The Expert's Approach to Managing Cardiovascular Risk Among Athletes Using Anabolic-Androgenic Steroids
Quick Takes
- The use of anabolic-androgenic steroids (AAS) is increasing among recreational athletes.
- People who take AAS maintain supraphysiological androgen levels, which have been associated with several deleterious cardiovascular (CV) consequences.
- CV risk evaluation among people taking AAS is important, and sports cardiologists should be aware of strategies to discontinue/wean AAS.
Introduction
The use of anabolic-androgenic steroids (AAS) has become widespread, with an estimated tens of millions of people worldwide using these drugs.1 An "androgen" is any natural or synthetic steroid hormone that binds to androgen receptors to induce the development of male primary and secondary sexual characteristics and other effects. The term "anabolic" refers to the specific capability of enhancing somatic tissue growth, such as skeletal muscle hypertrophy. AAS are a class of hormones that encompass testosterone along with its synthetic derivatives (Table 1).2 Testosterone and other AAS have been employed therapeutically for the treatment of selective medical conditions, including male hypogonadism, anemia, and muscle wasting diseases.1 Historically, illicit use of AAS was limited to professional athletes and bodybuilders, but currently most people taking AAS are recreational athletes.3 Unlike in older, nonathletic individuals taking testosterone replacement therapy, people taking AAS typically maintain supraphysiological androgen levels, which have potentially serious adverse cardiovascular (CV) and non-CV effects. Common dosing strategies are outlined in Table 1; people taking AAS may exceed these ranges in the pursuit of extreme muscle hypertrophy. Furthermore, AAS are typically taken in cycles, with deliberate off-drug periods, to decrease potential liver toxicity and adverse effects. This expert analysis will explore the relationship between AAS use and CV risk and provide an approach to the management of AAS in the sports cardiology clinic.
Table 1: Common Doses for Anabolic-Androgenic Steroids Used by Recreational Athletes.2 Courtesy of Meagher SP, Chandra MS, Irwig MS, Rao P.
| Anabolic-Androgenic Steroid | Route of Administration (Interval) | Dose |
| Testosterone cypionate | Injectable (weekly) | 200-600 mg |
| Testosterone enanthate | Injectable (weekly) | 200-600 mg |
| Testosterone propionate | Injectable (weekly) | 150-300 mg |
| Testosterone suspension | Injectable (weekly) | 150-700 mg |
| Trenbolone acetate | Injectable (weekly) | 150-300 mg |
| Trenbolone enanthate | Injectable (weekly) | 200-300 mg |
| Boldenone | Injectable (weekly) | 200-400 mg |
| Drostanolone | Injectable (weekly) | 300-450 mg |
| Methenolone | Injectable (weekly) | 200-400 mg |
| Nandrolone | Injectable (weekly) | 200-400 mg |
| Stanozolol | Injectable (weekly) | 150-700 mg |
| Fluoxymesterone | Oral (daily) | 20-40 mg |
| Methandrostenolone | Oral (daily) | 20-40 mg |
| Mesterolone | Oral (daily) | 50-100 mg |
| Oxandrolone | Oral (daily) | 20-40 mg |
| Oxymetholone | Oral (daily) | 50-100 mg |
| Stanozolol | Oral (daily) | 20-50 mg |
| Testosterone undecanoate | Oral (daily) | 80-160 mg |
| Chlorodehydromethyltestosterone | Oral (daily) | 20-80 mg |
Cardiovascular Disease Risk Factors
AAS use is associated with unfavorable changes in plasma lipoprotein levels and blood pressure (BP) compared with measurements in people who do not take AAS.4 The results of the prospective HAARLEM (Health risks of Anabolic Androgenic steRoid use by maLE aMateur athletes) study, which included 100 men (≥18 years of age) performing an AAS cycle, showed that mean systolic BP increased by 6.87 mm Hg and diastolic BP by 3.17 mm Hg after cycle completion.5 This study's results also confirmed previous observations reporting an association between AAS use and elevated low-density lipoprotein cholesterol levels, elevated apolipoprotein (b) levels, and decreased high-density lipoprotein cholesterol (HDL-C) levels.5 These changes in CV risk factors were reversible after cessation of AAS in this cohort.
Coronary Artery Disease
An estimated 3% of people taking AAS develop an acute myocardial infarction (MI) before 50 years of age.4 One of the most instructive studies on AAS use and CV risk assessed 86 people with long-term AAS use (mean lifetime duration of AAS, 7 years) and 54 people not taking AAS using coronary computed tomography angiography.4 In this study, people taking AAS were more likely to develop higher coronary plaque volume and to experience higher rates of early MIs than were people not taking AAS.4 Importantly, the investigators demonstrated a dose-dependent relationship between the cumulative lifetime duration of AAS use and the severity of atherosclerosis. The proposed mechanism is likely multifactorial, involving atherogenic lipid profiles, thrombosis, and possibly vasospasm.
Subclinical Cardiovascular Remodeling and Cardiomyopathy
Akin to their effect on skeletal myocytes, AAS may exert similar effects on cardiomyocytes. The results of several studies demonstrate a positive association between AAS use and left ventricular (LV) wall thickness, LV mass, and concentric hypertrophy.4,6,7 Most of the increased LV mass is due to matrix collagen deposition and fibrosis, which may increase the risk of subsequent cardiomyopathy.8 Indeed, study investigators have also reported an association of AAS use with LV systolic and diastolic dysfunction.4,8,9 Although case reports have shown reversibility of AAS-associated cardiomyopathy, whether subclinical CV remodeling is also reversible following cessation of AAS remains unclear.
Sudden Cardiac Death
Numerous case reports have attributed sudden cardiac death in athletes to AAS; however, there is limited high-quality evidence to rigorously assess causality. A Danish retrospective cohort study compared all-cause mortality rates in 545 men with laboratory-confirmed AAS use with 5,450 healthy volunteers consisting of randomly selected, age-matched individuals; the investigators found a threefold higher mortality rate among those taking AAS.10 Several hypotheses have been proposed to explain this finding, but it has yet to be fully elucidated.
Evaluation and Management
In the sports cardiology clinic, the ultimate goals are to educate people taking AAS about the harms of chronic supraphysiological androgen levels and to minimize their risk of serious CV and non-CV disease. To achieve this, it is imperative to create a safe and nonjudgmental environment to allow an open discussion of AAS use. Indeed, people taking AAS seldom disclose their use to clinicians, and it often only comes to attention after the development of serious adverse effects.
During the consultation, clinicians should carefully assess the lifetime exposure to AAS, including the specific type of AAS, its frequency and route of administration, the source of the supply, and whether the athlete has been taking multiple AAS simultaneously (referred to as "stacking") (Figure 1).
Figure 1: Evaluation and Management of Anabolic-Androgenic Steroids in Sports Cardiology. Courtesy of Meagher SP, Chandra MS, Irwig MS, Rao P.
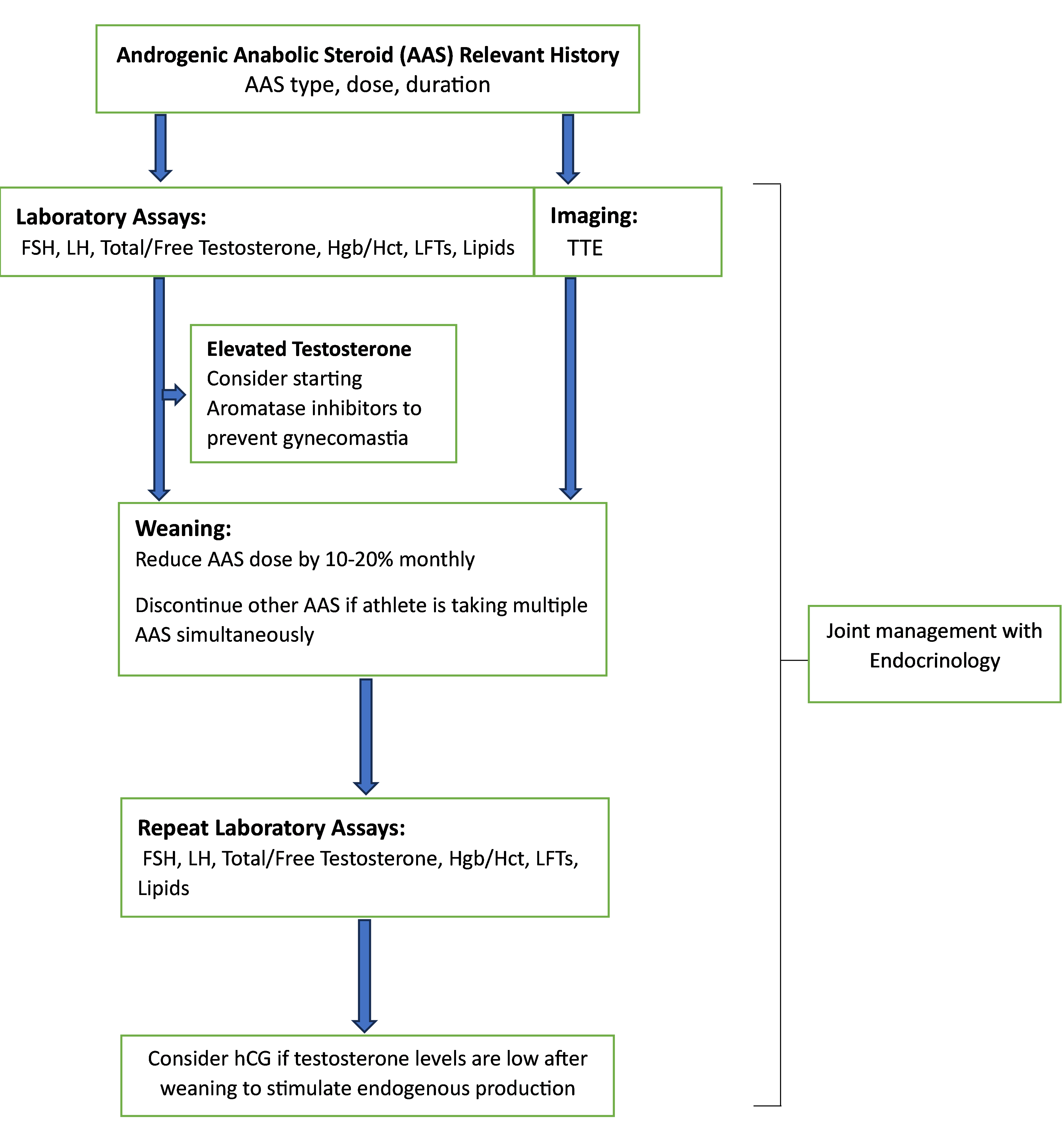
In addition to measuring blood pressure in the clinic, when laboratory testing is warranted, the authors measure total testosterone, free testosterone, follicle-stimulating hormone (FSH), and luteinizing hormone (LH) levels. Although testing for AAS may be available through large commercial laboratories, these urine tests are often not routinely ordered because they are not covered by health insurance and patients would need to consent to pay out of pocket. Instead, indirect indictors of AAS use would include low levels of HDL-C, LH, FSH, and sex-hormone binding globulin; elevated levels of aspartate aminotransferase and alanine aminotransferase; and elevated levels of testosterone and estradiol (depending on whether testosterone is used). The authors also recommend obtaining a complete blood count to assess for erythrocytosis, lipid profile for dyslipidemia, liver function tests for liver damage, and an echocardiogram for LV chamber size, thickness, and function. These data are crucial for risk stratification and may help steer the athlete toward weaning off AAS.
If the athlete is interested in discontinuing AAS, it is important to recognize that abrupt termination of AAS may be associated with multiple symptoms, including depression, low libido, and erectile dysfunction. For noncompetitive or recreational athletes taking multiple AAS, including testosterone, the authors recommend maintaining and gradually tapering the testosterone dose while discontinuing other AAS.11 One can try reducing the testosterone dose by 10-20% every month or go slower if the patient does not tolerate the taper.11 An aromatase inhibitor can be considered, whereas the testosterone dose is supraphysiological to avoid gynecomastia. Symptoms following withdrawal of testosterone or too rapid a taper may lead people to restart the AAS, which can become a vicious cycle. For men who have tapered off AAS or who are on low doses, human chorionic gonadotropin is sometimes used to stimulate endogenous production of testosterone by the Leydig cells (typical dose: 1000-2000 IU subcutaneously two to three times weekly).11 Importantly, for competitive athletes (for whom AAS are banned), immediate discontinuation of AAS is required, often without the use of any hormone therapy to mitigate against AAS withdrawal syndrome.
Conclusion
Exogenous AAS use is a growing public health concern among predominantly male recreational athletes, with its true prevalence underestimated given the typical clandestine nature of its use. Supraphysiological dosing of AAS have been linked to—and is likely causal for—several deleterious CV and non-CV outcomes. Fortunately, subclinical CV disease may be reversible. However, discontinuing AAS can be challenging because few athletes seek treatment, and there is limited guidance for clinicians to navigate this process with their patient-athletes. Further research is needed in this area to better understand the long-term consequences of chronic AAS use and to help provide better care for these individuals.
References
- Kanayama G, Pope HG Jr. History and epidemiology of anabolic androgens in athletes and non-athletes. Mol Cell Endocrinol 2018;464:4-13.
- McCullough D, Webb R, Enright KJ, et al. How the love of muscle can break a heart: impact of anabolic androgenic steroids on skeletal muscle hypertrophy, metabolic and cardiovascular health. Rev Endocr Metab Disord 2021;22:389-405.
- Sagoe D, Pallesen S. Androgen abuse epidemiology. Curr Opin Endocrinol Diabetes Obes 2018;25:185-94.
- Baggish AL, Weiner RB, Kanayama G, et al. Cardiovascular toxicity of illicit anabolic-androgenic steroid use. Circulation 2017;135:1991-2002.
- Smit DL, Grefhorst A, Buijs MM, de Hon O, den Heijer M, de Ronde W. Prospective study on blood pressure, lipid metabolism and erythrocytosis during and after androgen abuse. Andrologia 2022;54:[ePub ahead of print].
- Rasmussen JJ, Schou M, Madsen PL, et al. Cardiac systolic dysfunction in past illicit users of anabolic androgenic steroids. Am Heart J 2018;203:49-56.
- Fyksen TS, Vanberg P, Gjesdal K, et al. Cardiovascular phenotype of long‐term anabolic‐androgenic steroid abusers compared with strength‐trained athletes. Scand J Med Sci Sports 2022;32:1170-81.
- Fadah K, Gopi G, Lingireddy A, Blumer V, Dewald T, Mentz RJ. Anabolic androgenic steroids and cardiomyopathy: an update. Front Cardiovasc Med 2023;10:[ePub ahead of print].
- Smit DL, Voogel AJ, den Heijer M, de Ronde W. Anabolic androgenic steroids induce reversible left ventricular hypertrophy and cardiac dysfunction. Echocardiography results of the HAARLEM study. Front Reprod Health 2021;3:[ePub ahead of print].
- Horwitz H, Andersen JT, Dalhoff KP. Health consequences of androgenic anabolic steroid use. J Intern Med 2019;285:333-40.
- Anawalt BD. Diagnosis and management of anabolic androgenic steroid use. J Clin Endocrinol Metab 2019;104:2490-500.
Clinical Topics: Diabetes and Cardiometabolic Disease, Prevention, Sports and Exercise Cardiology, Exercise
Keywords: Sports, Exercise, Athletes, Steroids, Anabolic Agents, Athletic Performance, Testosterone