Expert Opinion: The Value Placed on Prevention versus the Impact of Prevention
Benjamin Franklin's famous quote, "an ounce of prevention is worth a pound of cure" was first used by the historical figure in 1735 with reference to Philadelphia's fire hazard and prevention practices. And over the years, it has been extrapolated to many different contexts, including management of chronic disease. Although we have all heard the expression, however, it isn't clear whether it still rings true in the way we practice modern medicine and the way we place value on what we do…with undue emphasis and importance placed on complex treatments and procedural interventions at the cost of undervaluing preventive measures.
As a preventive cardiologist, I was most drawn to the field by the impact my interventions could make, compared head-to-head with many of the treatments we deliver in cardiology. For example, spending 10 minutes counseling each of my patients about weight loss, healthier dietary and nutritional choices, incorporating more exercise, smoking cessation, or alcohol in moderation could result in preventing the morbidity and mortality from heart failure, stroke or myocardial infarctions for decades to come. On the other hand, spending 30 minutes placing an intracoronary stent may minimize the fallout from the acute coronary syndrome but is unlikely to have the same impact on disease modification that a preventive intervention may have had. It is the proverbial train on a track analogy – changing its trajectory just slightly today could result in a whole different destination for that train in 5-10 years. It's the "proactive" approach to medicine rather than the "reactive" approach.
The American Heart Association estimates that 80% of heart attacks and strokes are preventable1 and yet the burden of heart disease remains high, being the number one killer of men and women in the United States and worldwide. So where is the disconnect?
Certainly, we can attribute some of this ongoing disease burden to individual choices made by our patients. However, the medical system, which operates already on the brink of its capacity, should also be held accountable to some extent. As health systems and as clinicians, we are financially rewarded for ordering expensive tests and invasive procedures at the cost of time spent counseling and educating our patients on "nutritional prescriptions" or weight loss strategies. The work "relative value unit" (wRVU) for a 3-10-minute smoking cessation session is 0.24. Now compare this to the wRVUs for stenting of a coronary artery at 11.21. Does this mean that putting a stent in is considered approximately 47 times more valuable than spending time educating and encouraging a patient to stop smoking?
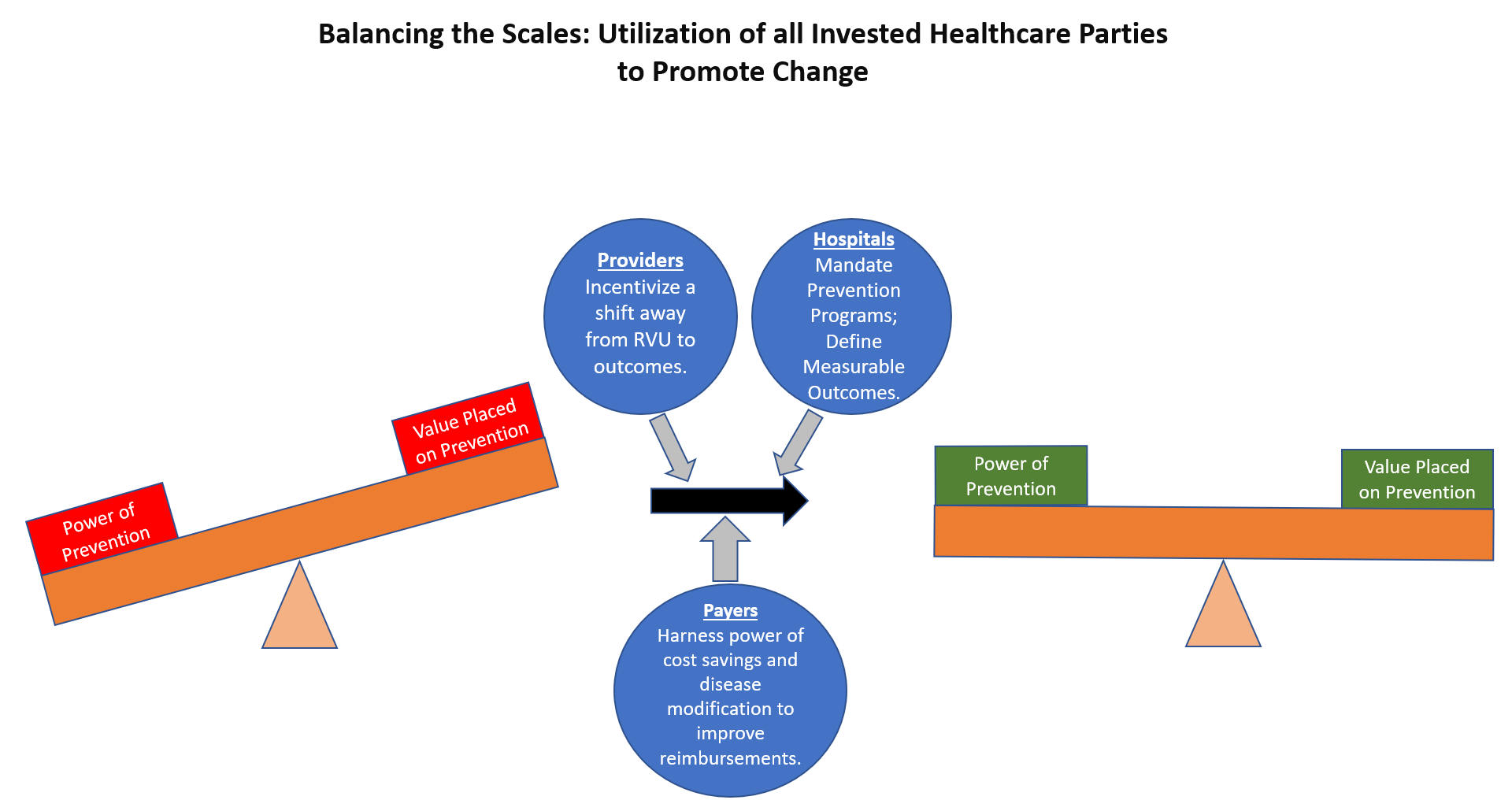
Granted, the "risk" and the skill associated with the coronary intervention is higher than that associated with smoking cessation. But the bottom line remains – that the system is fundamentally flawed in the way in which it incentivizes, reimburses and rewards clinicians for spending time on prevention. The impact that prevention can make on disease morbidity and on disease progression is simply not captured using the RVU system, which is the only currency that appears to be relevant to payers, hospitals, and providers alike.
Healthcare payers and insurance companies are certainly incentivized by preventive measures because it reduces their costs. But it isn't always clear that hospitals are incentivized in the same way. After all, keeping patients out of the hospital doesn't offer the same type of financial incentive for a hospital system, does it -- because they are in the business of treating disease and not preventing it?
The COVID pandemic and the importance of prevention of disease are perhaps the ultimate examples of the true impact of a good preventive intervention as compared with treatment and disease management. However, even there, have we added a current procedural terminology (CPT®) code for COVID vaccine counseling? During every visit in my office with patients who have not received a COVID vaccine, I take the last 5 minutes to discuss their concerns, answer questions and try to help them understand the benefits of the vaccine. Yet this is not recognized or rewarded in the same way that ordering an echo or a stress test may be. There is no RVU for my time, so in a perverse way, focusing on prevention is actually coming at a financial cost for my practice. For providers who are already stretched so thin, layering on more and more expectations that they will "make time" for prevention counseling and interventions on top of their history, physical exam, charting, medication reconciliation, order placement, after-visit summary and billing is nothing short of a fool's paradise.
The challenge also remains as to how to measure the impact of a preventive intervention. With a stent or an ablation, the outcome or goal of the procedure is clear and easily measurable. However, with a preventive intervention such as weight loss, the outcomes to measure and quantify on a population level for the purposes of assigning value remain much more nebulous. Using systems such as the merit-based incentive payments certainly start to assign value to quality rather than quantity, but substantial gaps remain in the implementation and delivery.
Whether it applies to fire safety or to management of chronic disease, the impact and value of prevention has been obvious for hundreds of years. The gap remains in now helping the medical system to empower and reward clinicians for emphasizing prevention in each and every visit, perhaps even more so than ordering costly diagnostic testing and interventional procedures, so that the value placed on prevention becomes aligned with the impact of this powerful intervention.
Figure 1. Courtesy of Kohli P.
References
- CDC Prevention Programs (Heart.org). 2018. Available at: https://www.heart.org/en/get-involved/advocate/federal-priorities/cdc-prevention-programs. Accessed 08/01/2021.
Clinical Topics: Acute Coronary Syndromes, Cardiovascular Care Team, COVID-19 Hub, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Prevention, Acute Heart Failure, Interventions and ACS, Smoking
Keywords: Primary Prevention, Current Procedural Terminology, Motivation, COVID-19 Vaccines, COVID-19, Smoking Cessation, American Heart Association, Exercise Test, Acute Coronary Syndrome, Cardiologists, Coronary Vessels, Weight Loss, Medication Reconciliation, Pandemics, Cost of Illness, Goals, Counseling, Heart Failure, Myocardial Infarction, Cardiology, Morbidity, Smoking, Chronic Disease, Delivery of Health Care, Physical Examination, Disease Progression, Disease Progression, Stroke, Hospitals, Prescriptions, Stents, Disease Management, Insurance
< Back to Listings