Quantifying and Understanding the Higher Risk of ASCVD Among South Asians
Quick Takes
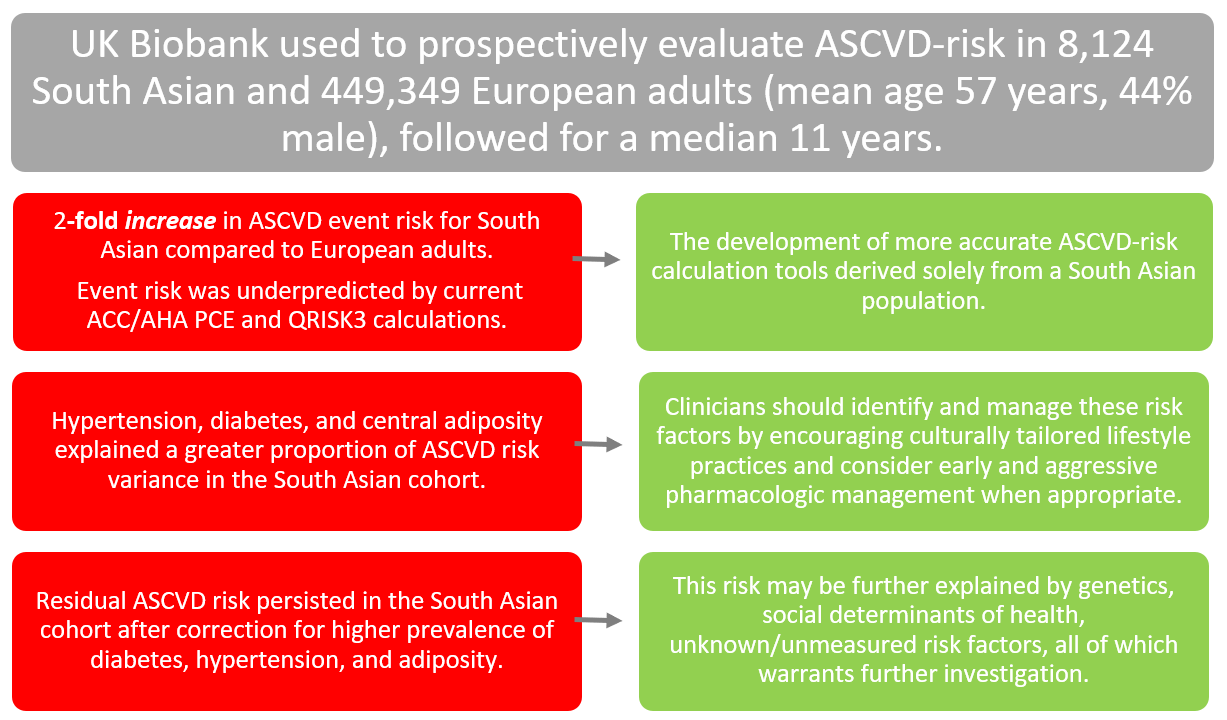
- Individuals of South Asian ancestry have about a two-fold increased risk of ASCVD events compared to adults of European ancestry.
- This observed increase in risk is not reflected by available prediction algorithms such as Pooled Cohort Equations (PCE) or QRISK3 estimators.
- Despite correcting for a higher prevalence of diabetes, hypertension, and central adiposity in South Asians, residual cardiovascular risk persisted and may be explained by differences in social determinants of health, genetic causes, or other yet unidentified factors.
Commentary based on Patel AP, Wang M, Kartoun U, Ng K, Khera AV. Quantifying and understanding the higher risk of atherosclerotic cardiovascular disease among South Asian individuals: results from the UK Biobank Prospective Cohort Study. Circulation 2021;Aug 10:[Epub ahead of print].1
South Asian (SA) individuals are a high risk group for atherosclerotic cardiovascular disease (ASCVD), and recent practice guidelines in the United States (US), Canada, and Europe have modified screening recommendations and risk estimates for this population.2,3 Prior investigations have shown that SA adults experience a 1.7- to 4-fold higher ASCVD risk; these findings have major public health implications.4-8 However, these studies have been limited by relatively small sample sizes, study type (case-control or retrospective), use of aggregated SA data, unreliable death registries, and lack of uniform risk factor assessment.
In addition, many were carried out prior to the introduction of contemporary preventive therapies. In their recent study in Circulation, Patel et al. addressed the following areas of ambiguity for SA compared to adults of European ancestry:1
- Confirm the magnitude of increased ASCVD risk experienced by SA in the context of contemporary clinical care.
- Whether the observed risk varies with sex, ethnic subgroup, or immigration pattern.
- Whether the observed risk is attenuated by adjustment for biological factors, comorbidities, lifestyle, and psychosocial factors.
- Whether the observed risk is attributable to various traditional and non-traditional risk factors.
There were 8,124 middle-aged individuals of SA ancestry and 449,349 middle-aged individuals of European ancestry enrolled from the modern United Kingdom (UK) Biobank prospective cohort study (individuals between 40-69 years of age between 2006 and 2010). The study group had a mean age of 57 years and 44% were male at enrollment. Individuals with a history of ASCVD diagnosed before enrollment were excluded. Participants were assessed for a myriad of ASCVD mediators including social, clinical, anthropometric, and lifestyle factors using a detailed survey. The median follow-up of the study was 11 years.
The results of the study corresponding with each study aim are discussed (Figure 1):
Figure 1
(1) Over the study period, 554 of 8,124 (6.8%) SA and 19,756 of 449,349 (4.4%) individuals of European ancestry experienced an ASCVD event (HR, 95%CI): 2.03 (1.86-2.22; P<0.001). In contrast to the significant difference of ASCVD events between the two groups observed in the study, current tools to estimate the 10-year risk of incident ASCVD predict no significant difference in risk between individuals of SA and European ancestry. The pooled cohort equations (PCE) predicted median risks of 4.8% and 6.0%, and the QRISK3 score predicted 9.7% and 8.3% for individuals of SA and European ancestry, respectively.9-11 After adjusting for baseline differences in age and sex between the two groups, the PCE predicted only 1.1-fold higher risk for SA, and QRISK3 predicted only 1.4-fold higher risk for SA.
(2) The higher risk of ASCVD in individuals of SA ancestry compared to those of European ancestry observed in the study was preserved when participants were stratified by sex, age, and whether they were born in the UK. There was no significant difference for men (2.06, 1.87-2.2; P<0.001) and women (1.92, 1.62-2.28; P<0.001). Those of Bangladeshi origin had the highest risk of an ASCVD event (3.66, 2.38-5.62, P<0.001), followed by Pakistani (2.45, 2.06-2.91; P<0.001).
(3) There was no significant difference in relative risk of ASCVD associated with many biological factors, comorbidities, lifestyle, and psychosocial factors between those of SA and European origin. Notable significant differences included ASCVD risk being higher with each 20-mmHg rise in systolic blood pressure in SA (HR, 95% CI: 1.33, 1.21-1.45) than European origin (1.12, 1.11-1.13) with a P for heterogeneity of <0.001. For obesity, a lower ASCVD risk was observed in SA compared to European (P for heterogeneity of 0.035). Similar results were seen for current smoking status (P for heterogeneity of 0.002).
(4) A greater proportion of variance in ASCVD risk was explained by hypertension, diabetes, and central adiposity in SA compared to European adults.
The study by Patel et al. is timely and provides insight into risk factors that mediate increased ASCVD risk in individuals of SA ancestry and provides a rationale for the focusing of treatment efforts on specific risk factors. The observed cardiovascular events did not reflect that which was predicted by the PCE.
The PCE is known to underestimate risk in SA (not unexpected given the model was derived from studies without representation from an SA population), but has also been shown to overestimate risk in disaggregated SA subgroups, or when considering a coronary artery calcium score.10,12,13 The QRISK3 calculation (which was derived using <2% SA adults) uses a multiplicative factor from 1.3 to 1.7 to account for country of SA ancestry; these corrective factors fell short of the actual risk observed in the study.9
Further study and subsequent development of prediction tools that more accurately reflect observed risk of ASCVD in SA individuals is important, and will only be achieved if derived from an all SA cohort, such as that offered by the MASALA study.14 Fortunately, practice guidelines in the US, Canada, and Europe have accounted for the increased ASCVD risk in SA individuals despite suboptimal PCE, Framingham risk score (FRS), and QRISK3 predictive tools, respectively; studies to better understand this higher risk will allow for more precise and effective medical management.
This study continues to amplify available literature showing an increased risk of ASCVD in those of SA descent and the importance of early and continued, culturally tailored, counseling with respect to primary prevention measures. While novel genetic causes may account for the imbalance of ASCVD between SA and European cohorts, this study suggests that the observed disparity is likely related to excess rates of hypertension, diabetes, and central obesity in SA adults.15-17 Clinicians should advocate for aggressive lifestyle modification in addition to a lower threshold for instituting pharmacologic therapy for blood pressure18 and diabetes19 as well as the selective use coronary artery calcium to improve risk stratification methods to guide statin and possibly aspirin therapy.20,21
References
- Patel AP, Wang M, Kartoun U, Ng K, Khera AV. Quantifying and understanding the higher risk of atherosclerotic cardiovascular disease among South Asian individuals: results from the UK Biobank Prospective Cohort Study. Circulation 2021;144:410-22.
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/ PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;73:3168-3209.
- Anderson TJ, Grégoire J, Pearson GJ, et al. 2016 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in the adult. Can J Cardiol 2016;32:1263–82.
- Forouhi NG, Sattar N, Tillin T, McKeigue PM, Chaturvedi N. Do known risk factors explain the higher coronary heart disease mortality in South Asian compared with European men? Prospective follow-up of the Southall and Brent studies, UK. Diabetologia 2006;49:2580–88.
- Tillin T, Hughes AD, Mayet J, et al. The relationship between metabolic risk factors and incident cardiovascular disease in Europeans, South Asians, and African Caribbeans: SABRE (Southall and Brent Revisited): a prospective population-based study. J Am Coll Cardiol 2013;61:1777–86.
- Hajra A, Li Y, Siu S, et al. Risk of coronary disease in the South Asian American population. J Am Coll Cardiol 2013;62:644–45.
- Klatsky AL, Tekawa I, Armstrong MA, Sidney S. The risk of hospitalization for ischemic heart disease among Asian Americans in Northern California. Am J Public Health 1994;84:1672–75.
- Lee J, Heng D, Chia KS, Chew SK, Tan BY, Hughes K. Risk factors and incident coronary heart disease in Chinese, Malay and Asian Indian males: the Singapore Cardiovascular Cohort Study. Int J Epidemiol 2001;30:983–88.
- Hippisley-Cox J, Coupland C, Brindle P. Development and validation of QRISK3 risk prediction algorithms to estimate future risk of cardiovascular disease: prospective cohort study. BMJ 2017;357:j2099.
- Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:2935-59.
- Li Y, Sperrin M, van Staa TP. QRISK3: 10-Year Cardiovascular Disease Risk Calculator (QRISK3 2017). 2019. Available at: https://CRAN.R-project.org/package=QRISK3. Accessed 07/27/2021.
- Al Rifai M, Cainzos-Achirica M, Kanaya AM, et al. Discordance between 10-year cardiovascular risk estimates using the ACC/AHA 2013 estimator and coronary artery calcium in individuals from 5 racial/ethnic groups: comparing MASALA and MESA. Atherosclerosis 2018;279:122-29.
- Rodriguez F, Chung S, Blum MR, Coulet A, Basu S, Palaniappan LP. Atherosclerotic cardiovascular disease risk prediction in disaggregated Asian and Hispanic subgroups using electronic health records. J Am Heart Assoc 2019;8:e011874.
- Kanaya AM, Kandula N, Herrington D, et al. Mediators of atherosclerosis in South Asians living in America (MASALA) study: objectives, methods, and cohort description. Clin Cardiol 2013;36:713-20.
- Kalra D, Vijayaraghavan K, Sikand G, et al. Prevention of atherosclerotic cardiovascular disease in South Asians in the US: a clinical perspective from the National Lipid Association. J Clin Lipidol 2021;15:402-22.
- Joshi P, Islam S, Pais P, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA 2007;297:286-94.
- Koirala B, Turkson-Ocran RA, Baptiste D, et al. Heterogeneity of cardiovascular disease risk factors among Asian immigrants: insights from the 2010 to 2018 National Health Interview Survey. J Am Heart Assoc 2021;10:e020408.
- Patel J, Mehta A, Al Rifai MA, et al. Hypertension guidelines and coronary artery calcification among South Asians: results from MASALA and MESA. Am J Prev Cardiol 2021;6:100158.
- Gujral UP, Narayan KMV, Kandula NR, Liu K, Kanaya AM. Incidence of diabetes and prediabetes and predictors of glycemic change among South Asians in the USA: the MASALA study. BMJ Open Diabetes Res Care 2020;8:e001063.
- Al Rifai M, Cainzos-Achirica M, Kanaya AM, et al. Discordance between 10-year cardiovascular risk estimates using the ACC/AHA 2013 estimator and coronary artery calcium in individuals from 5 racial/ethnic groups: comparing MASALA and MESA. Atherosclerosis 2018;279:122-29.
- Patel J, Pallazola VA, Dudum R, et al. Assessment of coronary artery calcium scoring to guide statin therapy allocation according to risk-enhancing factors: the Multi-Ethnic Study of Atherosclerosis. JAMA Cardiol 2021;Jul 14:[Epub ahead of print].
Clinical Topics: Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Nonstatins, Novel Agents, Statins, Hypertension, Smoking
Keywords: Hydroxymethylglutaryl-CoA Reductase Inhibitors, Calcium, Retrospective Studies, Blood Pressure, Emigration and Immigration, Obesity, Abdominal, Coronary Vessels, Cardiovascular Diseases, Public Health, Biological Factors, Prospective Studies, Adiposity, Biological Specimen Banks, Follow-Up Studies, Diabetes Mellitus, Life Style, Risk Factors, Primary Prevention, Hypertension, Counseling, Registries, Surveys and Questionnaires, Risk Assessment, Aspirin, Smoking, Asian Continental Ancestry Group
< Back to Listings