Are Certain Adverse Pregnancy Outcomes Associated With Long-Term Increased Risk of HF?
Women who experienced any of five major adverse pregnancy outcomes have increased risk of heart failure (HF) up to 46 years later and need early preventive actions and long-term clinical care to reduce that risk, according to results from a national cohort and co-sibling study published Jan. 22 in JACC: Heart Failure.
Casey Crump, MD, PhD, et al., conducted a national cohort study using the Swedish Medical Birth Register to examine five major adverse pregnancy outcomes and their relationship to long-term risks of HF. The study consisted of all 2,201,638 women with a singleton delivery in Sweden from 1973 to 2015 with no prior diagnosis of HF, followed for HF from nationwide outpatient and inpatient diagnoses through 2018.
Cox regression of prenatal and birth records was used to compute the five major adverse pregnancy outcomes, which included preterm delivery, small for gestational age, preeclampsia, other hypertensive disorders, and gestational diabetes. The authors also performed co-sibling analyses for potential confounding by shared familial (genetic or environmental) factors.
Results of the study showed that all five adverse pregnancy outcomes were independently associated with long-term increased HF risk. In 48 million person-years of follow-up, 66,774 women (30%) experienced an adverse pregnancy outcome, and 19,922 (0.9%) women with a median age of 61 years were diagnosed with HF.
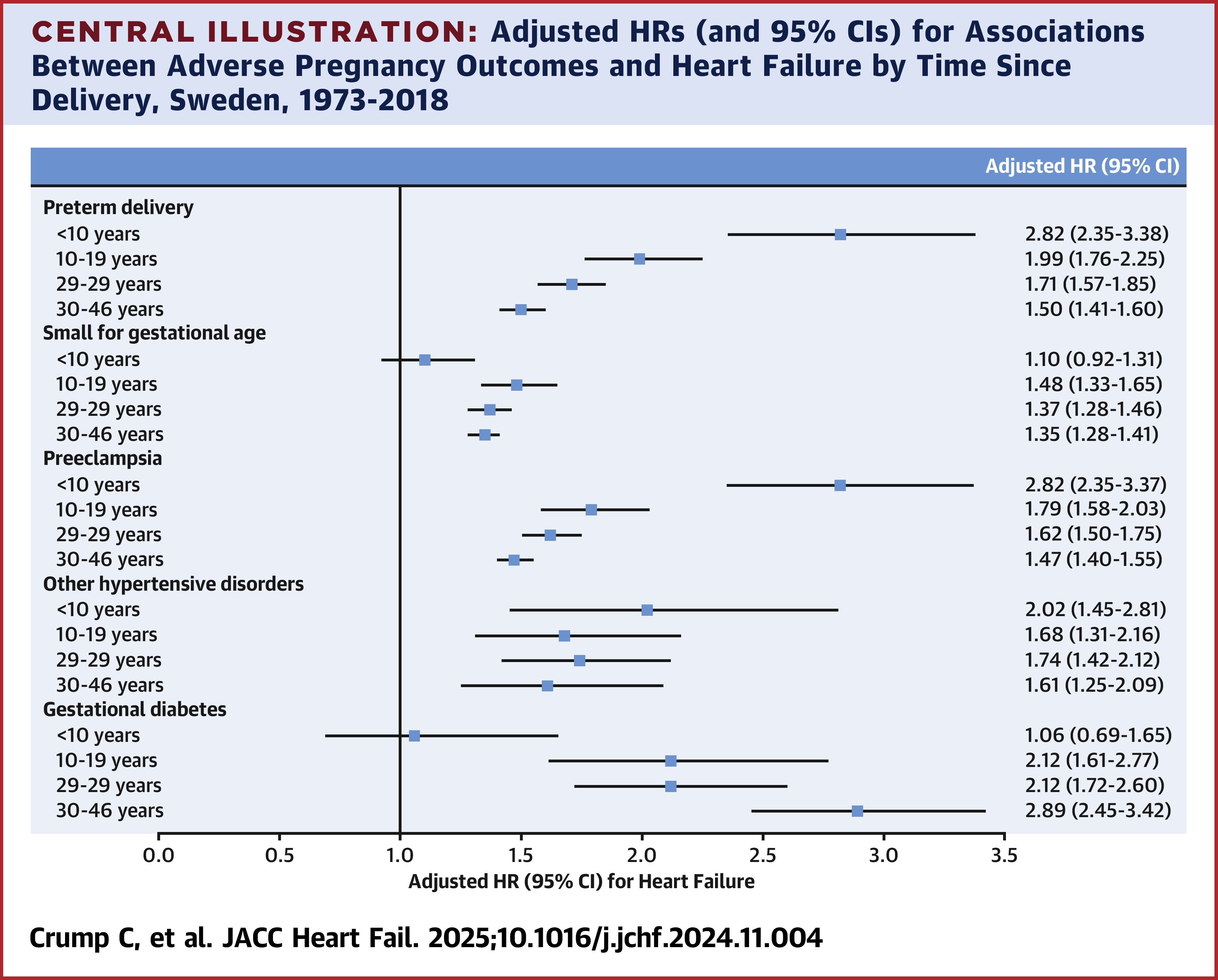
Additionally, the authors note that with up to 46 years of follow-up after delivery, adjusted hazard ratios (aHRs) for HF associated with specific adverse pregnancy outcomes were: gestational diabetes, 2.19; preterm delivery, 1.68; other hypertensive disorders, 1.68; preeclampsia, 1.59; and small for gestational age, 1.35. Furthermore, even 30 to 46 years after delivery, the risk remained significantly elevated (1.3-to 3.0-fold). Familial factors did not fully explain the findings.
The study also found that the risk of HF increased with the number of pregnancies, up to 46 years after delivery: the aHRs were 1.51, 2.31 and 3.18, respectively, for one, two or three pregnancies.
"All major adverse pregnancy outcomes should now be recognized as long-term independent risk factors for HF," write the authors. Early preventive actions and long-term clinical care are needed for the women who experience these adverse pregnancy outcomes to reduce their risk. Cardiovascular risk assessment in women should include their reproductive history.
In an accompanying editorial comment, Garima Sharma, MBBS, FACC; Tiffany Brazile, MD; and Sara A. Thorne, MD, write that, "Most importantly, identifying and engaging women who experience [adverse pregnancy outcomes] presents a valuable opportunity to initiate preventive care with timely postpartum follow-up and management of modifiable risk factors." They also highlight the need for more studies to understand the mechanisms "by which different [adverse pregnancy outcomes] result in various HF phenotypes have the potential to improve preventive care and reduce the incidence of these diseases."
Clinical Topics: Diabetes and Cardiometabolic Disease, Heart Failure and Cardiomyopathies, Prevention, Vascular Medicine, Acute Heart Failure, Hypertension
Keywords: Hypertension, Pregnancy-Induced, Diabetes, Gestational, Pregnancy Outcome, Pre-Eclampsia, Premature Birth, Heart Disease Risk Factors, Heart Failure
< Back to Listings

