Cardiac CT: A New Frontier in Advocating for Women's Cardiovascular Health
Quick Takes
- Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of morbidity and mortality in women.
- Appropriate use of computed tomography (CT) imaging, namely coronary artery calcium (CAC) and coronary CTA (CCTA), enables diagnosis and accurate risk stratification of coronary artery disease in women.
- CT imaging can effectively identify at-risk women, and results can be used to guide targeted treatment and initiation of appropriate preventive therapy, thereby improving long-term risk and cardiac outcomes.
Introduction
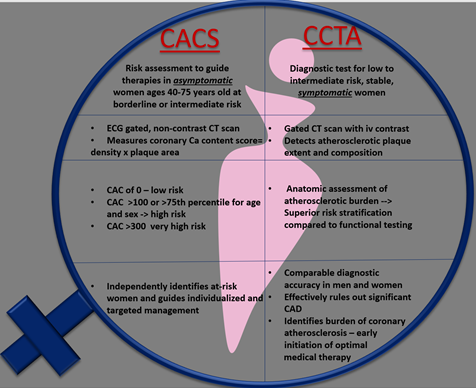
Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of morbidity and mortality in women in the United States and worldwide.1,2 Epidemiologic data suggest a higher acute and long-term case fatality rate for coronary artery disease (CAD) among women when compared with men.3,4 There is increased recognition of sex and gender related disparities in underdiagnoses and under treatment of heart disease in women, leading to worsening clinical outcomes.5,6 Early and accurate risk stratification, combined with targeted treatment, is crucial to manage ASCVD and improve outcomes in women. Cardiac computed tomography (CT) imaging allows for a comprehensive anatomic assessment of CAD and characterization of subclinical coronary atherosclerosis that can identify sex-specific phenotypes of varying cardiovascular risk. Figure 1 discusses the differences between coronary artery calcium (CAC) scoring and coronary CT angiography (CCTA) in the evaluation of CAD. Taken together the use of cardiac CT can help us better diagnose, refine prognosis, and individualize early and appropriate management strategies for CAD in women.
Figure 1
CAC in Asymptomatic Women
CAC is a surrogate marker of burden of sub-clinical coronary atherosclerosis and is a validated predictor for ASCVD risk in asymptomatic individuals. Given that traditional risk calculators such as Framingham Risk Score (FRS) and the Pooled Cohort Equations (PCE) underestimate the CVD risk in women, CAC scoring offers an opportunity for precise cardiovascular risk assessment in asymptomatic women and can guide primary preventive interventions, such as early initiations of statins.
In a large cohort of asymptomatic women, CAC was more effective in identifying high risk women that were previously classified as low risk based on FRS. The 15-year mortality in asymptomatic women with a low to intermediate risk factor burden was 5.0% for those with a CAC score of 0 and 23.5% for those with a CAC score ≥400 (P<0.001).7 Most recently, the CAC consortium of asymptomatic men and women demonstrated similarly low rates of cardiovascular mortality in both sexes when CAC was 0. Of note, women with detectable CAC had a 1.3-fold higher relative hazard for CVD mortality when compared to men from similar CAC groups, (Hazard ratio, [HR] for women vs. men were 2.93 vs. 2.13; 9.72 vs. 4.98; 26.65 vs. 13.32 for CAC 1-100, 101-399, and ≥400, respectively).8 Of note, higher rates of cardiovascular mortality in women as compared to men, were observed with multiple (HR: 8.6 vs. 5.9 for >/= 5 CAC lesions), larger size (HR: 8.5 vs. 4.4 for a lesion size >/= 15 mm3) or more diffuse distribution of CAC lesions (HR: 8.2 vs. 5.1 for multivessel CAC). Plaque density was not predictive of CVD mortality for women but was so for men.8 These findings highlight features of a sex specific atherosclerotic profile that can refine early risk stratification, provide mechanistic correlations to differential cardiovascular outcomes in women, and influence preventive strategies. Prior analysis of the MESA participants, including a sex-specific analysis, suggested that a CAC score ≥100 identifies patients who are most likely to derive net benefit from aspirin for primary prevention of CAD, while in those with CAC=0, aspirin use could result in net harm.9 Overall, in light of the robust evidence in favor of the ability of CAC to accurately characterize risk in women, current expert consensus is to utilize CAC scanning in women with borderline and intermediate risk and in women with sex-specific risk enhancers such as pre-eclampsia and early menopause.
Future research including clinical trials must explore these unique insights to sex-specific differences in coronary atherosclerosis and its impact on prognostication and focused preventive strategies in women.
CCTA in Stable, Symptomatic Chest Pain in Women
CCTA is established as a powerful, non-invasive imaging test that can provide pertinent information regarding anatomic assessment of CAD in various stages, including severity and extent of obstructive and non-obstructive coronary atherosclerosis.10 Data suggest a unique female specific profile of CAD with evidence of non-obstructive coronary atherosclerosis and lower prevalence and extent of obstructive disease, compared to men.11,12 A recent sub-analysis of ISCHEMIA (International Study of Comparative Health Effectiveness With Medical and Invasive Approaches) trial demonstrated that women had more frequent episodes of angina, independent of less severe ischemia and less extent of obstructive disease, than men. Of the participants enrolled in the ISCHEMIA trial with at least moderate ischemia on stress testing, women were more likely to have no obstructive CAD (<50% stenosis in all vessels on CCTA), compared to men (353 of 1022 [34.4%] vs. 378 of 3353 [11.3%]).13
The comparable diagnostic accuracy of CCTA for obstructive CAD in women and men has been established previously in sex-specific analyses of ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) and Multi Center Combined Non-invasive Coronary Angiography and Myocardial Perfusion Imaging Using 320-Detector Computed Tomography (CORE-320) trials.14 The excellent spatial and temporal resolution of CCTA permits high diagnostic accuracy for obstructive disease despite smaller epicardial vessels in women, in comparison with gold standard, invasive coronary angiography (ICA). In comparison, diagnostic accuracy of functional testing in women has been limited by breast attenuation artefacts on nuclear testing, limited windows with stress echo, and a higher likelihood of false positives on exercise treadmill testing.15
Exposure to ionizing radiation, particularly breast tissue in women, has been a common safety concern for use of cardiac CT in women. Advances in technology and acquisition techniques such as prospective electrocardiogram (ECG) triggered scanning, ECG based tube modulation, iterative reconstruction and single heartbeat, high pitch helical scanning, have been shown to significantly reduce radiation doses with CCTA.16 Radiation exposure remains a concern for other imaging modalities including myocardial perfusion imaging with single-photon emission computerized tomography (SPECT) and positron emission tomography (PET). In a subgroup analysis of the PROMISE (Prospective Multicenter Imaging Study for Evaluation of Chest Pain) trial, CTA use was associated with lower radiation dose compared to functional testing, with lower median index test (8.8 vs. 12.6 mSv, p < 0.001) and 90-day cumulative (11.6 vs. 13.1 mSv, p < 0.001) dose, independent of patient characteristics.17 Previous data has suggested that the lifetime attributable risk (LAR) of cancer for a 60-year-old woman is 0.22% after undergoing a CCTA, however contemporary dose reduction techniques are expected to decrease these risk estimates even further and makes it a safer, useful test in women.18
Anatomic assessment of the extent and burden of coronary atherosclerosis by CCTA is shown to have major implications on accurate risk stratification, prognosis, and can guide targeted management, leading to subsequent benefits in clinical outcomes. In a sex-specific analysis of the PROMISE trial, women derived more effective prognostic information from anatomic assessment by CCTA compared to stress testing (exercise electrocardiography, exercise imaging, or pharmacologic imaging), with adjusted HR for major adverse cardiovascular events of 5.9 versus 2.3 respectively, (p=0.028).19 In this context, CCTA as a frontline test in stable symptomatic women can provide enhanced risk stratification, improved diagnostic accuracy, and guide appropriate initiation of evidence based therapies, thereby providing an opportunity to improve clinical outcomes in women.20
Further insights from women-centered clinical studies such as ongoing WARRIOR (Women's Ischemia Trial to Reduce Events In Non-Obstructive CAD) trial will continue to expand our understanding on the complex interplay of sex, coronary anatomy/atherosclerosis by CCTA or ICA, and ischemia in differential risk profiles, clinical presentation and outcomes of CAD in stable, symptomatic women.21
Conclusion
Effective and appropriate use of cardiac CT imaging enables accurate diagnosis and precise risk-stratification of CAD in women. Identification of at-risk women can enable targeted management strategies, including early initiation of appropriate therapy, that can reduce long-term risk and improve cardiovascular outcomes.
References
- Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart Disease and Stroke Statistics-2017 Update: a report from the American Heart Association. Circulation 2017;135:e146-e603.
- Vogel B, Acevedo M, Appelman Y, et al. The Lancet women and cardiovascular disease commission: reducing the global burden by 2030. Lancet 2021;397:2385-2438.
- Wilmot KA, O'Flaherty M, Capewell S, Ford ES, Vaccarino V. Coronary heart disease mortality declines in the United States from 1979 through 2011: evidence for stagnation in young adults, especially women. Circulation 2015;132:997-1002.
- Mehta LS, Beckie TM, DeVon HA, et al. Acute myocardial infarction in women: a scientific statement from the American Heart Association. Circulation 2016;133:916-47.
- Blomkalns AL, Chen AY, Hochman JS, et al. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol 2005;45:832-37.
- Bairey Merz CN, Shaw LJ, Reis SE, et al. Insights from the NHLBI-sponsored Women's Ischemia Syndrome Evaluation (WISE) study: Part II: gender differences in presentation, diagnosis, and outcome with regard to gender-based pathophysiology of atherosclerosis and macrovascular and microvascular coronary disease. J Am Coll Cardiol 2006;47:S21-29.
- Kelkar AA, Schultz WM, Khosa F, et al. Long-term prognosis after coronary artery calcium scoring among low-intermediate risk women and men. Circ Cardiovasc Imaging 2016;9:e003742.
- Shaw LJ, Min JK, Nasir K, et al. Sex differences in calcified plaque and long-term cardiovascular mortality: observations from the CAC Consortium. Eur Heart J 2018;39:3727-35.
- Miedema MD, Duprez DA, Misialek JR, et al. Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes 2014;7:453-60.
- Truong QA, Rinehart S, Abbara S, et al. Coronary computed tomographic imaging in women: an expert consensus statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr 2018;12:451-66.
- Shaw LJ, Shaw RE, Bairey Merz CN, et al. Impact of ethnicity and gender differences on angiographic coronary artery disease prevalence and in-hospital mortality in the American College of Cardiology-National Cardiovascular Data Registry. Circulation 2008;117:1787-801.
- Khuddus MA, Pepine CJ, Handberg EM, et al. An intravascular ultrasound analysis in women experiencing chest pain in the absence of obstructive coronary artery disease: a substudy from the National Heart, Lung and Blood Institute-Sponsored Women's Ischemia Syndrome Evaluation (WISE). J Interv Cardiol 2010;23:511-19.
- Reynolds HR, Shaw LJ, Min JK, et al. Association of sex with severity of coronary artery disease, ischemia, and symptom burden in patients with moderate or severe ischemia: secondary analysis of the ISCHEMIA randomized clinical trial. JAMA Cardiol 2020;5:773-86.
- Jug B, Gupta M, Papazian J, et al. Diagnostic performance of 64-slice multidetector coronary computed tomographic angiography in women. J Nucl Cardiol 2012;19:1154-61.
- Nguyen PK, Nag D and Wu JC. Sex differences in the diagnostic evaluation of coronary artery disease. J Nucl Cardiol 2011;18:144-52.
- Chinnaiyan KM, Boura JA, DePetris A, et al. Progressive radiation dose reduction from coronary computed tomography angiography in a statewide collaborative quality improvement program: results from the Advanced Cardiovascular Imaging Consortium. Circ Cardiovasc Imaging 2013;6:646-54.
- Lu MT, Douglas PS, Udelson JE, et al. Safety of coronary CT angiography and functional testing for stable chest pain in the PROMISE trial: a randomized comparison of test complications, incidental findings, and radiation dose. J Cardiovasc Comput Tomogr 2017;11:373-82.
- Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 2007;298:317-23.
- Pagidipati NJ, Hemal K, Coles A, et al. Sex differences in functional and CT angiography testing in patients with suspected coronary artery disease. J Am Coll Cardiol 2016;67:2607-16.
- Newby DE, Adamson PD, Berry C, et al. Coronary CT angiography and 5-year risk of myocardial infarction. N Engl J Med 2018;379:924-33.
- Lakshmanan S, Wei J, Cook-Wiens G, et al. Comparison of risk profiles of women with Inoca diagnosed by coronary computed tomography angiography vs invasive coronary angiography - a substudy of the women's ischemia trial to reduce events in non-obstructive coronary artery disease (WARRIOR). J Am Coll Cardiol 2021;77:1357-57.
Clinical Topics: Cardiovascular Care Team, Dyslipidemia, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Prevention, Atherosclerotic Disease (CAD/PAD), Nonstatins, Novel Agents, Statins, Interventions and Coronary Artery Disease, Interventions and Imaging, Angiography, Computed Tomography, Nuclear Imaging
Keywords: Primary Prevention, Coronary Artery Disease, Computed Tomography Angiography, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Cardiovascular Diseases, Calcium, Coronary Angiography, Myocardial Perfusion Imaging, Aspirin, Heart Rate, Constriction, Pathologic, Pre-Eclampsia, Prospective Studies, Drug Tapering, Risk Factors, Tomography, X-Ray Computed, Electrocardiography, Atherosclerosis, Tomography, Emission-Computed, Single-Photon, Positron-Emission Tomography, Radiation Exposure, Biomarkers, Radiation, Ionizing, Radiation Dosage, Ischemia, Risk Assessment, Heart Disease Risk Factors, Menopause, Phenotype, Reference Standards, Breast Neoplasms
< Back to Listings