How Do the 2025-2030 Dietary Guidelines For Americans Measure Up For Cardiovascular Health?
Quick Takes
- The 2025-2030 Dietary Guidelines for Americans include both evidence-based advances and some recommendations that diverge from those of the 2025 Dietary Guideline Advisory Committee.
- Plant-forward eating patterns remain the most consistent dietary strategy for reducing cardiovascular risk.
- Clinicians should use simple tools and knowledge to proactively translate the DGA into clear, evidence-based guidance for patients.
The Dietary Guidelines for Americans (DGA), released jointly by the secretaries of the U.S. Department of Health and Human Services (HHS) and U.S. Department of Agriculture (USDA) every 5 years, are a major driver of food policy, diet quality, and cardiovascular (CV) health in the population. As in prior years, the 2025-2030 DGA was preceded by a 2025 Dietary Guideline Advisory Committee (DGAC) evidentiary review compiled by a panel of independent nutrition experts.1,2 The 2025-2030 DGA will be used by policymakers to develop nutrition programs (including the National School Lunch Program [NSLP]; Special Supplemental Nutrition Program for Women, Infants, and Children [WIC]; and Supplemental Nutrition Assistance Program [SNAP]) and by health care professionals, nutrition educators, the food industry, the media, and the public. Given their broad reach, the 2025-2030 DGA will significantly impact the dietary practices of Americans.
The American College of Cardiology (ACC) Prevention of CV Disease Section's Nutrition & Lifestyle Work Group reviewed the 2025 DGAC report and 2025-2030 DGA, and summarized their findings for the ACC community in this expert analysis.1,2
A Focus on the Diet-Driven Health Crisis
More than 80% of health care dollars in the United States are now spent on treating chronic illness, a large proportion of which is diet driven: 70% of US adults have overweight or obesity, one in three have prediabetes, and 45% of cardiometabolic deaths (including heart disease, stroke, and diabetes mellitus) are now linked to poor diet.3 Overconsumption of nutrient-poor, calorie-dense, ultraprocessed, salt- and sugar-laden foods and beverages plays a major role.3 The 2025-2030 DGA directly confronts this crisis, taking a strong stance on what needs to be removed (added sugars, refined grains, and highly processed foods) and what needs to be put back in ("real foods"). The guideline emphasizes the "real foods" promoted in other recent guidelines (fruits, vegetables, and whole grains) and makes new recommendations regarding protein and fat.
Evidence-Based 2025-2030 DGA Recommendations
- Eat the right amount of calories;
- Prioritize high-quality, nutrient-dense protein with no additives at every meal;
- When consuming dairy, avoid versions with added sugars;
- Eat mostly whole grains and limit refined grains and other refined carbohydrates;
- Eat vegetables and fruits throughout the day;
- Incorporate foods with healthy fats, as well as liquid oils such as olive oil, and limit saturated fats to <10% of daily calories;
- Limit highly processed foods;
- Limit added sugars to <10 g per meal, <2.5-5 g per product, and <10% of daily calories;
- Limit dietary sodium to <2,300 mg/day; and
- Limit alcoholic beverages.
Other 2025-2030 DGA Recommendations
New Protein Recommendations
The 2025-2030 DGA recommend prioritizing protein at every meal, raising the current Recommended Dietary Allowance set by the National Academy of Sciences (NAS) from 0.8 g/kg of body weight per day in healthy adults <75 years of age to 1.2-1.6 g/kg of body weight per day, a shift not included in the 2025 DGAC report.2 The 2025-2030 DGA recommend consuming "a variety of protein foods from animal sources, including eggs, poultry, seafood, and red meat," graphically showing red meat in this section and secondarily listing "plant-sourced protein foods, including beans, peas, lentils, legumes, nuts, seeds, and soy."1
Because plant proteins like beans, peas and lentils, and nuts and soy, as well as seafood and dairy sources, have demonstrated greater health benefits than red and processed meats,2 and the latter have also been linked to gut dysbiosis, inflammation, diabetes mellitus and several cancers,4,5 plant protein sources should be emphasized to patients.
New Saturated Fat Recommendations
The 2025-2030 DGA retain the limit on saturated fat at ≤10% of daily calories. They also advise consuming "healthy fats [from] meat, poultry, eggs, omega-3-rich seafood, nuts, seeds, full-fat dairy, olives, and avocados"; other fats "with essential fatty acids, such as olive oil" (the only plant oil listed and a lesser source of essential fatty acids than others); and "other options [including] butter or beef fat (tallow)."1 Some of these recommendations are not evidence based. Data from feeding trials and/or cohort studies show that saturated fats, especially butter, and beef fat to a lesser extent, raise low-density lipoprotein cholesterol (LDL-C) levels compared with olive oil, and that higher butter versus liquid plant oil intake is associated with higher risks of death from all-causes and CV disease.6,7 Regarding dairy fat from whole milk, yogurt, and cheese, although cheese raises LDL-C compared with unsaturated fat sources, dairy food consumption has not been associated with increased CV risk,8 suggesting possible differences in the health effects of fat from dairy versus butter or red meat, and the need for more research.
In short, evidence from feeding trials and/or cohort studies does not support promotion of butter or beef tallow. Moreover, if the newly recommended servings of animal protein foods (e.g., meats and whole-fat dairy) and proposed "healthy fats" (e.g., butter and beef tallow) are incorporated into the diet, saturated fat intake will exceed 10% of daily calories.
A New Food Graphic
The graphic published with the 2025-2030 DGA, although meant to be a symmetric triangle, can also be misinterpreted as an inverted food pyramid with steak, meat, ground meat, whole milk, and cheese, along with fruits and vegetables, at the top, visually shifting the recommended diet to animal protein–predominant foods. Although legumes (beans) and nuts appear in the pyramid, they are de-emphasized, and soy foods, a major source of plant protein, are absent.1
Without clear accompanying communication materials, the 2025-2030 DGA graphic may confuse some Americans. Ultimately, unprocessed, fiber- and nutrient-rich plant foods featured in vegetarian, whole-food plant-based, Mediterranean, and DASH (Dietary Approaches to Stop Hypertension) diets are optimal for CV health, cancer reduction, and longevity.9,10
Recommendations for Counseling Patients and Peers
The ACC Nutrition & Lifestyle Work Group suggests open discussions with patients with CV conditions about the strengths of the 2025-2030 DGA and areas of question. A counterclockwise turn of the food pyramid can visually emphasize whole, unprocessed plant foods. The Harvard T. H. Chan School of Public Health's Healthy Eating Plate model (Figure 1), downloadable in 21 languages, can also be used to convey the most evidence-based balance of foods for health and disease prevention. Both can help jumpstart evidence-based messaging surrounding the guidelines, which will be crucial for their translation into improved health for patients with CV conditions and all Americans.
Figure 1: Healthy Eating Plate Model
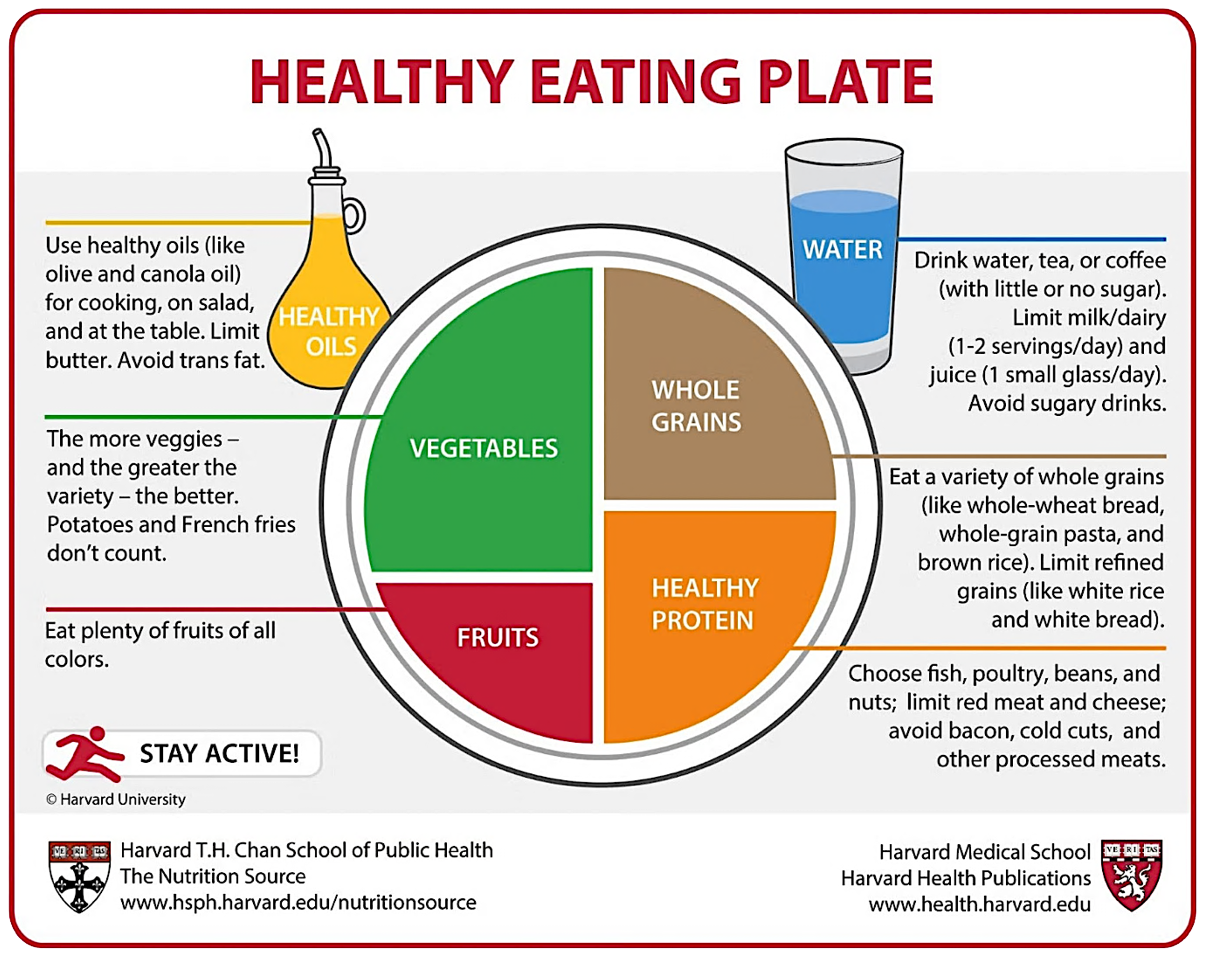
Adapted with permission from Harvard T. H. Chan School of Public Health. Healthy Eating Plate (Harvard T. H. Chan School of Public Health website). 2023. Available at: https://nutritionsource.hsph.harvard.edu/healthy-eating-plate/. Accessed 01/21/2026.
References
- U.S. Department of Health and Human Services, U.S. Department of Agriculture. Dietary Guidelines for Americans, 2025-2030 (RealFood.gov website). Available at: https://cdn.realfood.gov/DGA.pdf. Accessed 01/21/2026.
- U.S. Department of Health and Human Services, U.S. Department of Agriculture. Scientific Report of the 2025 Dietary Guidelines Advisory Committee: Advisory Report to the Secretary of Health and Human Services and Secretary of Agriculture (Dietary Guidelines for Americans website). Available at: https://www.dietaryguidelines.gov/2025-advisory-committee-report#:~:text=The%20Scientific%20Report%20of%20the,and%20is%20now%20available%20online. Accessed 01/21/2026.
- Micha R, Peñalvo JL, Cudhea F, Imamura F, Rehm CD, Mozaffarian D. Association between dietary factors and mortality from heart disease, stroke, and type 2 diabetes in the United States. JAMA. 2017;317(9):912-924. doi:10.1001/jama.2017.0947
- Li C, Bishop TRP, Imamura F, et al. Meat consumption and incident type 2 diabetes: an individual-participant federated meta-analysis of 1·97 million adults with 100 000 incident cases from 31 cohorts in 20 countries. Lancet Diabetes Endocrinol. 2024;12(9):619-630. doi:10.1016/S2213-8587(24)00179-7
- Farvid MS, Sidahmed E, Spence ND, Mante Angua K, Rosner BA, Barnett JB. Consumption of red meat and processed meat and cancer incidence: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. 2021;36(9):937-951. doi:10.1007/s10654-021-00741-9
- Kim Y, Je Y, Giovannucci EL. Association between dietary fat intake and mortality from all-causes, cardiovascular disease, and cancer: a systematic review and meta-analysis of prospective cohort studies. Clin Nutr. 2021;40(3):1060-1070. doi:10.1016/j.clnu.2020.07.007
- Zhang Y, Chadaideh KS, Li Y, Li Y, Gu X, Liu Y, et al. Butter and plant-based oils intake and mortality. JAMA Intern Med. 2025;185(5):549-560. doi:10.1001/jamainternmed.2025.0205
- Kiesswetter E, Neuenschwander M, Stadelmaier J, et al. Substitution of dairy products and risk of death and cardiometabolic diseases: a systematic review and meta-analysis of prospective studies. Curr Dev Nutr. 2024;8(5):102159. Published 2024 Apr 23. doi:10.1016/j.cdnut.2024.102159
- Lichtenstein AH, Appel LJ, Vadiveloo M, et al. 2021 dietary guidance to improve cardiovascular health: a scientific statement from the American Heart Association. Circulation. 2021;144(23):e472-e487. doi:10.1161/CIR.0000000000001031
- Shan Z, Wang F, Li Y, et al. Healthy eating patterns and risk of total and cause-specific mortality. JAMA Intern Med. 2023;183(2):142-153. doi:10.1001/jamainternmed.2022.6117
Clinical Topics: Prevention
Keywords: Diet, Food, and Nutrition, Nutrition Policy, Guidelines as Topic