Key Takeaways From the 2021 Coronary Revascularization Guidelines
Quick Takes
- Learn the important updates to the management of stable ischemic heart disease from the 2021 revascularization guidelines.
- Understand circumstances where revascularization is indicated for coronary artery disease.
- Share updates on best practices for percutaneous and surgical revascularization.
The 2021 ACC/AHA/SCAI guideline for coronary artery revascularization take on a monumental task of synthesizing data over the last 10 years to consolidate prior coronary artery bypass graft (CABG), stable ischemic heart disease (SIHD), percutaneous coronary intervention (PCI), ST elevation myocardial infarction (STEMI), and non-ST-elevation myocardial infarction (NSTEMI) guidelines to create a simplified patient-centered revascularization approach.1 This article will highlight key takeaways and areas of dispute.
Disparities and Shared Decision-Making
New and unique to the 2021 revascularization guidelines is the emphasis on equity of care and the importance of shared decision making. Irrespective of risk factors or disease burden, women and racial or ethnic minorities are less likely to be offered medical therapy or revascularization, and often have worse outcomes.2,3 The writing committee made a conscious effort to stress that all revascularization decisions should be made without considering sex, race, or ethnicity. The 2021 guidelines also recognize that revascularization decisions are often nuanced and strongly recommend using a shared decision-making approach and Heart Team involvement in difficult clinical decisions.
Revascularization in SIHD to Improve Survival
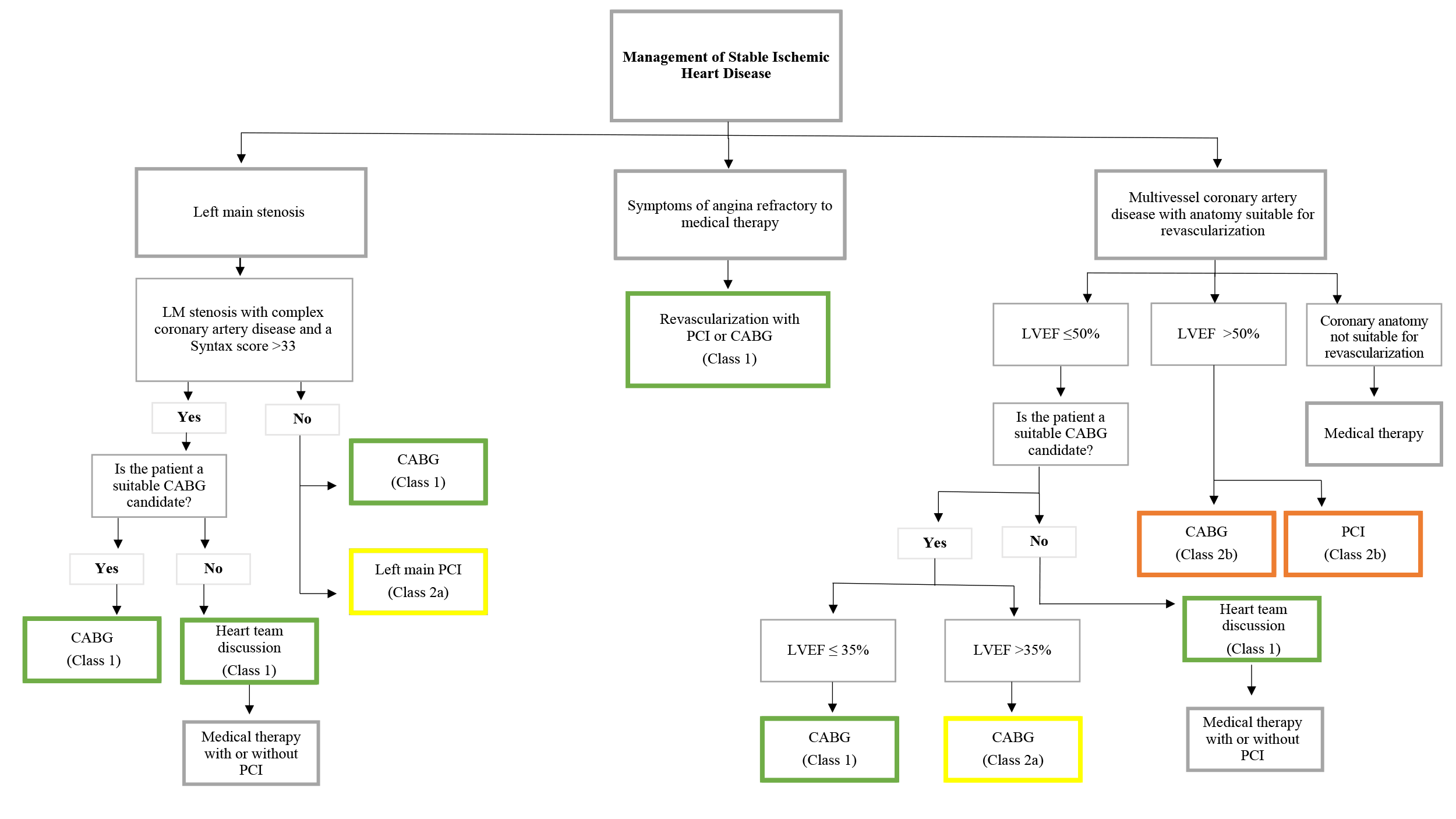
Arguably the most significant changes to the 2021 guidelines are updates on the management of SIHD with a clear deemphasis on the role for revascularization outside of the following groups: left ventricular ejection fraction (LVEF) ≤35%, left main (LM) disease, diabetes mellitus (DM), or refractory angina despite optimal medical therapy (OMT) (Figure 1).
Figure 1
Revascularization for a survival benefit in patients with multivessel coronary artery disease (CAD) and a normal LVEF was downgraded from class 1 to 2B. This was largely driven by the 2020 ISCHEMIA trial data. ISCHEMIA randomized approximately 5,000 patients with moderate/severe ischemia on stress testing to a routine invasive strategy (PCI or CABG) versus OMT alone and found no significant difference in major adverse cardiovascular events (MACE).4 Revascularization for isolated proximal left anterior descending artery (LAD) disease was also downgraded to a 2B recommendation. PCI in 1-2 vessel CAD not involving the LAD, in the setting of a normal LVEF, received a class 3 recommendation.
CABG retains a class 1 recommendation in patients with LVEF ≤35% primarily based on the 2016 STITCH Extension study showing a long-term mortality benefit for CABG versus OMT.5 CABG also remains a class 1 recommendation in LM disease.6,7 LM PCI is a reasonable alternative to CABG and remains a 2A recommendation in select patients.6,8
PCI versus CABG in Complex CAD, DM, and LM Disease
Numerous randomized controlled trials, including FREEDOM, NOBLE, and EXCEL, studied PCI versus CABG in cases of LM disease, DM, and complex CAD.7,9,10 The updated guidelines give a class 1 recommendation for a survival benefit with CABG for patients with DM with multivessel (MV) CAD, and LM disease with complex CAD.7,9,11 In patients with complex multivessel CAD (SYNTAX score >33), CABG has a 2A recommendation for a survival benefit over PCI, although a Heart Team approach is recommended given multiple studies showing patients with less complex disease (SYNTAX score <33) likely do equally well with CABG or PCI.6,10,12 There is a new 2A recommendation for PCI in patients with DM with MV CAD who are poor surgical candidates.13
Revascularization in SIHD to Reduce CV Events
A section on revascularization to reduce cardiovascular events is new as previous guidelines focused only on survival or symptoms. There is a 2A recommendation for revascularization in SIHD with multivessel CAD (not including LM) and normal LVEF to reduce the risk of cardiac death, spontaneous myocardial infarction, and unplanned urgent revascularization. This is supported by ISCHEMIA, FAME 2, and 10-year updates from the MASS II trial showing a reduction in CV mortality with revascularization versus OMT alone.4,14,15 Revascularization either by CABG or PCI remains a class 1 recommendation for uncontrolled angina despite OMT.16
Complete Revascularization in ACS
The STEMI/NSTEMI guidelines remain largely unchanged. A notable exception is the upgraded and more nuanced recommendation on the management of non-infarct arteries in acute coronary syndrome (ACS). Staged PCI of the non-infarct artery in hemodynamically stable patients has a class 1 recommendation based on data showing a reduction in MACE.17 STEMI cases complicated by cardiogenic shock however are assigned a class 3 (harm) recommendation for routine PCI of non-culprit arteries based on evidence from the CULPRIT-SHOCK trial.18
PCI Focused Updates: Radial Access, Drug Eluting Stents, and DAPT
The guidelines make note of several best practices for operators and generally mirror current practice trends although with some significant differences compared to the 2011 guidelines. Radial artery access is the preferred method for coronary angiography and PCI based on reduced death, bleeding, and vascular complications.19 Currently available drug eluting stents (DES) have a class 1 recommendation over bare‐metal stents (BMS) for all patients. Dual anti-platelet therapy (DAPT) recommendations reflect current practice patterns, and short durations (1-3 months) of DAPT following PCI in SIHD for select patients is supported with a class 2 recommendation. Other notable changes include downgrading embolic protection devices in saphenous vein graft (SVG) interventions from class 1 to 2A and highlighting unfractionated heparin as the only class 1 anticoagulant for PCI unless contraindicated.
CABG Focused Updates
An internal mammary artery (IMA) graft remains the preferred choice for the LAD; however, there is a new class 1 recommendation for using a radial artery bypass graft over a SVG for the next most important (non-LAD) vessel. Previous guidelines gave radial artery use a 2B recommendation. The 2A recommendation for bilateral IMA grafting is unchanged.
Noteworthy Controversy
These guidelines have not been endorsed by the surgical societies Society of Thoracic Surgeons (STS) and American Association for Thoracic Surgery (AATS) despite representatives from both being on the guideline committee. The STS/AATS explained their reasoning in a joint 2022 editorial.20 Dissent was focused on three areas: (1) overemphasis of the ISCHEMIA trial leading to the downgrade of CABG to 2B in SIHD, (2) grouping together of PCI and CABG for the reduction of ischemic events without acknowledging differences in repeat reintervention and postprocedural MI, and (3) the class 1 recommendation for radial artery bypass graft above bilateral IMA grafts without including patient selection qualifiers.
Conclusion
The 2021 revascularization guidelines provide a concise and comprehensive review of best practices for the management of patients with CAD. Several important takeaways are highlighted in this article, and it should be noted that even with ongoing debate there is still much more consensus than disagreement.
References
- Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol 2022;79:e21–e129.
- Ya'qoub L, Lemor A, Dabbagh M, et al. Racial, ethnic, and sex disparities in patients with STEMI and cardiogenic shock. JACC Cardiovasc Interv 2021;6:653–60.
- Havrenak EP, Mujahid SM, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease. Circulation 2015;132:873-898.
- Maron DJ, Hochman JS, Reynold HR, et al. Initial invasive or conservative strategy for stable coronary disease. N Engl J Med 2020;382:1395-1407.
- Velazquez E, Lee KL, Jones RH, et al. Coronary artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med 2016;374:1511-20.
- Thuijs DJFM, Kappetein AP, Serruys PW, et al. Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicenter randomized controlled SYNTAX trial. Lancet 2019;394:1325-34.
- Holm NR, Mäkikallio T, Lindsay MM, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in the treatment of unprotected left main stenosis: updated 5-year outcomes from the randomized, non-inferiority NOBLE trial. Lancet 2020;395:191-99.
- Bittl JA, He Y, Jacobs AK, Yancy CW, Normand SL. Bayesian methods affirm the use of percutaneous coronary intervention to improve survival in patients with unprotected left main coronary artery disease. Circulation 2013;127:2177-85.
- Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012;367:2375-84.
- Stone GW, Kappetein AP, Sabik JF, et al. Five-year outcomes after PCI or CABG for left main coronary disease. N Engl J Med 2019;381:1820-30.
- Park SJ, Ahn JM, Kim YH, et al. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med 2015;372:1204-12.
- Buszman PE, Buszman PP, Banasiewicz-Szkrobka I, et al. Left main stenting in comparison with surgical revascularization: 10-year outcomes of the (Left Main Coronary Artery Stenting) LE MANS Trial. JACC Cardiovasc Interv 2016;9:318-27.
- Pandey A, McGuire DK, de Lemos JA, et al. Revascularization trends in patients with diabetes mellitus and multivessel coronary artery disease presenting with non-ST elevation myocardial infarction: insights from the National Cardiovascular Data Registry Acute Coronary Treatment and Intervention Outcomes Network Registry-get with the guidelines (NCDR ACTION Registry-GWTG). Circ Cardiovasc Qual Outcomes 2016;9:197-205.
- Hueb W, Lopes NH, Gersh BJ, et al. Ten-year follow-up of the Medicine, Angioplasty, or Surgery Study (MASS II): a randomized controlled clinical trial of 3 therapeutic strategies for multivessel coronary artery disease. Circulation 2010;122:949–57.
- De Bruyne B, Fearon WF, Pijls NHJ, et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med 2014;371:1208-17.
- Fearon WF, Nishi T, De Bruyne B, et al. Clinical outcomes and cost-effectiveness of fractional flow reserve-guided percutaneous coronary intervention in patients with stable coronary artery disease: three-year follow-up of the FAME 2 Trial (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation). Circulation 2018;137:480-87.
- Mehta SR, Wood DA, Storey RF, et al. Complete revascularization with multivessel PCI for myocardial infarction. N Engl J Med 2019;381:1411-21.
- Thiele H, Akin I, Sandri M, et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med 2017;377:2419-32.
- Feldman DN, Swaminathan RV, Kaltenbach LA, et al. Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention: an updated report from the national cardiovascular data registry (2007-2012). Circulation 2013;127:2295-2306.
- Sabik JF, Bakaeen FG, Ruel M, et al. The American Association for Thoracic Surgery and The Society of Thoracic Surgeons reasoning for not endorsing the 2021 ACC/AHA/SCAI coronary revascularization guidelines. Ann Thorac Surg 2022;113:1065-68.
Clinical Topics: Acute Coronary Syndromes, Anticoagulation Management, Arrhythmias and Clinical EP, Cardiac Surgery, Cardiovascular Care Team, Heart Failure and Cardiomyopathies, Invasive Cardiovascular Angiography and Intervention, Noninvasive Imaging, Stable Ischemic Heart Disease, Vascular Medicine, Atherosclerotic Disease (CAD/PAD), Anticoagulation Management and ACS, Aortic Surgery, Cardiac Surgery and Arrhythmias, Cardiac Surgery and Heart Failure, Cardiac Surgery and SIHD, Acute Heart Failure, Interventions and ACS, Interventions and Coronary Artery Disease, Interventions and Imaging, Interventions and Vascular Medicine, Angiography, Nuclear Imaging, Chronic Angina
Keywords: Coronary Artery Disease, Drug-Eluting Stents, Percutaneous Coronary Intervention, Coronary Angiography, Stroke Volume, Heparin, Non-ST Elevated Myocardial Infarction, Platelet Aggregation Inhibitors, ST Elevation Myocardial Infarction, Patient Selection, Acute Coronary Syndrome, Decision Making, Shared, Dual Anti-Platelet Therapy, Ethnic Groups, Mammary Arteries, Radial Artery, Saphenous Vein, Shock, Cardiogenic, Thoracic Surgery, Ventricular Function, Left, Coronary Artery Bypass, Risk Factors, Embolic Protection Devices, Patient-Centered Care, Cost of Illness, Anticoagulants, Diabetes Mellitus, Surgeons
< Back to Listings