Remaining Inadequacy of Diabetes Control and Implications for Cardiovascular Disease
Quick Takes
- There has been a lack of improvement in control of multiple risk factors in persons with diabetes in the last decade, perhaps attributable to "therapeutic inertia" despite newer effective drug agents.
- It is important to identify deficits in translating recommended treatment options and overcoming regional, socioeconomic, and financial barriers in persons with diabetes.
- Greater emphasis is needed on achieving guideline recommended targets to improve the standard level of care among younger persons with diabetes focusing on prevention of future microvascular and macrovascular complications.
Diabetes is an ongoing epidemic that has increased in prevalence in the United States (US) and globally. An estimated 47 million in adults in the US are living with diabetes which places them at a higher risk for cardiovascular (CV) complications including premature death.1 Various studies have shown that the complications of diabetes can be curbed specifically with improved targets for lipid, blood pressure (BP) and tighter diabetes control.2-4 Over the last two decades there has been significant advancements in the form of newer agents from different drug classes that have a specific role in improvement in risk factor management and diabetes control.5,6 There are clinical guidelines that highlight of treatment options and focus on combination therapies for improved outcomes tailored to individual patients with diabetes. It is essential to understand these trends in the use of various diabetes treatments to better contextualize our current status of risk factor control.7 Indeed, despite these significant achievements in treatment options for diabetes, recent analysis shows that the progress in control of outcomes may be stalled.5
The study by Fang et al. on trends in diabetes treatments and controls in US Adults, 1999 – 2018 published in New England Journal of Medicine included participants from the National Health and Nutritional Examination Survey (NHANES) which is a series of nationally representative, cross-sectional studies designed to monitor the health of the US population. They looked at 6,653 persons with diabetes, non-pregnant, and aged 20 years or greater from the period of 1999 to 2018.
The study considered various factors including glycated hemoglobin (<7.0%), hypertension <140/90 mm Hg, non–HDL-C <130 mg dl and LDL-C <100 mg /dl, medication use (single, multiple), socioeconomic background, and educational background apart from height, weight, body mass index (BMI), smoking status, and age at diagnosis of diabetes.
Participant's characteristics were evaluated over time along with estimated prevalence of risk factor control and medication use. Temporal trends were assessed with the use of two-piece linear spline models, time modeled at 4-year survey years into 4-year intervals. They assessed the number of glucose lowering, BP and lipid lowering agents used overall and across specific risk factor control.
Results
Trends for diabetes risk factors, including glycemic control, BP and lipid control were nonlinear and showed an infliction point around 2010. Overall, there was some improvement in all three categories, however when all years were modeled, the annual rate of change in diabetes control decreased for all outcomes from 1999 to 2018. Of note, the proportion controlled for all three risk factors (HbA1c, BP, and non-HDL-C) reached a peak of 24.9% in 2007-2010 but has stalled or even decreased since then (22.2% in 2015-2018).
Trends in Diabetes Treatment
Anti-glycemic therapies, specifically metformin, insulin, and newer agents such as sodium-glucose co-transporter 2 (SGLT2) inhibitors showed an increase from 1999 to 2018, while there were decreases in the use of sulfonylureas and thiazolidinediones. Among antihypertensive therapies, there was an increase in the use of beta blockers and angiotensin receptor converting enzyme inhibitors from 1999 to 2018, while there was no increase in the use of calcium channel blockers and diuretics. Therapy for dyslipidemia with statins showed a significant increase in use up to 2014 before levelling off. Combination therapies for diabetes and hypertension increased until 2010, specifically in those with poor glycemic control. Younger Mexican American adults with no insurance were less likely to receive guideline directed therapy and reach risk factor targets. Black persons compared to White persons were more likely to receive combination therapies for hypertension (HTN) over glycemic treatments.
Discussion
Overall, the study shows that treatment of diabetes, HTN and lipid control improved from 1999 to 2010 and declined thereafter along with stalling of treatment for lipid control in line with recent research.5 As the authors point out, major trials about more relaxed target cut offs in glycemic control and HTN and their relation to CV outcomes during 2008-2010 may have influenced the relaxation in the treatment strategies in the following years leading to a less intensive management course.8-10 On the other hand, the recent years have seen the emergence of more robust trials of SGLT2-inhibitors and GLP1-receptor agonists, icosapent ethyl, and PCSK9 inhibitors demonstrating improved CV outcomes; however, these improved and newer treatment options may not have translated into meaningful changes in practice due to their high costs and no generic alternatives.11 It is a known fact that uncontrolled risk factors of diabetes continue to confer significant risk of microvascular disease, CV outcomes, and even death among patients with type 2 diabetes.1 The poor control of composite risk factors (HbA1c, non-HDL-C, and BP) observed in this study can be compared with that reported by the Diabetes Collaborative Registry in nearly 75,000 US adults with diabetes, where it was noted 25% were at target for HbA1c, BP, and LDL-C, but lower at 15% if the more recent BP target of <130/80 mmHg is used.12 This lack of composite risk factor control is significant, given a large pooled cohort study showing that risks of CV outcomes are 60% lower if all three of these factors (vs. none) are at target.13
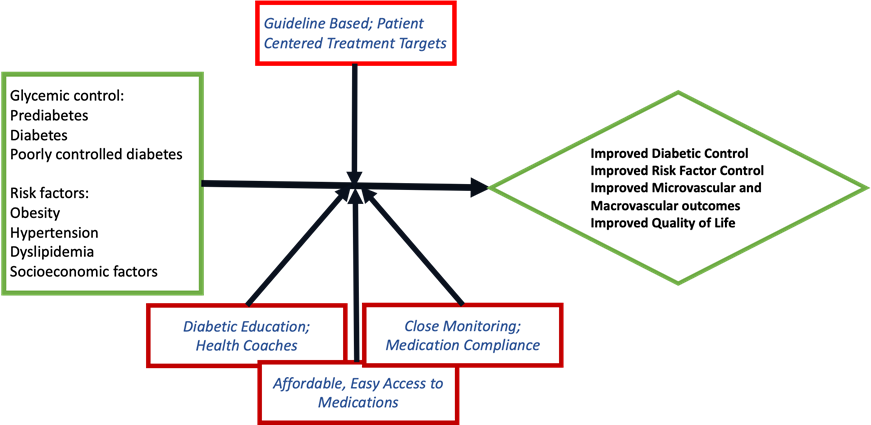
Clinical inertia needs to be improved to better address composite risk factor control if we are to make advances in further reducing CV disease complications in persons with diabetes. To improve progress in treatment and outcomes, we believe in a multi-strategy approach which can also curb the predicted increase in diabetes and outcomes. It should start with education of the population about diabetes and its CV risks in general and the importance of greater adherence to lifestyle management and medications. It should continue with reinforcing current treatment guidelines encouraging the general physicians to risk stratify their patients into pre-diabetic, diabetic, and high-risk diabetic groups. The focus should be on prevention (primary secondary and tertiary) with appropriate guideline recommended targets with special focus on high-risk patients with uncontrolled risk factors. This would mean early initiation of first line therapies which means accessible and affordable medicine targeting the vulnerable population groups like younger, socioeconomic, or ethnic uninsured minorities, as identified in the study. Finally, the importance of shared decision making cannot be overemphasized in helping patients understand their diagnosis and treatment expectations; furthermore, educating them about available medication therapies, medication compliance, and lifestyle changes helps in improved outcomes.
Figure 1
References
- National Diabetes Statistics Report 2020 (CDC website). 2020. Available at: https://www.cdc.gov/diabetes/pdfs/data/statistics/ national-diabetes-statistics-report.pdf. Accessed 11/30/2020.
- Cholesterol Treatment Trialists' (CTT) Collaborators. Efficacy of cholesterol lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet 2008;371:117-25.
- UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703–13.
- Gæde P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008;358:580-91.
- Kazemian P, Shebl FM, McCann N, Walensky RP, Wexler DJ. Evaluation of the cascade of diabetes care in the United States, 2005-2016. JAMA Intern Med 2019;179:1376-85.
- Kalyani RR. Glucose-lowering drugs to reduce cardiovascular risk in type 2 diabetes. N Engl J Med 2021;384:1248-60.
- American Diabetes Association. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes - 2021. Diabetes Care 2021;44:S111-S124.
- ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560-72.
- Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545-59.
- Duckworth W, Abraira C, Moritz T, et al. Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 2009;360:129-39.
- Taylor SI. The high cost of diabetes drugs: disparate impact on the most vulnerable patients. Diabetes Care 2020;43:2330-32.
- Fan W, Song Y, Inzucchi SE, et al. Composite cardiovascular risk factor target achievement and its predictors in US adults with diabetes: the Diabetes Collaborative Registry. Diabetes Obes Metab 2019;21:1121-27.
- Wong ND, Zhao Y, Patel R, et al. Cardiovascular risk factor targets and cardiovascular disease event risk in diabetes: a pooling project of the Atherosclerosis Risk in Communities Study, Multi-Ethnic Study of Atherosclerosis, and Jackson Heart Study. Diabetes Care 2016;39:668-76.
Clinical Topics: Cardiovascular Care Team, Diabetes and Cardiometabolic Disease, Dyslipidemia, Prevention, Lipid Metabolism, Nonstatins, Novel Agents, Statins, Hypertension
Keywords: Glycated Hemoglobin A, PCSK9 protein, human, Antihypertensive Agents, Body Mass Index, Calcium Channel Blockers, Cholesterol, LDL, Cross-Sectional Studies, Hydroxymethylglutaryl-CoA Reductase Inhibitors, Proprotein Convertase 9, Sodium-Glucose Transporter 2 Inhibitors, Diabetes Mellitus, Type 2, Cohort Studies, Blood Pressure, Decision Making, Shared, Glycemic Control, Medically Uninsured, Mortality, Premature, Nutrition Surveys, Prediabetic State, Vulnerable Populations, Risk Factors, Diabetes Complications, Dyslipidemias, Hypertension, Hypertension, Treatment Outcome, Diuretics, Medication Adherence, Receptors, Angiotensin, Thiazolidinediones, Life Style, Metformin, Metformin, Insulins, Registries, Glucose, Pharmaceutical Preparations
< Back to Listings