesions deemed to have high-risk plaque features.
Conclusions
The current body of evidence supports angiography-guided complete revascularization of all obstructive lesions in patients presenting with STEMI, provided that the patients are not in cardiogenic shock at the time of initial presentation. Nevertheless, caution needs to be exercised in patients presenting with more complex coronary anatomy (high SYNTAX scores) and especially in those who have underlying renal dysfunction (Figures 1-2).
An FFR-guided complete revascularization strategy may reduce the need for repeat revascularization and possibly have cost benefits, but it does not reduce the hard endpoints of death and MI. This matter requires further clarification through appropriately powered randomized trials with long-term follow-up.
For patients presenting with STEMI and shock, the current body of evidence supports culprit-only PCI as an initial strategy.
Figure 1: Contributing Factors
Figure 2: Decision Making
References
- Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. EuroIntervention 2019;14:1435-1534.
- Wald DS, Morris JK, Wald NJ, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med 2013;369:1115-23.
- Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol 2015;65:963-72.
- Smits PC, Abdel-Wahab M, Neumann FJ, et al. Fractional Flow Reserve-Guided Multivessel Angioplasty in Myocardial Infarction. N Engl J Med 2017;376:1234-44.
- Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet 2015;386:665-71.
- Mehta SR, Wood DA, Storey RF, et al. Complete Revascularization with Multivessel PCI for Myocardial Infarction. N Engl J Med 2019;381:1411-21.
- Pinilla-Echeverri N, Mehta SR, Wang J, et al. Nonculprit Lesion Plaque Morphology in Patients With ST-Segment-Elevation Myocardial Infarction: Results From the COMPLETE Trial Optical Coherence Tomography Substudys. Circ Cardiovasc Interv 2020;13:e008768.
- Dehghani P, Cantor WJ, Wang J, et al. Complete Revascularization in Patients Undergoing a Pharmacoinvasive Strategy for ST-Segment-Elevation Myocardial Infarction: Insights From the COMPLETE Trial. Circ Cardiovasc Interv 2021;Jul 29:[Epub ahead of print].
- Thiele H, Akin I, Sandri M, et al. One-Year Outcomes after PCI Strategies in Cardiogenic Shock. N Engl J Med 2018;379:1699-1710.
- Puymirat E, Cayla G, Simon T, et al. Multivessel PCI Guided by FFR or Angiography for Myocardial Infarction. N Engl J Med 2021;385:297-308.
- Böhm F, Mogensen B, Östlund O, et al. The FULL REVASC (Ffr-gUidance for compLete non-cuLprit REVASCularization) Registry-based Randomized Clinical Trial. Am Heart J 2021;Jul 23:[Epub ahead of print].
- iFR Guided Multi-vessel Revascularization During Percutaneous Coronary Intervention for Acute Myocardial Infarction (iMODERN) (ClinicalTrials.gov website). October 9, 2020. Available at https://clinicaltrials.gov/ct2/show/NCT03298659. Accessed August 5, 2021.
- OCT Guided vs COmplete Pci in patieNts With sT Segment Elevation myocArdial infarCtion and mulTivessel Disease (OCT-CONTACT) (ClinicalTrials.gov website). May 11, 2021. Available at https://clinicaltrials.gov/ct2/show/NCT04878133. Accessed August 5, 2021.
Clinical Topics: Cardiac Surgery, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Stable Ischemic Heart Disease, Vascular Medicine, Aortic Surgery, Cardiac Surgery and Heart Failure, Cardiac Surgery and SIHD, Acute Heart Failure, Interventions and Imaging, Interventions and Vascular Medicine, Angiography, Nuclear Imaging, Chronic Angina, Acute Coronary Syndromes
Keywords: ST Elevation Myocardial Infarction, Fractional Flow Reserve, Myocardial, Hemoglobin A, Quality of Life, Percutaneous Coronary Intervention, Plaque, Atherosclerotic, Shock, Cardiogenic, Incidence, Outpatients, Confidence Intervals, Follow-Up Studies, Myocardial Infarction, Diabetes Mellitus, Heart Failure, Coronary Artery Bypass, Renal Replacement Therapy, Angioplasty, Acute Kidney Injury, Registries, Renal Insufficiency, Chronic, Hospitalization, Angiography, Magnetic Resonance Spectroscopy, Perfusion
< Back to Listings