Antithrombotic Therapy in Athletes: A Balancing Act
Quick Takes
- Venous thromboembolism, atrial fibrillation, and coronary artery disease are the three main conditions for which antithrombotic therapy is indicated.
- Managing antithrombotic agents in athletes necessitates a personalized approach that balances the risks and benefits of therapy with considerations of both the underlying disease and the specific sport.
- In select patients, exploring opportunities for intermittent anticoagulation may be reasonable.
- Ultimately, the acceptable level of risk is a personal decision for the athlete, made in collaboration with health care professionals and using consensus recommendations and guidelines as a framework to develop individualized care plans through shared decision making.
Introduction
Antithrombotic agents provide critical protective benefits to individuals with cardiovascular (CV) disease, but the associated bleeding risk is particularity concerning for athletes and highly active individuals. Venous thromboembolism (VTE), atrial fibrillation (AF), and coronary artery disease (CAD) are the three main conditions requiring antithrombotic therapies, which include both anticoagulant and antiplatelet agents. In this piece, common indications for antithrombotic therapy and considerations that inform a comprehensive management approach in athletes are highlighted.
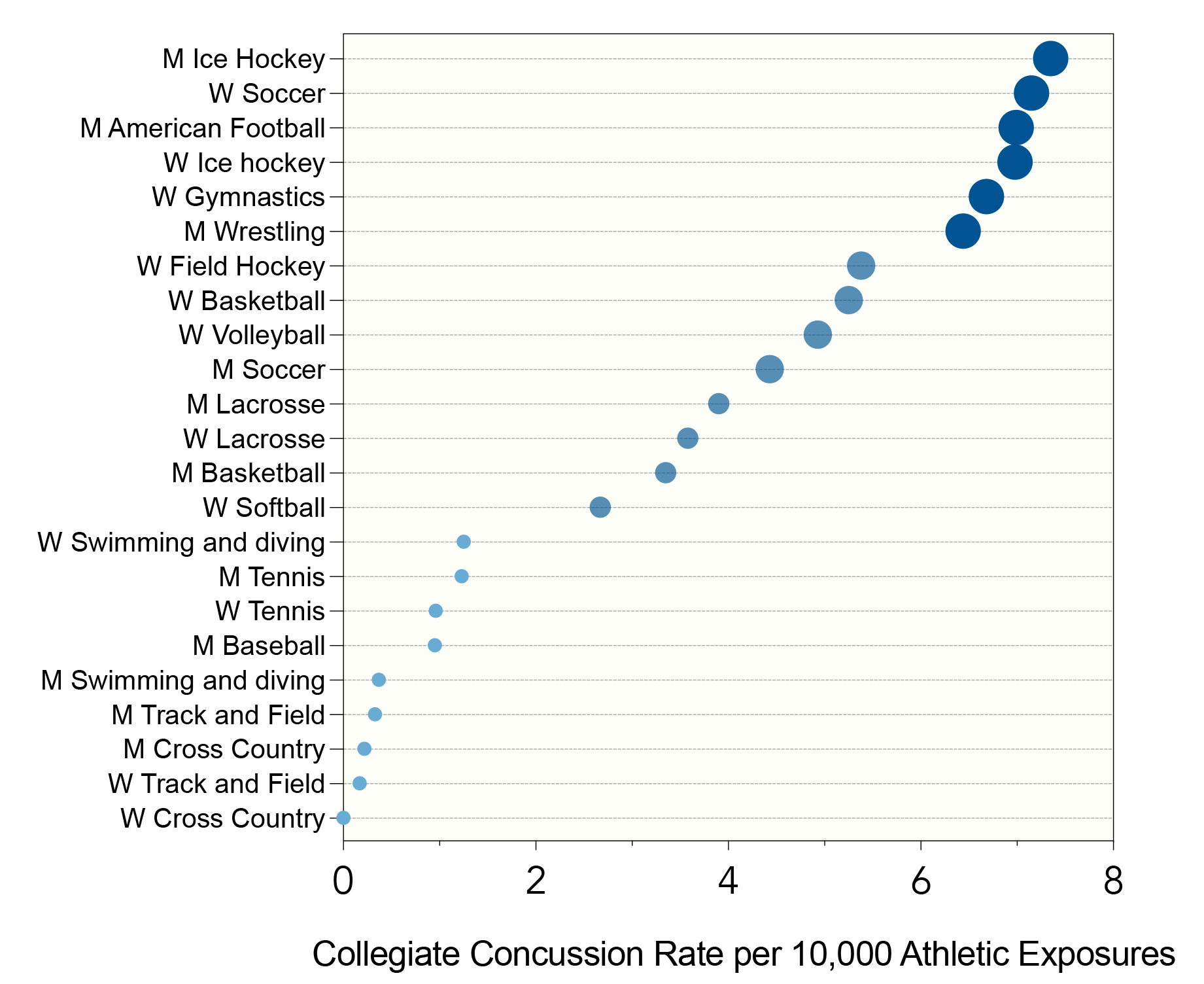
Athletes requiring antithrombotics have historically been temporarily or permanently disqualified from participating in contact sports. The dominant concern was of catastrophic intracranial hemorrhage thought to correlate with risk of concussion (Figure 1).1 Current guidelines suggest that athletes should be restricted from participation in high-impact competitive sports when anticoagulated.2 Commonly encountered high-impact sports include American-style football, ice hockey, soccer, basketball, and lacrosse. These contact sports are the most likely to increase bleeding risk in younger athletes. Athletes >35 years of age often engage in a range of athletic activities that carry traumatic risk (e.g., cycling, skiing, martial arts).
Figure 1
This figure presents point estimates from Chandran et al. of concussion rates per athletic exposure, ordered from lowest to highest, across different sport categories: collision (e.g., ice hockey, football), high contact (e.g., soccer, basketball), limited contact (e.g., baseball, swimming), and noncontact (e.g., tennis, track and field). These data illuminate the relationship between sport type and concussion rates, offering insight into decisions regarding antithrombotic use in athletes. The risk of severe intracranial hemorrhage is hypothesized to align with concussion risk across these sports. Data from Chandran A, Boltz AJ, Morris SN, et al. Epidemiology of concussions in National Collegiate Athletic Association (NCAA) sports: 2014/15-2018/19. Am J Sports Med 2022;50:526-36.
NCAA = National Collegiate Athletic Association.
Managing antithrombotic therapy in athletes requires a personalized approach balancing the risks and benefits of therapy with considerations of the underlying disease and specific sport. The shift away from a restrictive, paternalistic approach allows for greater athlete autonomy by incorporating patient preferences through shared decision making.
Venous Thromboembolism and Intermittent Dosing
Athletes are considered to have a higher risk of VTE than the general population, which has been tied to training intensity, increased risk of injuries requiring immobilization, and frequent long-haul travel.3 Anticoagulation is required for 3 months following provoked VTE, after which athletes can fully return to play without restriction. However, when unprovoked or recurrent, lifelong anticoagulation is indicated, often threatening sport eligibility.
Intermittent dosing strategies have been proposed to accommodate athletes desiring to return to competitive sporting activities after 3 months of anticoagulation therapy. Thanks to the availability of direct oral anticoagulants (DOACs), pharmacokinetic studies, and calibrated assays, such athletes can be provided with a flexible dosing regimen and maintain a low risk of VTE recurrence. Intermittent dosing strategies are based on the rationale that temporary cessation of therapy for sporting events is safe because of the very low daily risk of VTE recurrence. Therefore, consideration of once-a-day dosing timed to peak trough levels may be reasonable to enable participation in higher-risk activities using a shared decision-making approach.4,5
Atrial Fibrillation
AF is the most common arrhythmia worldwide, and endurance athletes are known to be at increased risk.6,7 Cardinal aspects of AF management include symptom control and stroke prevention. The latter requires a thoughtful approach, often supported by stroke-risk prediction scores such as CHA2DS2-VASc and bleeding-risk tools such as HAS-BLED.
In younger athletes with "lone AF," anticoagulation is rarely necessary given low thrombotic risk. However, in older athletes, as stroke risk accumulates, anticoagulation is often indicated. For nonvalvular AF, the authors recommend prompt initiation of DOAC therapy in those with elevated risk. Athletes who participate in contact sports or sports with an inherent risk of trauma (e.g., cycling) should be counseled regarding the risks of minor and catastrophic bleeding, and individualized participation plans should be generated.
Coronary Artery Disease
Athletes are not exempt from CAD, a common cause of exercise-related sudden cardiac death (SCD) in active individuals >35 years of age.8 Acute coronary syndromes are treated independent of athletic status. However, when stable CAD is present, revascularization may be considered differently in competitive athletes to decrease the risk of SCD in competition. Revascularization requires lifelong antiplatelet therapy. Consensus guidelines recommend that athletes requiring dual antiplatelet therapy (DAPT) be restricted from collision sports.9
Following revascularization in athletic individuals, the authors' approach is to counsel a staged return to exercise that includes time for recovery, rehabilitation, and retraining before full return to sport. Although this staged return varies athlete to athlete, it typically occurs over 6-12 months, overlapping with the commonly adopted timeline for optimal duration of DAPT following revascularization. When appropriate, the authors prioritize a reduction to long-term monotherapy in athletes and active individuals, particularly those with increased risk of injury and low-risk CAD presentations. Generally, the authors consider bleeding risks from low-dose aspirin monotherapy to be acceptable for most sports.
The Masters Athlete's Conundrum: Coexisting AF and CAD
Two of the most common CV conditions facing older athletes are AF and CAD, and they often coexist. Nearly 1 in 10 patients undergoing revascularization have AF. Simultaneous use of anticoagulants and antiplatelet agents to address the risks associated with AF and CAD present a clinical challenge. Those with unstable presentations are treated as having high thrombotic risk. However, for some athletes with stable presentations, low thrombotic risk, and increased bleeding risk due to their sport, P2Y12 inhibition may be discontinued in <1 year with consideration of anticoagulation monotherapy.10
Putting It All Together
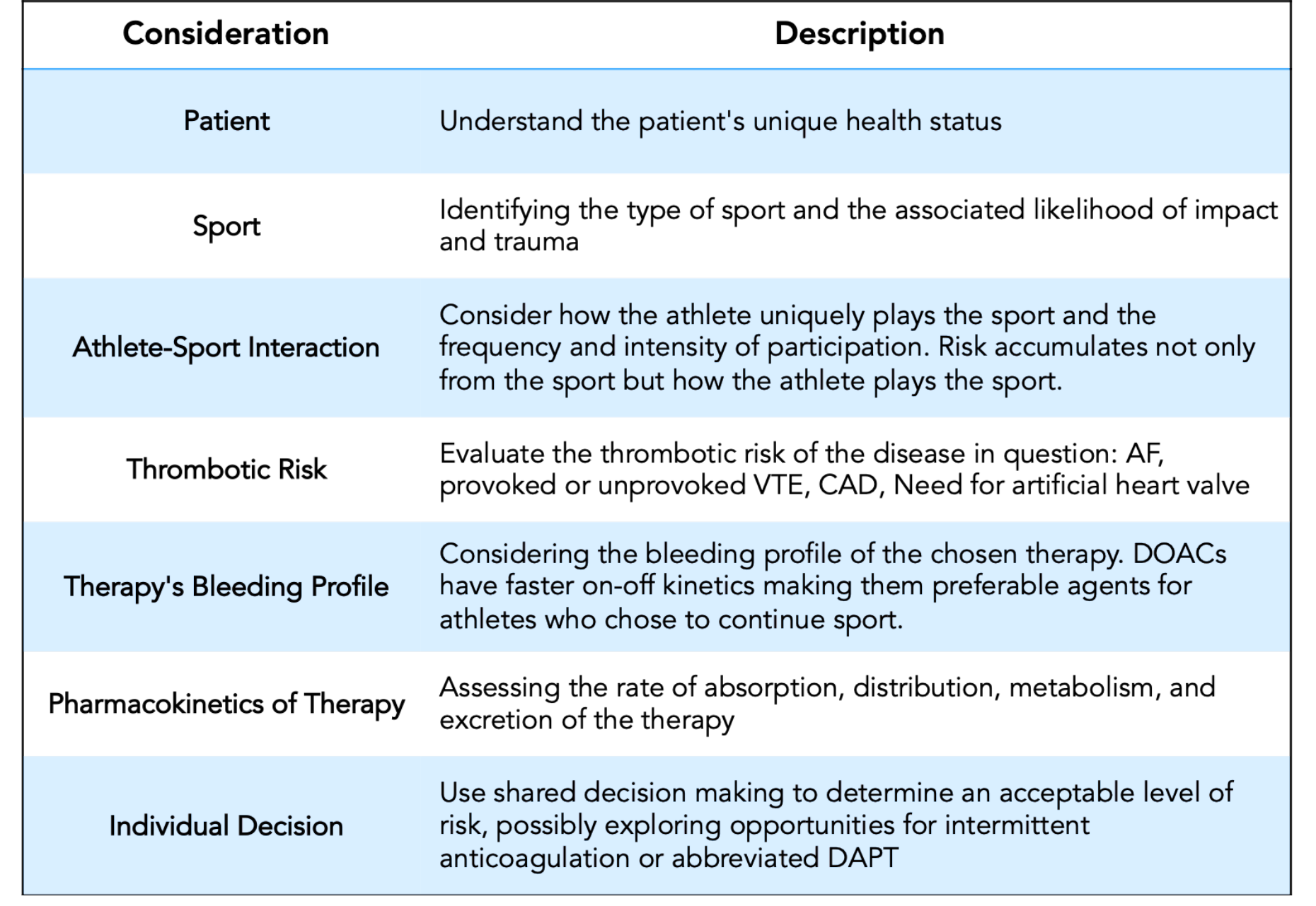
Managing antithrombotic agents in athletes requires a personalized approach that balances the risks and benefits of therapy with considerations of the underlying disease and specific sport. Thrombotic risk of the disease in question is a key consideration. The interaction between the athlete and their chosen sport is also crucial—not just which sport is played, but how the athlete uniquely plays the sport. Assessing a history of concussion may provide a sense of this interaction. Although contact sports carry inherently higher bleeding risks, noncontact sports such as cycling, skiing, climbing, and surfing pose different risks, predominantly around head injuries and falls (Table 1).
Table 1
AF = atrial fibrillation; CAD = coronary artery disease; DAPT = dual antiplatelet therapy; DOACs = direct oral anticoagulants; VTE = venous thromboembolism.
In select patients, exploring opportunities for intermittent anticoagulation under expert guidance may be reasonable. This approach could provide a balance between recommended antithrombotic therapy and potential bleeding risks inherent to sports participation.
Determining an acceptable level of risk is ultimately a personal decision for the athlete, made in collaboration with health care professionals. Decisions should be informed by health status, sporting commitments, and lifestyle preferences. Although consensus recommendations and guidelines provide a critical framework, they should serve as a starting point for a nuanced, individualized care plan.
References
- Chandran A, Boltz AJ, Morris SN, et al. Epidemiology of concussions in National Collegiate Athletic Association (NCAA) sports: 2014/15-2018/19. Am J Sports Med 2022;50:526-36.
- Zipes DP, Link MS, Ackerman MJ, Kovacs RJ, Myerburg RJ, Estes NA 3rd. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 9: arrhythmias and conduction defects: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2015;66:2412-23.
- Meyering C, Howard T. Hypercoagulability in athletes. Curr Sports Med Rep 2004;3:77-83.
- Berkowitz J, Moll S. Athletes and Anticoagulation: Return to Play After DVT/PE (ACC website). 2016. Available at: https://www.acc.org/latest-in-cardiology/articles/2016/10/19/15/13/athletes-and-anticoagulation. Accessed 08/22/2023.
- Nazha B, Pandya B, Spyropoulos AC, Kessler CM. Treatment of venous thromboembolism in elite athletes: a suggested approach to individualized anticoagulation. Semin Thromb Hemost 2018;44:813-22.
- Andersen K, Farahmand B, Ahlbom A, et al. Risk of arrhythmias in 52 755 long-distance cross-country skiers: a cohort study. Eur Heart J 2013;34:3624-31.
- Churchill TW, Baggish AL. Cardiovascular care of masters athletes. J Cardiovasc Transl Res 2020;13:313-21.
- Baggish AL, Battle RW, Beckerman JG, et al.; ACC's Sports and Exercise Council Leadership Group. Sports cardiology: core curriculum for providing cardiovascular care to competitive athletes and highly active people. J Am Coll Cardiol 2017;70:1902-18.
- Thompson PD, Myerburg RJ, Levine BD, Udelson JE, Kovacs RJ. Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task Force 8: coronary artery disease: a scientific statement from the American Heart Association and American College of Cardiology. J Am Coll Cardiol 2015;66:2406-11.
- Matoba T, Yasuda S, Kaikita K, et al.; AFIRE Investigators. Rivaroxaban monotherapy in patients with atrial fibrillation after coronary stenting: insights from the AFIRE trial. JACC Cardiovasc Interv 2021;14:2330-40.
Clinical Topics: Anticoagulation Management, Arrhythmias and Clinical EP, Pulmonary Hypertension and Venous Thromboembolism, Sports and Exercise Cardiology, Atherosclerotic Disease (CAD/PAD), Anticoagulation Management and Atrial Fibrillation, Anticoagulation Management and Venothromboembolism, Atrial Fibrillation/Supraventricular Arrhythmias
Keywords: Sports Medicine, Sports, Athletes, Fibrinolytic Agents, Platelet Aggregation Inhibitors, Return to Sport, Anticoagulants, Venous Thromboembolism, Coronary Artery Disease, Atrial Fibrillation, Hemorrhage, Risk Assessment
< Back to Listings