New ACC/AHA Guideline Focuses on Diagnosis, Management of AFib
The newest clinical guideline released by the ACC and the American Heart Association (AHA) provides new and updated recommendations for preventing and optimally managing atrial fibrillation (AFib).
The 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation updates two separate guidelines from 2014 and 2019, respectively, and includes new recommendations addressing AFib and thromboembolic risk assessment, anticoagulation, left atrial appendage occlusion, AFib catheter or surgical ablation, as well as risk factor modification and prevention.
Among the highlights, are a stronger, more prescriptive focus on healthy lifestyle habits to prevent or lessen the burden of AFib across the disease continuum, including weight loss, physical activity, smoking cessation, alcohol moderation, hypertension and other comorbidities. Use of clinical care pathways, such as nurse-led AFib clinics, is also reasonable, according to the guideline, when it comes to "promoting comprehensive, team-based care and to enhance adherence to evidence-based therapies for AFib and associated conditions."
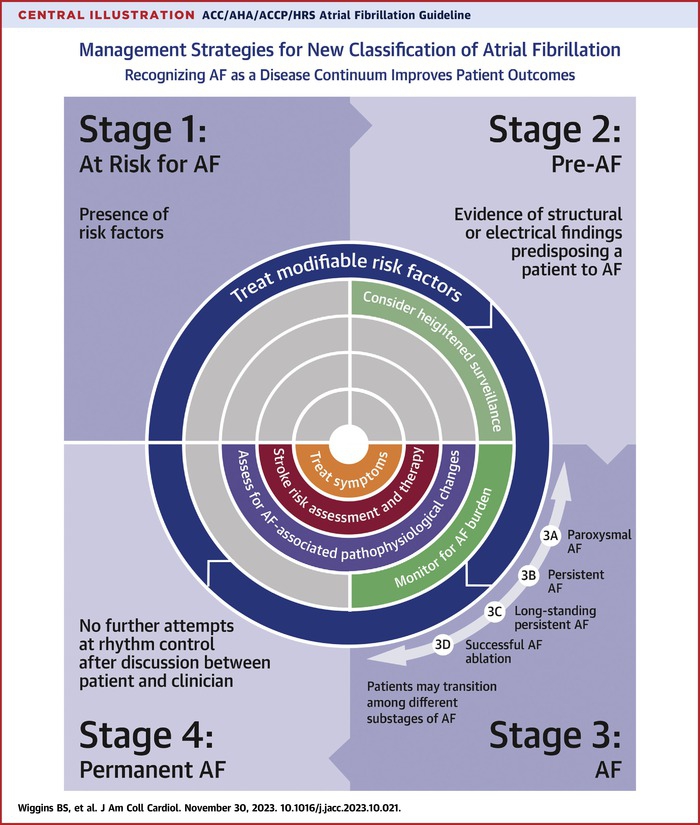
The guideline also sets forth a new way to classify AFib, using stages that reinforce the continuum of the disease and underscore the need to use a variety of strategies, including prevention, lifestyle and risk factor modification, screening, and therapy. Previously, AFib was primarily classified based only on arrhythmia duration, which, although useful, tended to emphasize specific therapeutic interventions as opposed to a more holistic and multidisciplinary management approach, according to the authors.
Early and more aggressive rhythm control in general is also addressed, along with upgraded recommendations for catheter ablation as first-line therapy to prevent disease progression in select patients, including those with heart failure with reduced ejection fraction. The updated recommendation is the result of recent randomized studies that have demonstrated the superiority of catheter ablation over drug therapy for rhythm control.
Flexibility in using clinical risk scores and expanding beyond CHA2DS2-VASc for prediction of stroke and systemic embolism are also a focus of the new guideline, as is consideration of stroke risk modifiers that may inform shared decision-making conversations between patients and clinicians. Updated guidance on the management of heart rate and rhythm medications, use of anticoagulants, and when to temporarily pause or stop these therapies is also a focus of the new guideline. Additionally, left atrial appendage occlusion devices receive higher level Class of Recommendation, based on new data showing safety and efficacy.
"The new guideline reinforces the urgent need to approach AFib as a complex cardiovascular condition that requires disease prevention, risk factor modification, as well as optimizing therapies and patients' access to care and ongoing, long-term management," says Jose Joglar, MD, FACC, chair of the writing committee. "This is a complex disease. It's not just an isolated disorder of the heart's rhythm, and we now know that the longer someone is in AFib, the harder it is to get them back to normal sinus rhythm."
Clinical Topics: Arrhythmias and Clinical EP, Atrial Fibrillation/Supraventricular Arrhythmias
Keywords: Atrial Fibrillation, Guideline, Guidelines as Topic