What Are the Determinants of Cardiovascular Disease Risk Equivalents Among Adults with Diabetes Mellitus?
Quick Takes
- In this study presence of diabetes was found to be a CVD risk equivalent in one-fifth of CVD-free adults living with diabetes.
- For patients with diabetes without prior CVD, there is higher associated relative CVD risk among women, patients of younger age, White race, elevated CRP or triglyceride levels, or decreased kidney function.
- The current ACC/AHA guidelines accordingly recommend high intensity statin use among those with diabetes only when 10-yr risk ≥20% as compared to moderate intensity statins for everyone else with diabetes.
Commentary based on Zhao Y, Malik S, Budoff MJ, et al. Identification and predictors for cardiovascular disease risk equivalents among adults with diabetes mellitus. Diabetes Care 2021;Aug 11:[Epub ahead of print].1
Diabetes mellitus (DM) is a well-known risk factor for cardiovascular disease (CVD) and atherosclerotic cardiovascular disease (ASCVD) development. However, the magnitude and clinical implications of such risk are not uniform across all patients with diabetes.2 Although diabetes has been previously shown as a coronary heart disease risk equivalent,3 subsequent meta-analyses and studies demonstrated that presence of diabetes and prior coronary heart disease are not necessarily risk equivalent for future coronary heart disease events.4-6 Reasons can be complex and multifactorial. First, interplay between patient and disease factors augments future CVD event occurrence. These may include patient age, race, socioeconomic status, and gender; diabetes duration, severity, and cardiometabolic comorbidities. Further, although previous studies included myocardial infarction (MI) in measured endpoints, peripheral vascular disease (PVD) and stroke were usually not accounted for as part of "CVD" or "ASCVD".3,4,7,8 Lastly, there is a paucity of data regarding ethnically diverse populations, women, and younger patients.2,9,10
In their recent study in Diabetes Care, Zhao et al. addressed this gap in knowledge of diabetes-associated CVD risk. Pooling data from four diverse prospective cohort studies (the Atherosclerosis Risk in Communities [ARIC] Study, Multi-Ethnic Study of Atherosclerosis [MESA], Jackson Heart Study [JHS], Framingham Heart Study [FHS]), they examined factors influencing CVD risk among patients with diabetes and without prior CVD (DM+/CVD-) compared to patients with CVD and without diabetes (DM-/CVD+). Additionally, the investigators used the identified factors to develop an algorithm defining CVD risk equivalent diabetes. The primary composite endpoint was CVD, including MI, cardiac revascularization, stroke, PVD, or heart failure. The secondary endpoint encompassed ASCVD events (MI, stroke, CVD death).1
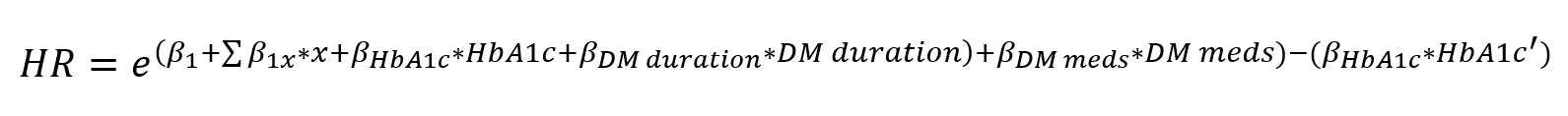
The investigators developed the algorithm below to describe CVD risk equivalence among DM+/CVD- individuals:
HR=e(β1+Σβ1x*x+βHbA1c*HbA1c+β(DM duration*DM duration)+βDM meds*DM meds)-(βHbA1c*HbA1c')
β1 = beta coefficient for DM+/CVD- variable
β1x = statistically significant interaction of DM+/CVD- variable and other variables X in the model
X = subject's actual CVD risk factor value(s)
HbA1c' = 6.5% if subject's HbA1c ≥6.5%; or actual value if subject's HbA1c <6.5
For each study participant, investigators calculated the hazard ratios (HRs) and relative risk between DM+/CVD- versus DM-/CVD+ and then compared the HR to 1. The referent group was DM-/CVD. After applying the equation, those with HR ≥1 were classified as having CVD risk equivalent diabetes.1
There were 27,730 individuals included in the study: 14,331 were from the ARIC cohort and remaining were from the other three cohorts. In total, 3,751 patients had DM+/CVD-, 2,463 had DM-/CVD+, and 1,119 had DM+/CVD+. Compared to those with DM+/CVD-, patients classified as DM+/CVD- were more likely men, White, older, smokers, alcohol drinkers, had family history of CVD, left ventricular hypertrophy, atrial fibrillation, and higher low density lipoprotein cholesterol (LDL-C) and serum creatinine. The median follow-up time was 14.0 years, during which DM-/CVD-, DM+/CVD-, DM-/CVD+, and DM+/CVD+ groups experienced 5,163 (25.3%), 1,576 (42.0%), 1,396 (56.7%), and 768 (68.6%) CVD events and 2,332 (11.4%), 863 (23.0%), 883 (35.9%), and 553 (49.4%) ASCVD events, respectively. The corresponding CVD event rates per 1,000 person years for DM-/CVD-, DM+/CVD-, DM-/CVD+, and DM+/CVD+ groups were 16.5, 33.4, 43.2, and 71.4, respectively. Using DM-/CVD- as the referent group, the unadjusted HR rates for CVD events for individuals with DM+/CVD-, DM-/CVD+, and DM+/CVD+ were 2.22 (95% confidence interval [CI]: 2.10–2.35), 2.93 (95% CI: 2.76–3.11), 5.13 (95% CI: 4.75–5.53), respectively. Compared to DM-/CVD+ patients, those with DM+/CVD- faced both lower CVD (HR: 0.86, 95% CI: 0.80–0.93) and ASCVD risk (HR: 0.76, 95% CI: 0.69–0.84). However, compared to those with DM-/CVD+, DM+/CVD- patients have a higher associated CVD risk if they had a ≥10-year duration of diabetes (20% higher CVD risk) or hemoglobin A1c (HbA1c) ≥9% (35% higher CVD risk). Similar associated CVD risk was noted among those with HbA1c 7%-8%.1
Subgroup analysis evaluated cardiovascular risk factors of DM+/CVD- versus DM-/CVD+ individuals. There was similar associated CVD risk between the two groups (HR close to 1.0 with non-significant p-values) among women, Whites, younger age (<55 years), hs-C-reactive protein (CRP) ≥2 mg/dL, triglycerides ≥2.26 mmol/L, or estimated glomerular filtration rate (eGFR) <60 mL/min/1.73m2. Among patients with DM+/CVD-, lower risk was observed for men, non-White race, older age (>55 years), hs-CRP <2 mg/dL, triglycerides <2.26 mmol/L, or eGFR >60 mL/min/1.73m2. Unadjusted subgroup analysis results were consistent with primary analysis observations.1
Of the 3,751 DM+/CVD- individuals, approximately 19.1% had CVD equivalent diabetes. However, their calculated mean 10-year pooled cohort equations (PCE) risk was 19.3%, falling short of the 20% threshold for the PCE high risk category. Among those with non-CVD risk equivalent diabetes, the mean PCE risk was 21.6% (p=0.0002). Presence of CVD risk equivalent diabetes was associated with higher event rates per 1,000 person-years when compared to non-CVD risk equivalent diabetes (CVD: 53.8 vs. 29.2; ASCVD: 27.7 vs. 14.1). Overall, DM+/CVD- patients experienced 14% lower CVD and 24% lower ASCVD risk than DM-/CVD+ patients.1 The current American College of Cardiology (ACC)/American Heart Association (AHA) guidelines now accordingly recommend intensifying treatment to high intensity statins among those with diabetes only when 10-yr risk ≥20% as compared to moderate intensity statin for everyone with diabetes.11
The study by Zhao et al. is timely and offers insight into risk factors that mediate future CVD event predictability among patients with diabetes. Comparison between DM+/CVD- and DM-/CVD+ groups show that a multitude of disease factors contribute to the heterogeneity of CVD risk conferred by diabetes, such as diabetes duration, control, and treatment status. Certain patient characteristics may also augment that risk, as similar CVD risk between DM+/CVD- and DM-/CVD+ were noted among women, Whites, patients aged <55 years, hs-CRP ≥2 mg/dL, triglycerides ≥2.26 mmol/L, and eGFR <60 mL/min/1.73m2.
This study adds to available literature that diabetes alone does not equate to CVD risk equivalence.2,4,6 In addition, since baseline data from these study cohorts were obtained at least two decades ago, more aggressive efforts and pharmacological advancements in recent years to treat patients with diabetes may have further mitigated risk due to diabetes as CVD equivalent. Moreover, primary prevention with aggressive lifestyle modification and treatment with aspirin and high-intensity statins in higher risk patients with diabetes becomes particularly important in saving disability-adjusted life years and potential healthcare burden.
References
- Zhao Y, Malik S, Budoff MJ, et al. Identification and predictors for cardiovascular disease risk equivalents among adults with diabetes mellitus. Diabetes Care 2021;Aug 11:[Epub ahead of print].
- Rana JS, Blankstein R. Are all individuals with diabetes equal, or some more equal than others? JACC Cardiovasc Imaging 2016;9:1289–91.
- Haffner SM, Lehto S, Rönnemaa T, Pyörälä K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 1998;339:229–34.
- Bulugahapitiya U, Siyambalapitiya S, Sithole J, Idris I. Is diabetes a coronary risk equivalent? Systematic review and meta-analysis. Diabet Med 2009;26:142–48.
- Pajunen P, Koukkunen H, Ketonen M, et al. Myocardial infarction in diabetic and non-diabetic persons with and without prior myocardial infarction: the FINAMI Study. Diabetologia 2005;48:2519–24.
- Rana JS, Liu JY, Moffet HH, Jaffe M, Karter AJ. Diabetes and prior coronary heart disease are not necessarily risk equivalent for future coronary heart disease events. J Gen Intern Med 2016;31:387–93.
- Schramm TK, Gislason GH, Køber L, et al. Diabetes patients requiring glucose-lowering therapy and nondiabetics with a prior myocardial infarction carry the same cardiovascular risk: a population study of 3.3 million people. Circulation 2008;117:1945–54.
- Lee CD, Folsom AR, Pankow JS, Brancati FL. Cardiovascular events in diabetic and nondiabetic adults with or without history of myocardial infarction. Circulation 2004;109:855–60.
- Wannamethee SG, Shaper AG, Whincup PH, Lennon L, Sattar N. Impact of diabetes on cardiovascular disease risk and all-cause mortality in older men: influence of age at onset, diabetes duration, and established and novel risk factors. Arch Intern Med 2011;171:404–10.
- Whiteley L, Padmanabhan S, Hole D, Isles C. Should diabetes be considered a coronary heart disease risk equivalent?: results from 25 years of follow-up in the Renfrew and Paisley survey. Diabetes Care 2005;28:1588–93.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2019;74:1376–414.
Clinical Topics: Arrhythmias and Clinical EP, Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Heart Failure and Cardiomyopathies, Prevention, Atherosclerotic Disease (CAD/PAD), Atrial Fibrillation/Supraventricular Arrhythmias, Hypertriglyceridemia, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Acute Heart Failure, Heart Failure and Cardiac Biomarkers
Keywords: Cardiovascular Diseases, Prospective Studies, Heart Failure, Risk Factors, Atherosclerosis, Myocardial Infarction, Coronary Disease, Stroke, Peripheral Vascular Diseases, Social Class, Algorithms, Longitudinal Studies, Glycated Hemoglobin A, Cholesterol, LDL, Hydroxymethylglutaryl-CoA Reductase Inhibitors, C-Reactive Protein, Creatinine, American Heart Association, American Heart Association, Glomerular Filtration Rate, Triglycerides, Aspirin, Atrial Fibrillation, Quality-Adjusted Life Years, Hypertrophy, Left Ventricular, Confidence Intervals, Follow-Up Studies, Diabetes Mellitus, Life Style, Primary Prevention, Cardiology, Delivery of Health Care, Heart Disease Risk Factors
< Back to Listings