The Influence of Diabetes on the Progression of Heart Failure: Minimizing the Risk
Quick Takes
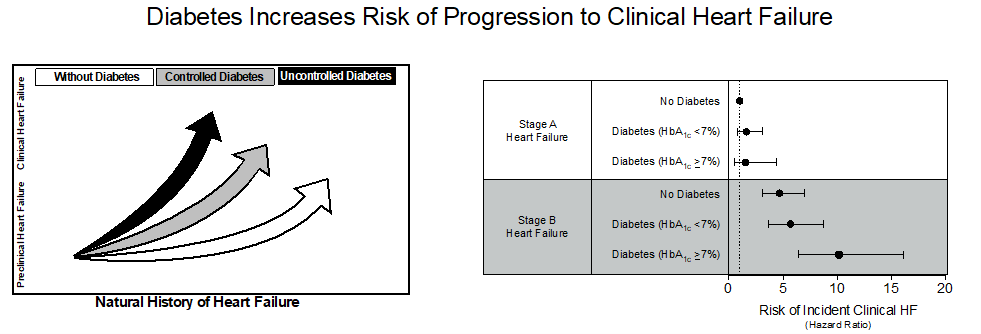
- Diabetes accelerates the progression from preclinical heart failure (Stages A and B, per universal definition) to clinical overt heart failure (Stages C and D).
- Better glycemic control (HbA1C <7%) limits the progression of preclinical to clinical heart failure in individuals with diabetes mellitus.
Commentary on Echouffo-Tcheugui JB, Ndumele CE, Zhang S, et al. Diabetes and progression of heart failure: the Atherosclerosis Risk In Communities (ARIC) Study. J Am Coll Cardiol 2022;79:2285-93.1
About one in three patients with heart failure (HF) have diabetes mellitus (DM).2 DM is a strong risk factor for the development of HF; however, the effect of DM on the early stages of the natural history of HF is not well characterized.3 Echouffo-Tcheugui et al. examined the progression of preclinical HF to clinically symptomatic HF in individuals with and without DM utilizing data from the Atherosclerosis Risk in Communities (ARIC) Study.
Summary
Among 4,774 individuals with preclinical HF (Stage A or B per universal definition), the progression to Stages C and D and associated characteristics was evaluated. Of the study participants (mean age 75.4 years, 58% Women, 20% Black), 30% had DM, about one-third had Stage A and two-thirds had Stage B. Over a median follow-up of 7.5 years, HF events were ascertained, and the absolute and relative risks HF in relation to DM were estimated.
The absolute risk of progression to HF was higher among those with DM across preclinical HF stages. In Stage A HF, individuals with DM had a HF incidence rate of 5.7 per 1,000-person years, versus 3.6 per 1,000-person years in those without DM. In Stage B HF, the incidence rate per 1,000-person years increased to 19.0 and 25.7, among those without and with DM, respectively. A similar pattern was observed with the HF relative risk, which was enhanced by DM across preclinical stage, but overall higher in Stage B versus Stage A, irrespective of DM status ̶ hazard ratios (HR) in Stage A: 1.0 (without DM), 1.60 (with DM); Stage B: 4.7 (without DM), 6.87 (with DM).
Further exploration of the effects of uncontrolled DM (HbA1C ≥7%) demonstrated that uncontrolled DM significantly increased the relative risk of developing clinical HF compared to controlled DM (HbA1C <7%) more so in Stage B than Stage A. Using Stage A individuals without DM as reference, the HRs for incident clinical HF in Stage B was 10.2 in individuals with uncontrolled DM and 5.7 in individuals with controlled DM, respectively.
This report demonstrates a gradient of risk of progression to clinical HF across stages of preclinical HF stages, as well as highlights the deleterious effect of DM and poor glycemic control, in accelerating the progression of preclinical HF to overt HF, especially in Stage B HF.
Perspective
With this community-based study, we gain further insight into the accelerating effect of DM on the progression of preclinical HF to clinical HF. This study highlights that 1) patients with DM have an accelerated progression towards HF, and 2) better glycemic control is important in patients with DM to prevent progression of HF.
The importance of preventing the progression of HF in patients with DM lies within targeting the populations most at risk. Individuals with structural disease or elevated biomarkers (Stage B HF) have a higher risk of developing HF than those individuals at risk (Stage A), and thus may be more vulnerable to the effect of DM.
Previous observational studies have aided in the identification of phenotypes (structural/functional ventricular dysfunction, and/or elevated cardiac biomarkers) that predict cardiovascular risk; this underlines the need to recognize these subtle asymptomatic states.4 Thus, differentiating those in Stage A HF from those in Stage B HF is important to our understanding the extent of the risk of developing clinical HF among individuals with DM.
Previous work showed that the duration of DM increases the incident risk of HF; there was an approximate 17% relative risk increase in HF risk with each 5-year increase in DM duration.5 Although individuals in this study had a variable duration of DM depending on the preclinical HF stage (9.4 ± 7.8 years in Stage A and 11.5 ± 8.6 years in Stage B), individuals with preclinical HF stages and longer duration of DM (>10 years) had a higher risk of incident clinical HF. This signals that continued emphasis on DM prevention and management with the relevant therapies will likely help delay the onset of clinical HF.
Among high-risk individuals with DM and Stage B HF, lower HF risk was observed among individuals maintaining a HbA1C <7%. This provides further insight into the role of DM and reinforces the notion that better glycemic control is likely particularly important for preventing HF. It is only logical to infer that, in addition to glycemic, the control of other modifiable risk factors including blood pressure and body mass index known to be associated with an increased HF risk6 will further enhance HF prevention.
Novel pharmacotherapies for DM, including the sodium-glucose cotransport-2 (SGLT2) inhibitors, have emerged as a primary pillar of guideline-directed medical therapy (GDMT) for HF, as these reduce the risk of HF-related hospitalizations. The benefits of SGLT2 inhibitors in preclinical HF are also emerging. The EMPA-HEART CardioLink-6 trial showed benefits of SGLT2 inhibitors in cardiac remodeling in patients with concomitant preclinical HF and DM.7 Further understanding the effect of SGLT2 inhibitors and other DM therapies (e.g., glucagon-like peptide [GLP-1] agonists) on cardiac remodeling will shed light into the best approaches to improve HF outcomes, especially among individuals with dysglycemia.
Final Thoughts
This study reinforces the importance of understanding DM in the context of HF. DM significantly increases the risk of progression from the preclinical HF stages to clinically overt HF. Identification of individuals with DM and preclinical HF (emphasizing Stage B) will be critical, with the implementation of targeted therapies including lifestyle interventions and antihyperglycemics.
Figure 1
References
- Echouffo-Tcheugui JB, Ndumele CE, Zhang S, et al. Diabetes and progression of heart failure: the Atherosclerosis Risk In Communities (ARIC) study. J Am Coll Cardiol 2022;79:2285-93.
- Echouffo-Tcheugui JB, Xu H, DeVore AD, et al. Temporal trends and factors associated with diabetes mellitus among patients hospitalized with heart failure: findings from Get With The Guidelines-Heart Failure registry. Am Heart J 2016;182:9-20.
- Echouffo-Tcheugui JB, Ogunmoroti O, Golden SH, et al. Glycemic markers and heart failure subtypes: the Multi-Ethnic Study of Atherosclerosis (MESA). J Card Fail 2022;Jan 31:[Epub ahead of print].
- Echouffo-Tcheugui JB, Musani SK, Bertoni AG, Correa A, Fox ER, Mentz RJ. Patients phenotypes and cardiovascular risk in type 2 diabetes: the Jackson Heart Study. Cardiovasc Diabetol 2022;21:89.
- Echouffo-Tcheugui JB, Zhang S, Florido R, et al. Duration of diabetes and incident heart failure: the ARIC (Atherosclerosis Risk In Communities) Study. JACC Heart Fail 2021;9:594-603.
- Hamo CE, Kwak L, Wang D, et al. Heart failure risk associated with severity of modifiable heart failure risk factors: the ARIC Study. J Am Heart Assoc 2022;11:e021583.
- Verma S, Mazer CD, Yan AT, et al. Effect of empagliflozin on left ventricular mass in patients with type 2 diabetes mellitus and coronary artery disease: the EMPA-HEART CardioLink-6 randomized clinical trial. Circulation 2019;140:1693-1702.
Clinical Topics: Heart Failure and Cardiomyopathies, Acute Heart Failure, Heart Failure and Cardiac Biomarkers, Dyslipidemia
Keywords: Sodium-Glucose Transporter 2 Inhibitors, Glycated Hemoglobin A, Ventricular Remodeling, Cardiovascular Diseases, Follow-Up Studies, Blood Pressure, Body Mass Index, Glycemic Control, Risk Factors, Heart Disease Risk Factors, Cardiometabolic Risk Factors, Heart Failure, Diabetes Mellitus, Hospitalization, Biomarkers, Ventricular Dysfunction, Asymptomatic Diseases, Atherosclerosis, Phenotype, Glucose, Sodium, Glucagon-Like Peptide 1
< Back to Listings