Cardiovascular and Cerebrovascular Disease Mortality in Asian American Subgroups
Quick Takes
- Age-standardized mortality rates (ASMR) for ischemic heart disease (IHD), heart failure (HF), and cerebrovascular accident (CVA) were calculated for Asian American subgroups. There was heterogeneity in cardiovascular and cerebrovascular mortality among Asian Americans, with increasing or stagnant mortality trends seen in several subgroups.
- Differences in risk may be drawn back to variability in access to care, cultural and behavioral practices, acculturation, and length of residence in the United States, as well as difference in risk factor burden within each subgroup.
Editor's note: Commentary based on Shah NS, Xi K, Kapphahn KI, et al. Cardiovascular and cerebrovascular disease mortality in Asian American subgroups. Circ Cardiovasc Qual Outcomes 2022;May 10:[ePub ahead of print].1
Asian Americans are a diverse group of population comprising of Chinese, Asian Indian, Filipino, Japanese, Korean, or Vietnamese American. Hence, aggregate reports of cardiovascular risk factors and mortality statistics may mask differences in health status and outcomes among various subgroups within the Asian American population. Additionally, cardiovascular disease (CVD) risk factors are not distributed uniformly across all Asian American groups. Asian Indian adults have a high prevalence of diabetes whereas Filipino adults have a high prevalence of hypertension.2,3
Shah et al. sought to estimate mortality patterns from ischemic heart disease (IHD), heart failure (HF), and cerebrovascular accident (CVA) in disaggregated Asian American subgroups to inform CVD prevention and management for the heterogenous Asian American population.1
Methods: Death certificate data were obtained from the National Center for Health Statistics for the six subgroups of Asian Americans (Chinese, Asian Indian, Filipino, Japanese, Korean, and Vietnamese American). The International Classification of Diseases, Tenth Revisions (ICD-10) were used to identify who had IHD, HF, or CVA listed as cause of death on the death certificate. Regression models were used to estimate trends in terms of average annual percent change (AAPC) of age-standardized mortality rates (ASMR) over the entire study period (2003-2017).
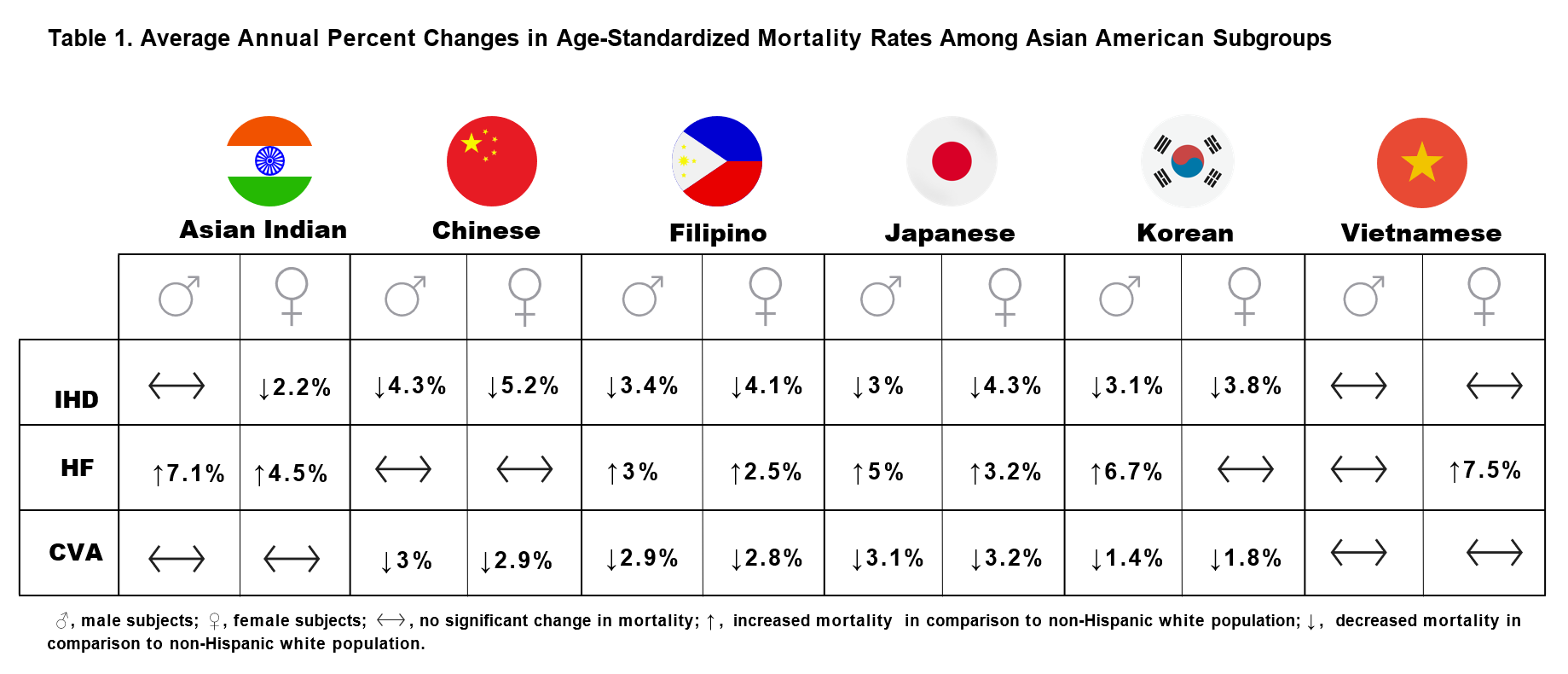
Main Findings: AAPC of ASMR from IHD/HF increased in Asian Americans on aggregate. ASMR by key outcomes by Asian subgroup and sex are shown in Table 1.
Indian American and Vietnamese American men did not have significant change in mortality from IHD. In women from 2003 to 2017, ASMR from HF significantly increased in Filipina women (2.5% per year [1.0 to 4.0]), Asian Indian American women (4.5% per year [2.3 to 6.7]), Japanese American women (3.2% per year [1.4 to 5.0]), and Vietnamese American women (7.5% per year [4.7 to 10.4]). AAPC of ASMR from CVA decreased in Chinese American women (-3% per year [-4.0 to -1.8]), Japanese American women (-3.1% per year [-4.2 to -2.0]), and Filipina American women (-2.8% per year [-3.8 to -1.7]), and Korean American women (-1.8% per year [-1.8 to 0.2]) in comparison to the reduction noted in non-Hispanic White (NHW) American women (-2.1% per year [-2.8 to -1.4]). AAPC of ASMR from CVA increased in Asian Indian American women (1.4% per year [-0.1 to 3.0]), as well as Asian Indian American men (1.6% per year [-0.3 to 3.5]) and Vietnamese American men (0.5% per year [-0.9 to 2.0]). AAPC of ASMR from IHD and CVA decreased in Korean men (-3.1% per year [-3.9 to -2.3] and -1.4% per year [-3.3 to 0.5]) and women (-3.8% per year [-4.7 to -3.0] and -1.8% per year [-3.5 to 0.0]), while mortality from HF did not change.
Discussion
The study by Shah et al. builds on the findings of previous studies describing diverse mortality patterns among Asian American subgroups.4-6 For example, heart and stroke mortality data for Asian American subgroups between 2003 and 2010 revealed that Asian Indian American and Filipino men had the greatest proportional mortality burden from IHD compared to NHW adults.4 National Centers for Disease Control and Prevention's Wide-ranging Online Data for Epidemiologic Research (CDC-WONDER) data (2018-2020) showed that Asian Indian American and Chinese American women had the greatest proportional mortality burden from IHD; Asian Indian American and Filipino men experienced significantly higher proportional mortality from IHD.5 Notably, the highest proportional mortality from IHD was observed in Asian Indian American men aged 45 to 64 years and Asian Indian American women aged >65 years.6
Among South Asian (SA) subgroups, Asian Indians typically have lower rates of coronary heart disease (CHD) compared to Pakistani and Bangladeshi adults, the difference likely driven by lower prevalence of traditional risk factors (hypertension, diabetes, obesity), and improved access to preventive care and pharmacotherapy (statins, for example).3 Notably, while there was an overall downward trend for IHD for all Asian Americans, an upward trend was noted around 2011 for Asian Indian men and women.1 Several factors could contribute to this disparity, including cultural and behavioral practices related to dietary habits and views on health and exercise, unrecognized or undermanaged traditional risk factors, social networks and neighborhood characteristics, length of residence in the United States (US) and acculturation strategy, generational differences (i.e., first vs. second generation immigrant), health seeking behavior, and language barriers.7-9 Between 2010 and 2018, The Affordable Care Act eliminated insurance coverage gaps between Asian Americans and NHW, suggesting that health care costs may not have been a barrier to medical access, particularly for Asian Indians who were least likely to be uninsured compared to other Asians ethnicities.10 Other South Asian subgroups (individuals who trace their ancestry from Bangladesh, Bhutan, India [included in the current study] the Maldives, Nepal, Pakistan, and Sri Lanka) were not included in this study due to limitations of data collection in the National Vital Statistics System; the US Census Bureau currently captures 'Asian Indian' and allows a write-in selection of "Other Asian" for remaining minority Asian subgroups. The inclusion of these subgroups would improve our understanding of mortality patterns among SA to help tailor CVD prevention and management in this higher risk group.
Mortality trends in this paper show an unsurprisingly close relationship between IHD and HF.11 Although the American Heart Association stages of HF were not defined due to limitations inherent to data capturing in this study, ASMR from HF significantly increased in Filipina and Asian Indian American women. While IHD mortality rates might have improved, the complication of HF from underlying CHD is well-observed in the Asian subpopulation.12,13 Given these findings, efforts should be directed towards determining ethnic specific screening guidelines and targeted prevention efforts. It may be of equal importance to investigate the cultural and behavioral habits of the Asian American sub-groups considering no change or reduction in cardiovascular risk burden in Chinese men and women, for example.1 The use of culturally specific data for Chinese American dietary habits, exercise routines and weight management resources, and smoking habits (including cessation interventions) could serve as a guide for other Asian American subgroups to mitigate cardiovascular risk burden.14-18
This timely report by Shah et al. highlights the importance of racial disaggregation to refine our understanding of health care disparities, as several groups experienced either increase, decrease, or stagnant trends in ASMR related to IHD, HF, and CVA. Specifically, this important body of work draws attention to multilevel social determinants of health and should influence clinical and population research in the area and emphasize the importance of implementing culturally appropriate CVD risk factor screening and preventive management strategies.
References
- Shah NS, Xi K, Kapphahn KI, et al. Cardiovascular and cerebrovascular disease mortality in Asian American subgroups. Circ Cardiovasc Qual Outcomes 2022;May 10:[ePub ahead of print].
- Ye J, Rust G, Baltrus, P, Daniels E. Cardiovascular risk factors among Asian Americans: results from a National Health Survey. Ann Epidemiol 2009;19:718-23.
- Banerjee AT, Shah B. One size does not fit all: diabetes prevalence among immigrants of the South Asian diaspora. J Immigr Minor Health 2021;23:653-58.
- Jose PO, Frank ATH, Kapphahn KI, et al. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol 2014;64:2486-94.
- Shah NS, Palaniappan LP, Khan SS. Proportional mortality from ischemic heart disease among Asian American subgroups, from 2018 to 2020. JAMA Intern Med 2022;182:1101-03.
- Kanaya AM, Kandula N, Herrington D, et al. Mediators of atherosclerosis in South Asians living in America (MASALA) study: objectives, methods, and cohort description. Clin Cardiol 2013;36:713-20.
- Enas EA, Garg A, Davidson MA, Nair VM, Huet BA, Yusuf S. Coronary heart disease and its risk factors in first-generation immigrant Asian Indians to the United States of America. Indian Heart J 1996;48:343-53.
- Ahmed F, Abel GA, Lloyd CE, Burt J, Roland M. Does the availability of a South Asian language in practices improve reports of doctor-patient communication from South Asian patients? Cross sectional analysis of a national patient survey in English general practices. BMC Fam Pract 2015;16:55.
- Lee S, Martinez G, Ma GX, et al. Barriers to health care access in 13 Asian American communities. Am J Health Behav 2010;34:21-30.
- Gap Closed: The Affordable Care Act's Impact on Asian Americans' Health Coverage (www.commonwealthfund.org). 2020. Available at: https://www.commonwealthfund.org/publications/issue-briefs/2020/jul/gap-closed-aca-impact-asian-american-coverage. Accessed 10/15/2022.
- Roth GA, Mensah GA, Johnson CO, et al.; GBD-NHLBI-JACC Global Burden of Cardiovascular Diseases Writing Group. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the GBD 2019 study. J Am Coll Cardiol 2020;76:2982-3021.
- Martinez-Amezcua P, Haque W, Khera R, et al. The upcoming epidemic of heart failure in South Asia. Circ Heart Fail 2020;Sep 23:[ePub ahead of print].
- Lam CSP, Teng TWK, Tay WT, et al. Regional and ethnic differences among patients with heart failure in Asia: the Asian sudden cardiac death in heart failure registry. Eur Heart J 2016;37:3141-53.
- Quit Smoking (www.lung.org) 2022. Available at: https://www.lung.org/quit-smoking. Accessed 10/15/2022.
- Chinese Diabetes Prevention Program (Chinese DPP) (https://clinicaltrials.gov). 2019. Avaliable at: https://clinicaltrials.gov/ct2/show/NCT02277509. Accessed 10/15/2022.
- Yeh MC, Lau W, Chen S, et al. Adaptation of diabetes prevention program for Chinese Americans – a qualitative study. BMC Public Health 2022;22:1325.
- Hou L, Chen B, Ji Y, Wang B, Wu J. China CDC in action — hypertension prevention and control. China CDC Weekly 2020;2:783-86.
- Chinese Society of Cardiology of Chinese Medical Association, Cardiovascular Disease Prevention and Rehabilitation Committee of Chinese Association of Rehabilitation Medicine, Cardiovascular Disease Committee of Chinese Association of Gerontology and Geriatrics, et al. Chinese guideline on the primary prevention of cardiovascular diseases. Cardiol Discov 2021;1:70–104.
Clinical Topics: Vascular Medicine, Prevention
Keywords: Asian Americans, Cardiovascular Diseases, International Classification of Diseases, Prevalence, Risk Factors, Diabetes Mellitus, Myocardial Ischemia, Stroke, Cerebrovascular Disorders
< Back to Listings