Advancing Cardiovascular Health Equity Through Prevention Science
Quick Takes
- Achieving optimal cardiovascular health requires a coordinated multidisciplinary and multilayer approach.
- Conscious efforts through implementing clinical interventions, leveraging technology, enhancing multidisciplinary care, and improving community engagement and health care policy are needed to mitigate inequities and achieve social justice.
Introduction
Attaining ideal cardiovascular (CV) health and improving overall well-being for individuals and communities necessitates a strong focus on preventing CV and related diseases. Prevention science aims to use evidence-based strategies to reduce disease risk factors and promote health holistically. The 2017 American Heart Association (AHA) Scientific Statement on Implementation of Prevention Science to Eliminate Health Care Inequities in Achieving CV Health examines barriers to ideal CV health, focusing on leveraging resources to reduce health care inequities and enhance preventive CV care.1 The AHA discusses interventions in health care settings, technology utilization, interdisciplinary collaborations, community engagement, and health-related government policies, providing evidence-based examples of equitable CV health.
Direct Patient Care
Health care environments that provide direct patient care are pivotal in addressing inequities and promoting effective preventive care.2 Firstly, education for the health care team is crucial and can be improved by integrating training on barriers to care and inequities into formal education for all health professionals.3 Enhancing diversity within health care settings, encompassing racial/ethnic, geographical, and gender diversity, facilitates better access to care, quality of care, and cultural awareness, fostering trust and improved CV outcomes.4 Effective communication is paramount for promoting health equity, and using language that avoids stigmatization, adopts person-first phrasing, and uses specific terms to describe subpopulations can create a holistic environment. Communication in the patient's preferred language and at their comprehension level encourages active engagement and adherence to treatment plans. Lastly, improving health literacy at the patient-care level is critical. Tailoring information to patients' literacy, language, and linguistic needs, along with promoting shared decision making, empowers them to take an active role in managing their health.
Health Care Technology
Health care technologies, including electronic medical records (EMRs) and telehealth visits, offer promising potential for enhancing preventive CV care. The benefits of technology include improved access to health records and diagnostic testing, along with enhanced communication with health care teams, leading to better longitudinal tracking and management of key health metrics. However, concerns remain about the inequality in their adoption by both patients and health systems. EMRs have varying functionality across health care settings, with cost limitations hindering their comprehensive implementation in low-resourced community-based clinics. Longitudinal data provided by EMRs are important for effectively managing chronic conditions such as hypertension and diabetes mellitus. Telehealth has seen exponential growth in health care delivery and provides an alternative and safe option for the continuation of care of chronic medical conditions.5 However, equitable implementation and access to telehealth services remain challenging and require further improvement.6 To improve CV preventive care for all, technological capacity should prioritize standards allowing low-resource communities access to high-quality internet services and virtual portals. Although technology cannot resolve all barriers to care, it serves as a valuable tool to help mitigate certain inequities.7
Multiprofessional Collaborations
Multidisciplinary approaches emphasizing collaborative care effectively reduce health care inequities by providing preventive interventions that address social determinants of health (Table 1). Evidence supports team-based care, showing significant improvements in hypertension control, especially in under-represented populations. Community health workers (CHWs), particularly in under-resourced areas, serve as frontline public health officials, bridging communities with health care systems. Engaging CHWs in a team-based care model improves CV risk factors in patients. Corporations, including pharmaceutical companies, pharmacies, and health insurance companies, can contribute to mitigating health care disparities through identification of vulnerable populations and facilitate resource allocation to areas with the most urgent needs.
Table 1: Definitions and Associated Disparities of Social Determinants of Health
| Social Determinants of Health | Definition | Associated Disparities |
| Health Literacy (HL) | The capability to obtain and understand fundamental healthcare resources and information |
|
| Neighborhood and Built Environment | Factors in a person's surroundings that impacts their quality of life (e.g., stores nearby and sense of safety in their community) |
|
| Access to Healthcare | The ability to obtain proper care, treatment, and medication from a healthcare professional |
|
| Economic Stability | A person's financial security with factors including socioeconomic status, income, and employment |
|
| Social and Community Context | The way someone is viewed in society and how this view impacts their life, especially in terms of discrimination based on race, ethnicity, gender, or sexual orientation |
|
Local Communities
Community engagement is a vital strategy for reducing and eliminating CVD inequities. Collaborative interventions involving community members have proven effective in changing health behaviors, benefiting from the community's expertise and credibility, while leveraging existing infrastructure for sustainability. Overlapping boundaries between clinical and community settings by placing health care professionals in everyday locations (e.g., grocery stores, barber shops, and schools) blurs the boundaries between health care and the community, yielding significant improvements in health inequities.8 Strengthening collaborations between federally qualified health centers and academic medical centers can also enhance access to care for individuals with lower socioeconomic status through health education programs and shared training initiatives.9 Engaging multiple stakeholders, including community leaders, patient representatives, and academic medical centers, can contribute to increased racial, ethnic, and gender diversity.3
Government Policies
Community stakeholders, local governments, and clinicians share a common interest in enhancing the health of the communities they serve, fostering an environment conducive to innovation. Government policies at both local and national levels play a significant role in reducing health care inequities and promoting ideal CV health. For example, population-level interventions, such as taxes on sugar-sweetened beverages or portion-size limitations, require support from local or state governments. The Centers for Medicare and Medicaid Services (CMS) have recently embraced health equity measures, focusing on health care disparities and improved reporting of individuals with health-related social needs as part of their quality-improvement activities.10
Conclusion
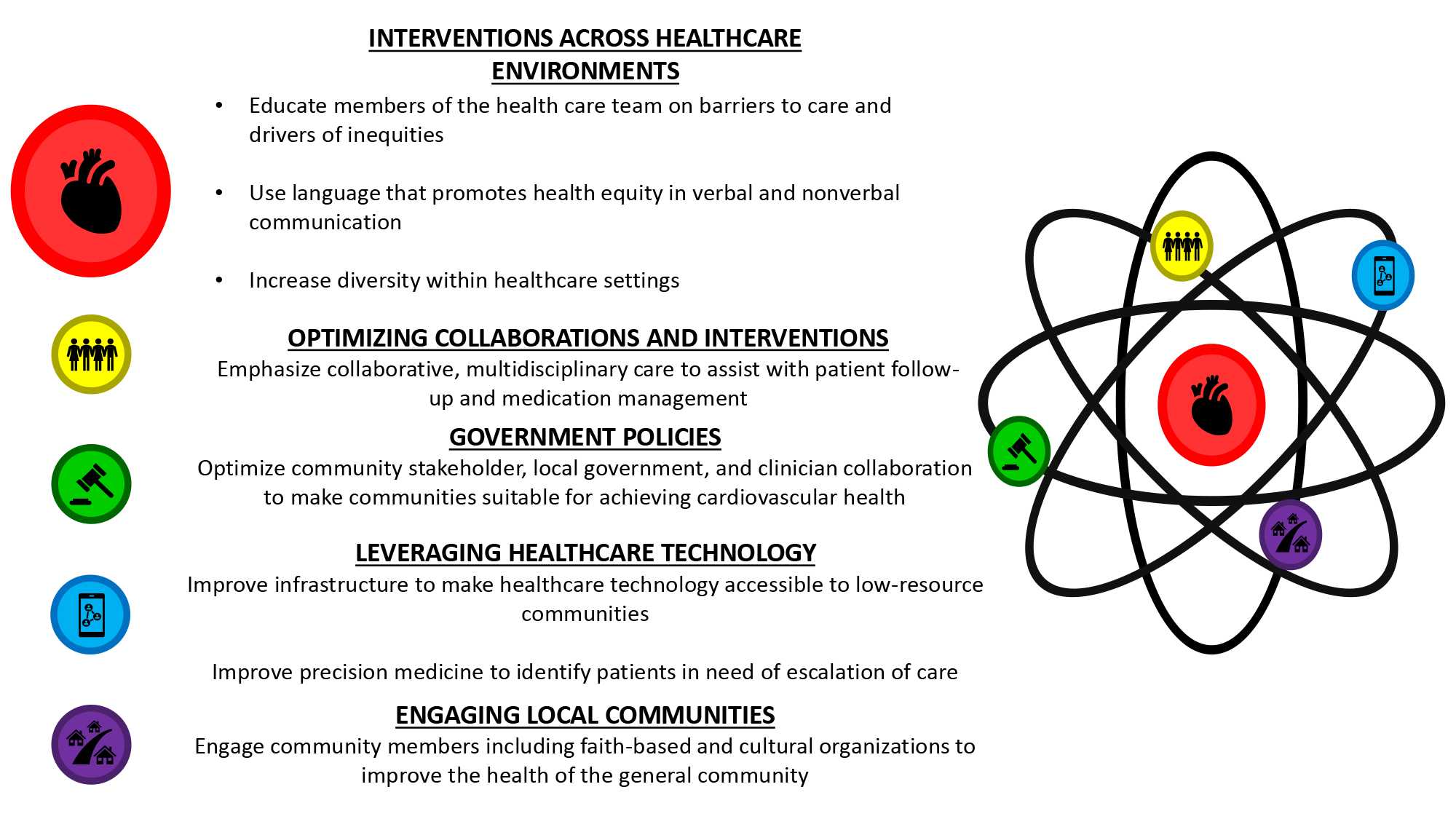
Achieving optimal CV health requires a coordinated, multidisciplinary approach. By implementing clinical interventions, leveraging technology, enhancing collaborative care across various disciplines, and augmenting community engagement alongside improvements in health care policy, inequities can be mitigated and social justice promoted within CV health care (Figure 1).
Figure 1: Interventions Across Health Care Environments
References
- Agarwala A, Patel J, Stephens J, et al.; American Heart Association Prevention Science Committee of the Council on Epidemiology and Prevention and Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, Council on Lifestyle and Cardiometabolic Health, Council on Peripheral Vascular Disease, Council on Quality of Care and Outcomes Research, Stroke Council. Implementation of prevention science to eliminate health care inequities in achieving cardiovascular health: a scientific statement from the American Heart Association. Circulation 2023;148:1183-93.
- Lloyd-Jones DM, Allen NB, Anderson CAM, et al.; American Heart Association. Life's Essential 8: updating and enhancing the American Heart Association's construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation 2022;146:e18-e43.
- Churchwell K, Elkind MSV, Benjamin RM, et al.; American Heart Association. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation 2020;142:e454-e468.
- Pittman P, Chen C, Erikson C, et al. Health workforce for health equity. Med Care 2021;59:S405-S408.
- Duffy EY, Cainzos-Achirica M, Michos ED. Primary and secondary prevention of cardiovascular disease in the era of the coronavirus pandemic. Circulation 2020;141:1943-5.
- Patel P, Dhindsa D, Eapen DJ, et al. Optimizing the potential for telehealth in cardiovascular care (in the era of COVID-19): time will tell. Am J Med 2021;134:945-51.
- Sieck CJ, Sheon A, Ancker JS, Castek J, Callahan B, Siefer A. Digital inclusion as a social determinant of health. NPJ Digit Med 2021;4:52.
- Victor RG, Lynch K, Li N, et al. A cluster-randomized trial of blood-pressure reduction in Black barbershops. N Engl J Med 2018;378:1291-301.
- Eck C, Biola H, Hayes T, et al. Efficacy of hypertension self-management classes among patients at a federally qualified health center. Prev Chronic Dis 2021;18:E70.
- Sandhu S, Liu M, Wadhera RK. Hospitals and health equity - translating measurement into action. N Engl J Med 2022;387:2395-7.
Clinical Topics: Prevention
Keywords: Primary Prevention, Secondary Prevention, Health Equity, Health Policy, Social Determinants of Health
< Back to Listings