2022 ACC Expert Consensus Decision Pathway on COVID-19: Return-to-Play Take Home Points
Quick Takes
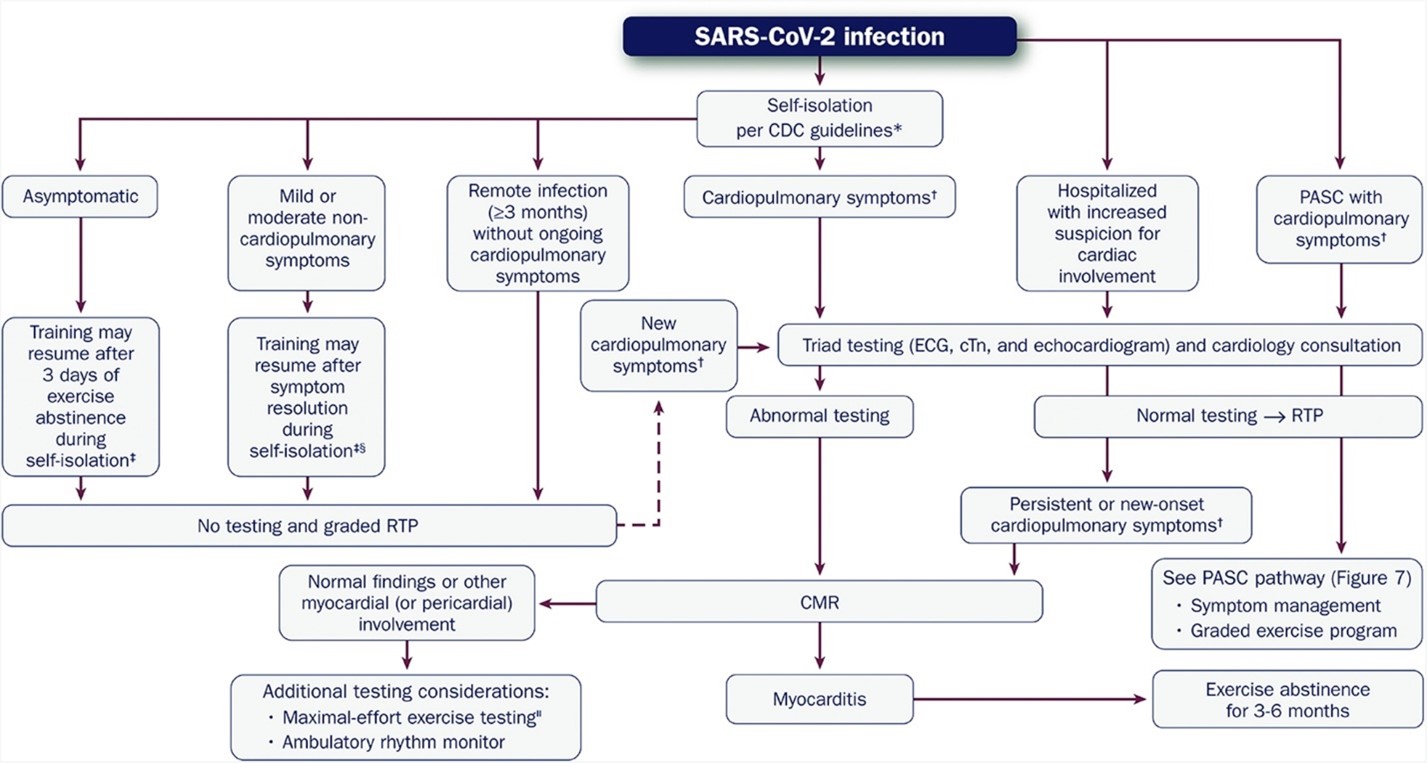
- The clinical evaluation of athletes infected with COVID-19 and prior to return-to-play should be dictated by the presence of cardiopulmonary symptoms and not 'screening'.
- Triad testing consists of a 12-lead electrocardiogram, cardiac troponin (preferably high sensitivity), and an echocardiogram.
- Regardless of symptomatology, all athletes with prior COVID-19 should implement a graded return-to-play regimen.
Over 2 years into the novel coronavirus disease 2019 (COVID-19) pandemic and after millions of individuals have been infected and affected, more evolving evidence and lingering questions have encouraged the need for guidance regarding the cardiovascular sequelae of the disease. An American College of Cardiology (ACC) expert panel convened to provide insight and an updated clinical resource for clinicians regarding the common questions surrounding myocarditis, post-acute sequelae of SARS-CoV-2 infection (PASC), and return-to-play (RTP). Here, we will summarize the top 10 take-home points from the RTP section of the 2022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults.1
- The prevalence of clinical myocarditis in athletes following SARS-CoV-2 infection is low.
Early reports from single-center, small-sized case series suggested a higher prevalence of myocarditis, which added to the initial apprehension regarding the safety of competitive athletes. With continued clinical vigilance and the development of much larger registries of competitive athletes recovered from COVID-19, current data suggests that the true prevalence of clinical myocarditis in this population is very low and closer to 0.5%-0.7%. - Cardiac testing is not required for every athlete.
Initial conservative recommendations had a much lower threshold for triad testing (electrocardiogram [ECG], cardiac troponin [cTn] [preferably high sensitivity], and echocardiogram) prior to RTP for competitive athletes. Cardiac triad testing is now only recommended in those with cardiopulmonary symptoms (e.g., chest tightness, worsening exertional shortness of breath, palpitations, lightheadedness/syncope). In addition, for those athletes with new cardiopulmonary symptoms after RTP and/or those requiring hospitalization for a suspected cardiac cause, cardiac testing should be performed. For athletes who are asymptomatic or have non-cardiopulmonary symptoms, no cardiac testing is recommended prior to RTP (Figure 1).
Figure 1Figure 1: Evaluation of the Athletic Patient Convalesced From COVID-19 and Guidance on RTP and/or Intense Training. Reprinted with permission from Gluckman TJ, Bhave NM, Allen LA, et al. 2022 ACC expert consensus decision pathway on cardiovascular sequelae of COVID-19 in adults: myocarditis and other myocardial involvement, post-acute sequelae of SARS-CoV-2 infection and return to play: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol 2022;Mar 14:[Epub ahead of print]. - Routine cardiovascular magnetic resonance imaging (CMR) screening in athletes after SARS-CoV-2 infection is not recommended.
There are a fair number of limitations to recognize when considering CMR as a screening tool for athletes with prior COVID-19. For these reasons, CMR is more efficacious as a diagnostic resource when suspicion of myocarditis or other myocardial or pericardial involvement is strongly suspected; namely if one or more of the cardiac triad tests are abnormal (when obtained if athletes have symptoms with high pre-test probability for myocarditis) or if cardiopulmonary symptoms persist or occur after a graded return-to-training. - RTP can occur sooner depending on symptoms.
The 10-day recommendation for exercise abstinence is no longer necessary. While still recognizing the Centers for Disease Control and Prevention (CDC) self-isolation guidelines (currently 5 days), asymptomatic athletes with COVID-19 may resume training after 3 days of exercise abstinence. For those with mild-moderate, non-cardiopulmonary symptoms, training can resume after symptom resolution (this excludes anosmia and ageusia which may have a prolonged course). - While current consensus recommendations state that athletes with myocarditis should avoid exercise training for 3-6 months, there is a call for more evidence in this arena.
Standard practice, based on the 2015 AHA/ACC Sports Eligibility Statement,2 is 3-6 months of complete abstinence from exercise for individuals with clinical myocarditis. New data from the Big 10 COVID-19 Registry3 suggest that it may be reasonable to reassess for resolution of myocardial inflammation in athletes with COVID-19 myocardial involvement earlier than 3 months, particularly if they had rapid resolution of symptoms and clinical sequalae (imaging findings, cardiac biomarkers) of cardiac involvement. The timing of earlier testing should be individualized, but no sooner than 1 month since diagnosis. - Regardless of symptomatology, all athletes with prior COVID-19 should implement a graded RTP regimen.
It is important for all athletes participating in organized competitive sports, with the support of their medical/training staff, to monitor closely for new or recurrent cardiopulmonary symptoms that would warrant cardiac testing after RTP. Most individuals participating in recreational athletics are not monitored nor have access to concierge medical professionals, so diligent surveillance for symptoms during graded RTP is vital. - Athletes with remote SARS-CoV-2 infection without ongoing cardiopulmonary symptoms may resume training without testing.
With over 78 million cases of SARS-CoV-2 infection in America, and a patient population that spans from youth sports (aged <18 years) to Masters (aged >35 years) athletes, today's clinicians are sure to see athletes who were previously infected and are ready to return to their sport. If an athlete had a remote infection (>3 months) and no longer has any cardiopulmonary symptoms, no further cardiac testing is required. - Athletes who receive a COVID-19 mRNA vaccine do not require routine screening for myocarditis prior to RTP.
Data currently shows that post-vaccination myocarditis following COVID-19 vaccination is rare. It is not recommended to screen for post-vaccination myocarditis in the absence of suggestive symptoms. - Cardiac testing beyond CMR (if necessary, based on the clinical evaluation) should be individualized.
As discussed, in athletes with cardiopulmonary symptoms after infection with SARS-CoV-2, or in those with new cardiopulmonary symptoms after RTP, cardiac triad testing should be performed. Abnormal findings or persistent symptoms should encourage additional evaluation with CMR. If warranted, only after ruling out acute myocarditis, maximal-effort exercise testing (stress echo if there is left ventricular systolic dysfunction) and ambulatory rhythm monitoring may be helpful in the clinical evaluation. - Repeat cardiac testing in athletes with recurrent SARS-CoV-2 infection should be limited to those who have cardiopulmonary symptoms.
Due to the high transmissibility of the SARS-CoV-2 virus and the advent of new variants, many athletes, regardless of vaccination status, will be infected more than once. For these athletes, repeat cardiac testing is not warranted in the absence of cardiopulmonary symptoms.
References
- Gluckman TJ, Bhave NM, Allen LA, et al. 2022 ACC expert consensus decision pathway on cardiovascular sequelae of COVID-19 in adults: myocarditis and other myocardial involvement, post-acute sequelae of SARS-CoV-2 infection and return to play: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol 2022;Mar 14:[Epub ahead of print].
- Maron BJ, Udelson JE, Bonow RO, et al. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: task force 3: hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, and myocarditis: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2015;66:2362-71.
- Daniels CJ, Rajpal S, Greenshields JT, et al. Prevalence of clinical and subclinical myocarditis in competitive athletes with recent SARS-CoV-2 infection: results from the Big Ten COVID-19 Cardiac Registry. JAMA Cardiol 2021;6:1078–87.
Clinical Topics: Cardiovascular Care Team, COVID-19 Hub, Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Noninvasive Imaging, Prevention, Sports and Exercise Cardiology, Heart Failure and Cardiac Biomarkers, Magnetic Resonance Imaging, Exercise, Sports and Exercise and ECG and Stress Testing, Sports and Exercise and Imaging
Keywords: COVID-19, COVID-19 Vaccines, SARS-CoV-2, Return to Sport, Exercise Test, Myocarditis, Ageusia, Anosmia, Dizziness, Pandemics, Youth Sports, Sports, Athletes, Electrocardiography, Biomarkers, Centers for Disease Control and Prevention, U.S., Magnetic Resonance Imaging, Dyspnea, Exercise, Hospitalization, Inflammation, Vaccination, Registries, Troponin, Syncope
< Back to Listings