RESHAPE-HF2: Impact of M-TEER on Patients With FMR and Symptomatic HF
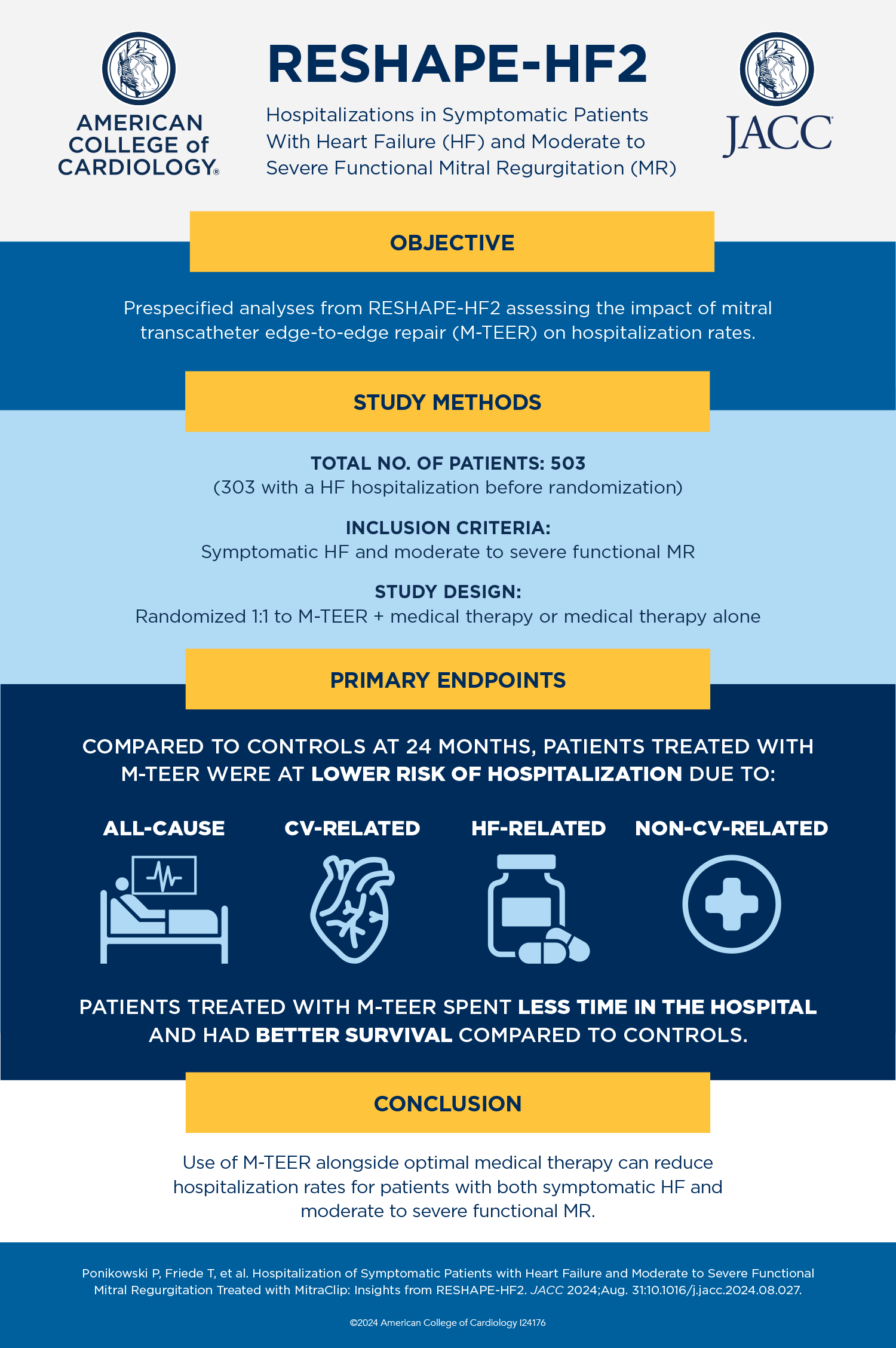
In patients with symptomatic heart failure (HF) and moderate to severe functional mitral regurgitation (FMR), mitral transcatheter edge-to-edge repair (M-TEER) reduced cardiovascular death and heart failure (HF)-related hospitalizations with improved health status, based on results of the RESHAPE-HF2 trial presented at ESC Congress 2024 in London and simultaneously published in the New England Journal of Medicine. Patients with recent HF hospitalizations prior to undergoing M-TEER saw even greater benefits, according to a sub-analysis published in JACC.
In RESHAPE-HF2, 505 patients from 30 sites across nine countries were randomized to either M-TEER in addition to medical therapy or medical therapy alone. All patients had signs and symptoms of HF despite receiving guideline-recommended medical therapy and an left ventricular ejection fraction between 20% and 50%. In addition, all were either recently hospitalized for HF or had elevated natriuretic peptide plasma concentrations within the previous 90 days and were not recommended for mitral surgery.
Overall results at 24 months showed the rate of total hospitalizations for HF and cardiovascular death was significantly lower among the M-TEER group (37.0 per 100 patient-years vs. 58.9 per 100 patient-years, respectively. The rate of total HF-related hospitalizations within 24 months was significantly reduced by 41% in the M-TEER group compared with the medical therapy alone group (26.9 per 100 patient-years vs. 57.8 per 100 patient-years).
"RESHAPE-HF2 now provides additional compelling evidence for using M-TEER over optimal medical therapy alone, which will help to guide medical decision-making," said Principal Investigator Stefan Anker, MD.
In the sub-analysis, which looked specifically at the impact of M-TEER on hospitalization rates, researchers Piotr Ponikowski, MD; Tim Friede, PhD, et al., found that patients assigned to M-TEER "had better symptom status throughout the study and they had lower rates of all-cause, cardiovascular-related, and HF-related hospitalizations rates at 24 months." Patients in the M-TEER group also lost fewer days due to death or HF-related hospitalization (13.9% vs. 17.4%) and had a better NYHA functional class at 30 days and six, 12 and 24 months of follow-up.
Ponikowski, Fried and colleagues also noted that among the 333 patients who were hospitalized for HF prior to the study, M-TEER was associated with even greater reductions in total HF hospitalizations and cardiovascular deaths within 24 months. "The results indicate that a broader application of M-TEER in addition to optimal [guideline-directed medical therapy] should be considered among patients with symptomatic HF and moderate to severe FMR, particularly in those with a history of a recent hospitalization for HF," they write.
RESHAPE-HF2 is among three randomized controlled trials comparing treatment with M-TEER plus medical therapy to medical therapy alone in patients with that has been conducted in patients with HF and FMR. A meta-analysis comparing its results with that of the other two trials – COAPT and MITRA-FR – can be found in JACC. The authors note that interpretation of the meta-analysis results. "Given the overall heterogeneity of results, an individual patient-level meta-analysis is urgently needed in the near future and may provide information that aids in interpreting the totality of the data" they write. "In the meantime, the public dialogue and uncertainty about who benefits from this intervention will likely continue. Access two separate editorial comments adding to this public dialogue and also published in JACC, here and here.
Clinical Topics: Heart Failure and Cardiomyopathies, Valvular Heart Disease, Acute Heart Failure, Mitral Regurgitation
Keywords: ESC Congress, ESC24, Mitral Valve Insufficiency, Heart Failure